The relationship between ABO blood group and cardiovascular disease: results from the Cardiorisk program
Introduction
The ABO blood group system consists of three main alleles [two co-dominant (A and B) and one recessive (O)] (1,2). The A and B alleles of the ABO locus encode A and B glycosyltransferase activities, which convert precursor H antigen into either A or B determinants, the A and B antigens having an extra saccharide unit to the O unit (N-acetylgalactosamine and galactose, respectively). Group O individuals lack such transferase enzymes and express basic, unchanged H-antigen (3). Notably, the ABO antigens are expressed not only on the surface of red blood cells but also on a variety of human cells and tissues, including epithelia, platelets, vascular endothelia and neurons (4). Therefore, it is reasonable to hypothesize that such carbohydrate moieties are of importance not only for transfusion and transplantation medicine, but also for the pathogenesis of various systemic diseases (5-9). Among these pathologies, the best clinical evidence emerged from the association between ABO antigens and cardiovascular disorders, as documented by a number of systematic reviews and meta-analyses (6,10-12). In this study, we assessed whether the ABO blood group correlates with the risk of developing clinical or subclinical cardiovascular disease in a homogeneous population of blood donors at the Department of Transfusion Medicine and Haematology (DMTE) of Mantova.
Materials and methods
Since January 2005, all blood donors aged between 35 and 65 years belonging to the Italian Association of Volunteers Blood Donors (AVIS) and donating at the DMTE of Mantova were enrolled in the program of cardiovascular primary prevention named Cardiorisk. This program, which was initially developed by the Transfusion and Immunohematology Center of the Polyclinic of Milan (13,14) on the basis of the CUORE project from the Italian National Institute of Health (15-17), was designed to calculate the risk of developing cardiovascular disease within subsequent 10 years. Eight parameters [sex, age, total cholesterol >200 mg/dL (5.17 mmol/L), high-density lipoprotein (HDL) cholesterol <40 mg/dL (1.03 mmol/L), plasma glucose >100 mg/dL (5.56 mmol/L), arterial systolic blood pressure >140 mm/Hg, anti-hypertensive therapy and smoking] were annually collected for each enrolled blood donor to generate a score which identified individuals at low-moderate (score <20) or high cardiovascular risk (score ≥20). Clinical and laboratory data collection as well as the calculation of the Cardiorisk score were performed using the regional software EmoNet (Insiel Mercato, Udine, Italy) for global management of transfusion services. Only blood donors with a minimum follow-up of at least 2 years were included in this study. All blood donors with a Cardiorisk score ≥20 were suspended from blood donation and underwent additional instrumental tests (chest X-ray, stress electrocardiogram and Doppler ultrasound of supra-aortic trunks). Those with normal results were readmitted, whereas the others were withdrawn from blood donation and referred to the treating physicians for follow-up or further specialist (cardiologist, vascular surgeon) evaluation for most appropriate treatment. Their follow-up was updated every 3 months in the software for the management of blood donors (EmoNet). The ABO blood group of all blood donors with a Cardiorisk score ≥20 during the period 2005–2015 was recorded and the distribution was compared with that of the group of blood donors with a Cardiorisk score >20. Statistical analysis was performed using Fischer’s Exact Test. A P value less than 0.05 was considered statistically significant. Descriptive data were presented as medians with range.
Results
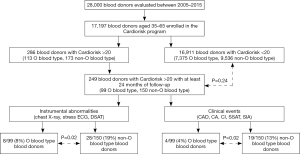
Among the 17,197 blood donors aged 35–65 years included in Cardiorisk program during the period 2005–2015, 286 had a Cardiorisk score >20, and 249 of them were evaluated having a follow-up of at least 24 months (median follow-up, 5.3 years; range, 2–10 years). All blood donors with Cardiorisk score ≥20 were males and their median age was 55 years (range, 35–65 years). Of these, 99 (39.8%) had O blood type while the remaining 150 (60.2%) had non-O blood type. Among the control group, represented by 16,911 consecutive blood donors with a Cardiorisk <20 (10,321 males and 6,590 females; median age at evaluation 47 years, range, 35–65 years), the ABO blood group distribution was the following: 7,375 (43.6%) O blood type and 9,536 (56.4%) non-O blood type. No statistically significant difference in ABO blood group distribution was present between the two groups of blood donors with Cardiorisk ≥ and <20 (P=0.2) (Table 1). Thirty-six of the 249 (14.5%) blood donors with a score ≥20 had at least one abnormal instrumental test result and their ABO status significantly differed from control group showing an excess of non-O blood types (77.8% in donors with Cardiorisk ≥20 and instrumental test abnormalities vs. 56.4% in blood donors with Cardiorisk <20, P=0.01) (Table 1). In addition, the prevalence of such abnormalities was markedly higher in non-O vs. O blood type subjects [28/150 (18.7%) vs. 8/99 (8.1%), P=0.02]. Twenty-three (9.2%) individuals developed also clinical cardiovascular events during the follow-up period (10 acute coronary syndrome, 2 cerebral ischemia, 3 cardiac arrhythmia, 8 stenosis of supra-aortic trunks or iliac arteries). Again, the non-O blood group distribution in such patients significantly differed from that of the control group with Cardiorisk <20 (82.6% vs. 56.4%, P=0.01), having non-O blood type subjects an increased risk of developing cardiovascular events compared with O blood type [19/150 (12.7%) vs. 4/99 (4.0%), P=0.02). Accordingly, non-O blood type subjects had a nearly 3-fold higher risk of developing cardiovascular events on follow-up compared to O blood type (crude odds ratio, 3.3; 95% CI, 1.1–10.1; P=0.033). Figure 1 summarizes the results of the study.
