Mental health issues amongst medical students in Asia: a systematic review [2000–2015]
Introduction
One of the main functions of medical schools is to train physicians to meet the healthcare needs of current and future national populations (1,2). This is usually achieved through arduous training curriculum and programmes in which high levels of motivation, intelligence and stamina are expected. In fact, the total expanse of professional knowledge and skills acquired by medical students is greater than that of students from other majors (3,4). This is exacerbated by the fact that individuals aged between 18–24 years of age are particularly at risk of developing mental disorders such as major depressive disorder (MDD), anxiety disorders (ADs) and psychiatric comorbidity (5-7). As a consequence, stress levels and the extent of emotional disturbances amongst medical students is high (8-10). Studies have also shown that mental health problems are higher amongst university students as compared to their peers (11-13). Despite this, the prevalence of such mental disorders amongst universities students continues to rise (14-16).
Mental disorders and distress can result in numerous undesirable personal and professional consequences which include burnout, social isolation, growing cynicism and eventual physician impairment (17-19). At times, mental health issues may persist into adulthood if they remain undetected or are not treated appropriately (20). Furthermore, undesirable coping mechanisms such as substance abuse, alcohol consumption, smoking and harm to self and others may be observed in mentally and emotionally distressed medical students.
Within Asia, there are numerous medical education systems (21). Initially having adopted their traditional education systems from their previous Western colonial leaders such as the United Kingdom, the US, Netherlands and France, there have been significant medical education reforms within Asian countries so as to prepare physicians to meet the unique cultural and healthcare needs of local communities within the continent (22,23). As such, the current state of medical education in Asia differs in certain areas compared to Western medical education. Thus, the different curricula place separate demands and expectations upon medical students. This may potentially result in distinct incidence and prevalence statistics of mental health issues amongst medical students in Asian medical schools.
Objective
Two previous systematic reviews done with papers from the United States of America (USA), and the United Kingdom (UK) and other English-speaking countries respectively, showed that North American and other medical students are more depressed and anxious than their peers. However there is a dearth of research synthesis focusing solely on Asian medical students (8,24). Consequently, the objective of this study is to perform a systematic review of papers that have studied mental health issues amongst Asian medical schools so as to identify the prevalence of mental health problems amongst medical students within Asia. We hope that the synthesised information obtained can bring to light the severity of mental health issues within Asian universities, and consequently result in psychological interventions within universities so as to improve the mental health of medical students.
Methods
Identification of studies
Our study focused on the incidence and prevalence of mental health issues in Asian medical schools. A broad search string (((medical student) OR medical school) AND mental AND Asia) was used in Medline, Embase/Scopus, and SpringerLink.
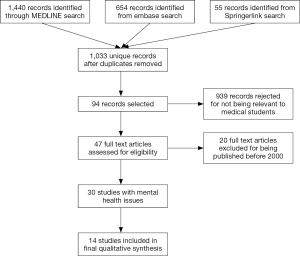
A total of 1,033 unique records were obtained and their titles and abstracts were reviewed in order to exclude irrelevant studies; articles in English and with sufficiently detailed English abstracts were included, articles not related to medical school or medical students were excluded. Potentially relevant abstracts were assessed and relevant articles were downloaded and their entire texts assessed. The references cited by each potentially relevant paper and papers suggested by databases, such as Elsevier, were also assessed for relevance; 94 potentially relevant abstracts were assessed and 47 full text articles downloaded (Figure 1).
Included studies
Thirty studies written in English and published between January 2000 till February 2015, reported primary data on the incidence and prevalence of mental disorders (according to various diagnostic criteria, such as the Beck Depression Inventory or Beck Anxiety Inventory) from a population or sub-population of medical students in Asian countries (25,26). Out of these 30 studies, 14 were included in the final qualitative synthesis.
Data extraction
Once a study was included, the data relevant to the study-level variables (first author, year of publication, country of study, diagnostic criteria) were noted. The studies were then given points according to the Joanna-Briggs Institute Prevalence Critical Appraisal Tool for rate-related variables (27). Two independent authors (ANC and AAS) assessed all the selected papers used in this analysis and disagreements were resolved by consensus. Studies were included for (qualitative synthesis) if there was a consensus between the two authors if the number of points (‘Yes’) were more than 6 out of 10 points.
Results
Fourteen full text articles, with 13,111 participants, were included in this study. This systematic review focused on depression, anxiety, common coping mechanisms, body dysmorphic disorders and its associated eating disorders, and suicidal ideations among medical students. The assessment tools used in each study are compiled in Table 1.
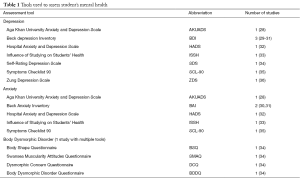
Full table
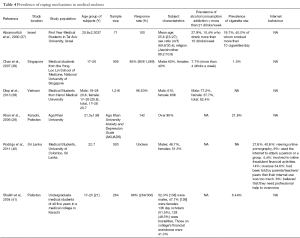
Nine studies (Table 2) evaluated depression among medical students, with an aggregate prevalence of 11.0%. ADs had an aggregate prevalence of 7.04%, based on data from six studies (Table 3). Coping mechanisms in the form of alcohol use, cigarette smoking and problematic Internet behaviors were discussed in 3, 4 and 1 study respectively (Table 4). One study and its 2-year follow-up included body dysmorphic disorder and disordered eating attitudes among medical students, but the prevalence for both of these issues was low, 1% and 2% respectively (Table 5). The prevalence of suicidal ideations was reported in one study, with 3% of medical students having such ideations (Table 6); none of the students were reported to have attempted suicide in the study.
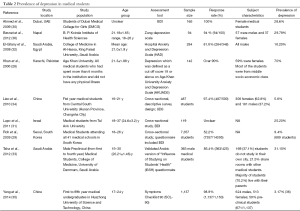
Full table
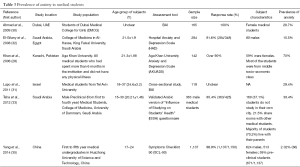
Full table
Full table

Full table

Full table
Depression
Data on depression was found in 9/30 studies, with a pooled prevalence of 11.0% (1,115/10,147) of students. Students were screened for depression using seven different tools (Table 1). The nine studies were from East Asia, South Asia and the Middle East (28-36).
Two studies categorized depression based on gender, showing no significant difference between the prevalence for male and female students, 12.9% (54/420) and 12.9% (41/319) for male and female medical students respectively.
The odds of preclinical students having being screened for depression was 1.63 times higher compared to clinical students. A total of 98.0% (48/49) of pre-clinical students were screened for depression, compared to 60% (27/45) clinical students. Home staying medical students had a 1.33 times higher odds to be depressed compared to hostel-stayers, with 12.1% (29/239) of home stayers being depressed compared to 9.2% (37/402) of hostel stayers.
Anxiety
Data on ADs was found in 6 studies with a pooled prevalence of 7.04% (100/1,420) (28,30-33,35). Five different tools were used to assess anxiety. There were no significant differences in prevalence between genders for anxiety.
Coping mechanisms
Alcohol use was prevalent in 38.7% (849/2,196) of students and cigarette smoking, was prevalent in 5.5% (76/1,386) of students in the included studies (28,37-39,41). One study in Vietnam compared the difference in alcohol use between male and female students (39). Male students had a 2.02 times higher odds to consume alcohol compared to female students. There was no significant difference in genders among students who smoked cigarettes.
Problematic internet behavior was noted in 27.3% (139/503) of students in a study done in Sri Lanka (40). The behaviors ranged from online pornography, fraudulent financial transactions, cyber attacks and overuse of internet. A total of 40.6% of these students admitted to viewing and downloading online pornography, 6% had used it for cyber attacks and 4.4% had been involved in some form of online fraudulent activity. A total of 6% of these students believed that they needed professional help to overcome their behaviors.
Body dysmorphic disorders
A study done by among first year medical students from Central South University (Hunan Province, Changsha City) in 2006 using the Body Shape Questionnaire (BSQ), Dysmorphic Concern Questionnaire (DCQ) and Body Dysmorphic Disorder Questionnaire (BDDQ) (34). One third of students showed a concern with some aspect of their physical appearance, measured by the BDDQ, however only 5 students out of 486, screened positive for body dysmorphic disorder; where they spent a significant portion of time every day pre-occupied with the appearance of a body part.