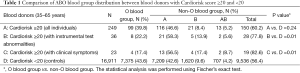
Full table
Discussion
The ABO blood group exerts a profound influence on hemostasis, being a key determinant of plasma concentrations of von Willebrand factor (VWF) and, consequently, of coagulation factor VIII (FVIII) (18,19). It is well known, indeed, that individuals with non-O blood group have circulating levels of both VWF and FVIII that are approximately 25% higher than O blood group subjects, and the underlying mechanism resides in the positive influence on VWF levels and activity of the addition of A and B antigens, by the specific glycosyltransferase enzymes, on the existing VWF H oligosaccharides (20). The non-O related increased levels of VWF and FVIII, in addition with those of several inflammatory cytokines (i.e., tumor necrosis factor-alpha, soluble intercellular adhesion molecule 1, E-selectin, P-selectin and interleukin-6) and cholesterol levels, have been suggested as the most likely mechanisms for explaining the association between ABO blood group and cardiovascular diseases (21-24). The close link between non-O blood type and cardiovascular risk emerges also from our study, which assessed for the first time the clinical impact of the Cardiorisk program in a large population of Italian blood donors. Indeed, while previous publications (13,14,25) limited their analysis to the epidemiological characteristics of blood donors stratified according to the Cardiorisk score, in the present study we followed such population to clinically validate the predictive risk of this program. Notably, all the blood donors with Cardiorisk ≥20 were males and their median age was higher than that of the general blood donor population (55 vs. 47 years), thus outlining the key role of sex and age in the atherosclerosis process. Since the distribution of the O and AB blood groups was found to have no association with the gender at our latitude (26), the prevalence of males observed in the population with Cardiorisk ≥20 has not seemingly influenced the outcome of our analysis. In addition, the observation that 14.5% and 9.2% of high-risk blood donors had a subclinical or clinical evidence of an underlying cardiovascular disease, respectively, further validates the utility of this primary cardiovascular prevention program in a large population such as that of blood donors. However, the most striking finding of our study was the strong correlation between the ABO status and the cardiovascular risk: indeed, among the blood donors identified as high risk by the Cardiorisk program (i.e., those with a score ≥20), those belonging to non-O blood type had a significantly increased incidence of cardiovascular adverse events compared with O blood type subjects. Our data are thus in keeping with previous investigations documenting the importance of ABO blood type in the pathogenesis not only of venous thromboembolism but also of arterial thrombotic process (10-12).
Conclusions
In conclusion we believe that, similarly to other scores evaluating the risk of developing acute occlusive arterial events (27,28), the ABO status should be incorporated also in the Cardiorisk score in order to better identify blood donors at higher risk of developing cardiovascular adverse events, and thus implementing preventive measures on modifiable risk factors.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the institutional ethic review board and informed consent was obtained from all patients.
References
- Yamamoto F, Clausen H, White T, et al. Molecular genetic basis of the histo-blood group ABO system. Nature 1990;345:229-33. [Crossref] [PubMed]
- Storry JR, Olsson ML. The ABO blood group system revisited: a review and update. Immunohematology 2009;25:48-59. [PubMed]
- Lowe JB. The blood group-specific human glycosyltransferases. Baillieres Clin Haematol 1993;6:465-92. [Crossref] [PubMed]
- Franchini M, Liumbruno GM. ABO blood group: old dogma, new perspectives. Clin Chem Lab Med 2013;51:1545-53. [PubMed]
- Liumbruno GM, Franchini M. Beyond immunohaematology: the role of the ABO blood group in human diseases. Blood Transfus 2013;11:491-9. [PubMed]
- Franchini M, Mannucci PM. ABO blood group and thrombotic vascular disease. Thromb Haemost 2014;112:1103-9. [Crossref] [PubMed]
- Franchini M, Lippi G. Relative Risks of Thrombosis and Bleeding in Different ABO Blood Groups. Semin Thromb Hemost 2016;42:112-7. [PubMed]
- Anstee DJ. The relationship between blood groups and disease. Blood 2010;115:4635-43. [Crossref] [PubMed]
- Franchini M, Favaloro EJ, Targher G, et al. ABO blood group, hypercoagulability, and cardiovascular and cancer risk. Crit Rev Clin Lab Sci 2012;49:137-49. [Crossref] [PubMed]
- Dentali F, Sironi AP, Ageno W, et al. ABO blood group and vascular disease: an update. Semin Thromb Hemost 2014;40:49-59. [PubMed]
- Wu O, Bayoumi N, Vickers MA, et al. ABO(H) blood groups and vascular disease: a systematic review and meta-analysis. J Thromb Haemost 2008;6:62-9. [Crossref] [PubMed]
- Dentali F, Sironi AP, Ageno W, et al. Non-O blood type is the commonest genetic risk factor for VTE: results from a meta-analysis of the literature. Semin Thromb Hemost 2012;38:535-48. [Crossref] [PubMed]
- Longo M, Lucci C, Marconi M, et al. Cross-sectional epidemiological study to evaluate the cardiovascular profile of a cohort of blood donors. Blood Transfus 2007;5:153-7. [PubMed]
- Longo M, Palmieri L, Marconi M, et al. A new setting of opportunistic cardiovascular screening: from blood donation to preventive cardiology. Preliminary results of the Cardiorisk program. G Ital Cardiol (Rome) 2010;11:578-83. [PubMed]
- Giampaoli S, Palmieri L, Panico S, et al. Favorable cardiovascular risk profile (low risk) and 10-year stroke incidence in women and men: findings from 12 Italian population samples. Am J Epidemiol 2006;163:893-902. [Crossref] [PubMed]
- Ferrario M, Chiodini P, Chambless LE, et al. Prediction of coronary events in a low incidence population. Assessing accuracy of the CUORE Cohort Study prediction equation. Int J Epidemiol 2005;34:413-21. [Crossref] [PubMed]
- Palmieri L, Donfrancesco C, Giampaoli S, et al. Favorable cardiovascular risk profile and 10-year coronary heart disease incidence in women and men: results from the Progetto CUORE. Eur J Cardiovasc Prev Rehabil 2006;13:562-70. [Crossref] [PubMed]
- Jenkins PV, O'Donnell JS. ABO blood group determines plasma von Willebrand factor levels: a biologic function after all? Transfusion 2006;46:1836-44. [Crossref] [PubMed]
- Song J, Chen F, Campos M, et al. Quantitative Influence of ABO Blood Groups on Factor VIII and Its Ratio to von Willebrand Factor, Novel Observations from an ARIC Study of 11,673 Subjects. PLoS One 2015;10:e0132626. [Crossref] [PubMed]
- Franchini M, Crestani S, Frattini F, et al. ABO blood group and von Willebrand factor: biological implications. Clin Chem Lab Med 2014;52:1273-6. [Crossref] [PubMed]
- Paré G, Chasman DI, Kellogg M, et al. Novel association of ABO histo-blood group antigen with soluble ICAM-1: results of a genome-wide association study of 6,578 women. PLoS Genet 2008;4:e1000118. [Crossref] [PubMed]
- Karakas M, Baumert J, Kleber ME, et al. A variant in the ABO gene explains the variation in soluble E-selectin levels-results from dense genotyping in two independent populations. PLoS One 2012;7:e51441. [Crossref] [PubMed]
- Paterson AD, Lopes-Virella MF, Waggott D, et al. Genome-wide association identifies the ABO blood group as a major locus associated with serum levels of soluble E-selectin. Arterioscler Thromb Vasc Biol 2009;29:1958-67. [Crossref] [PubMed]
- Chen Y, Chen C, Ke X, et al. Analysis of circulating cholesterol levels as a mediator of an association between ABO blood group and coronary heart disease. Circ Cardiovasc Genet 2014;7:43-8. [Crossref] [PubMed]
- Dell'anna P, Adorni D, Bernuzzi G, et al. Evaluation of cardiovascular risk in blood donors: results of the CARDIORISK study in the Parma Transfusion Service. Blood Transfus 2010;8:155-8. [PubMed]
- Mengoli C, Bonfanti C, Rossi C, et al. Blood group distribution and life-expectancy: a single-centre experience. Blood Transfus 2015;13:313-7. [PubMed]
- Yang N, Zhang B, Xie L, et al. The association baseline NIH Stroke Scale score with ABO blood-subtypes in young patients with acute ischemic stroke. Atherosclerosis 2014;236:144-9. [Crossref] [PubMed]
- Gong P, Luo SH, Li XL, et al. Relation of ABO blood groups to the severity of coronary atherosclerosis: an Gensini score assessment. Atherosclerosis 2014;237:748-53. [Crossref] [PubMed]