A third of the sample was concerned with some aspect of their physical appearance (as measured by BDDQ)—this finding is markedly lower than rates reported in other studies although the inclusion of weight-related concerns with their appearance screened positive for BDD in our study. The most significant correlates of dysmorphic concern for males were scores on the SIAS (anxiety) (P<0.001) and SDS (depression) (P<0.001). For females, the most significant correlates of dysmorphic concern were scores on the BSQ (body shape) (P<0.001), SDS (P<0.001) and SIAS (P<0.05).
Suicidal ideation
One study in the UAE reported 3% prevalence of suicidal ideation in medical students. This can be compared to a study in the United States with a prevalence of 20.4% (30,42). None of the students in the study attempted suicide.
Discussion
Medical school is a highly demanding phase in a student’s medical career where a lot is expected from students due to the course content and duty hours in the curricula. In addition to coping with normal stressors in life, medical students have to cope with the amount complexity of the medical knowledge they learn, the financial debt that they sometimes have to take up, the lack of leisure time compared to their peers and having to make career choices at the end of medical school (28).
This systematic review showed that medical students in Asia are prone to mental health issues, with 52.7% of students citing significant stress as one of the issues that they faced in medical school.
Depression
A systematic review on undergraduate students showed that the global prevalence for depression among undergraduate students was 33% (43). While depression had a pooled prevalence of 11% in this systematic review, 5 of the studies done in the Middle East and South Asia had incidence of depression near or higher than 30% (28,29,31,33,36). This fitting with the prevalence of depression found in the undergraduates in general as well as the 2 other systematic reviews of medical students’ mental health issues (8,24). The study in Pakistan had a 70% incidence of depression in its cohort (28). This prevalence of depression in these studies could be due to cultural and social reasons, as a similar study done in Pakistan before 2000 had similar rates of depression, stating that terrorism and political instability had a role to play in the mental health issues faced by medical students (44). Three reasons could be given for the low pooled prevalence, the first being underreporting in certain studies as some Asian cultures do not view mental health issues favorably, and thus students might be unwilling to report certain issues which they face (34). However a second reason is that medical students obtain relevant knowledge in psychiatry and medical psychology during their clerkships and hence they know more about self-psychological management (35). Thirdly, this low prevalence could also be due to good support by medical schools (35), where the schools have improved their focus on students’ mental health education as well as engaging psychological counselors to help students who have mental health issues (35).
Anxiety
While the pooled prevalence of anxiety was 7.04%, there was a study in China with a prevalence of 2.02% (35). The rest of the studies from the Middle East and South Asia had prevalences from 15.5–70% (28-30,32). Like depression, this low prevalence in China was associated with medical students having more knowledge compared to their other undergraduate contemporaries as well as schools being more prepared to cope with students’ mental health issues by engaging psychological counselors to help students.
Suicidal ideation
The study on suicidal ideations noted that students in the UAE, while they did have ideas of suicide, did not attempt suicide due to religious reasons. A study in Sweden showed a 2.8% suicide attempt rate among medical students (45). It is thus relevant to note that Asian students’ religions might preclude them from acting on these suicidal ideations.
Strengths
One of the biggest strengths of this study would be the fact that the overall sample size was large covering a total of 13,111 participants from various regions in Asia, from East to South Asia and the Middle East. This number of participants is comparative to the previous systematic reviews done in other regions. Furthermore the study focussed on newer studies published after 2000, thus being more applicable for current medical students.
Limitations
We noted certain limitations to our systematic review. Firstly, due to the lack of sufficient data within the current literature, we were unable to perform a quantitative meta-analysis of the various risk factors which could explain the mental health issues amongst medical students. Apart from that, there were certain limitations to the scales used by the various studies included within our systematic review. While the Beck’s Depression and Anxiety indexes are validated tools for making the diagnosis of depression and anxiety, certain studies used different cut-off values for diagnosing these mental health issues, thus this would result in differing prevalences seen in the different studies. However the BDI was used in only three studies and the BAI in 2, hence reducing the extent of this limitation.
In addition to the depression and anxiety scores, the data for the prevalence of body dysmorphic disorder and eating disorders might be limited by the self-reporting nature of the tools, such as the BDDQ, thus leading to either an over- or under-estimation of the actual incidence of such disorders and hence more studies should be done to find out more about how medical students are affected by these issues.
Conclusions
Mental health issues affect a significant proportion of medical students in Asia. While the prevalence of depression and anxiety are lower than global values, the high levels of motivation, intelligence and stamina expected of medical students can result in undesirable personal and professional consequences which can cause eventual physician impairment. Studies have shown that medical students’ knowledge in mental health issues as well as schools’ support through psychological intervention results in these lower prevalence rates compared to undergraduate students. More research should be done regarding this issue. With such information, it is hoped that appropriate interventions can be designed to improve the mental health of medical students.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Schofield JR, editor. New and Expanded Medical Schools: Mid-Century to the 1980s. San Francisco: Jossey-Bass, 1984.
- Mullan F, Chen C, Petterson S, et al. The social mission of medical education: ranking the schools. Ann Intern Med 2010;152:804-11. [PubMed]
- Bond AR, Mason HF, Lemaster CM, et al. Embodied health: the effects of a mind-body course for medical students. Med Educ Online 2013;18:1-8. [PubMed]
- O'Rourke M, Hammond S, O'Flynn S, et al. The Medical Student Stress Profile: a tool for stress audit in medical training. Med Educ 2010;44:1027-37. [PubMed]
- Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004.21-7. [PubMed]
- Patten SB. Major depression prevalence in Calgary. Can J Psychiatry 2000;45:923-6. [PubMed]
- Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med 1998;28:109-26. [PubMed]
- Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med 2006;81:354-73. [PubMed]
- Tyssen R, Vaglum P, Grønvold NT, et al. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord 2001;64:69-79. [PubMed]
- Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ 2005;39:594-604. [PubMed]
- Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol 2008;43:667-72. [PubMed]
- Stewart-Brown S, Evans J, Patterson J, et al. The health of students in institutes of higher education: an important and neglected public health problem? J Public Health Med 2000;22:492-9. [PubMed]
- Tomoda A, Mori K, Kimura M, et al. One-year prevalence and incidence of depression among first-year university students in Japan: a preliminary study. Psychiatry Clin Neurosci 2000;54:583-8. [PubMed]
- Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety 1998;7:3-14. [PubMed]
- Gallagher RP, Gill AM, Sysco HM, editors. National Survey of Counseling Centre Directors 2000. Alexandria, VA, USA: International Association of Counseling Service, 2000.
- Benton SA, Robertson JM, Tseng W, et al. Changes in counseling center client problems across 13 years. Professional Psychology: Research and Practice 2003;34:66-72.
- Crandall SJ, Volk RJ, Loemker V. Medical students' attitudes toward providing care for the underserved. Are we training socially responsible physicians? JAMA 1993;269:2519-23. [PubMed]
- Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: a cohort study. Med Educ 2004;38:522-34. [PubMed]
- Notman M, Nadelson C. Adaptation to stress in physicians. In: Shapiro E, Lowenstein L, editors. Becoming a Physician: Development of Values and Attitudes in Medicine. Cambridge, MA: Ballinger, 1979:201.
- Pine DS, Cohen P, Gurley D, et al. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 1998;55:56-64. [PubMed]
- Tan CH, Amin Z, Khoo HE, et al. Student perceptions of the benefits of problem-based learning. Med Teach 2007;29:284. [PubMed]
- Lam TP, Lam YY. Medical education reform: the Asian experience. Acad Med 2009;84:1313-7. [PubMed]
- Majumder AA, D'Souza U, Rahman S. Trends in medical education: challenges and directions for need-based reforms of medical training in South-East Asia. Indian J Med Sci 2004;58:369-80. [PubMed]
- Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ 2014;48:963-79. [PubMed]
- Beck AT, editor. Depression: Causes and Treatment. Philadelphia: University of Pennsylvania Press, 1972.
- Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-7. [PubMed]
- The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual 2014. Copyright © The Joanna Briggs Institute 2014.
- Khan MS, Mahmood S, Badshah A, et al. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J Pak Med Assoc 2006;56:583-6. [PubMed]
- Roh MS, Jeon HJ, Kim H, et al. Factors influencing treatment for depression among medical students: a nationwide sample in South Korea. Med Educ 2009;43:133-9. [PubMed]
- Ahmed I, Banu H, Al-Fageer R, et al. Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care 2009;24:e1-7. [PubMed]
- Lupo MK, Strous RD. Religiosity, anxiety and depression among Israeli medical students. Isr Med Assoc J 2011;13:613-8. [PubMed]
- El-Gilany AH, Amr M, Hammad S. Perceived stress among male medical students in Egypt and Saudi Arabia: effect of sociodemographic factors. Ann Saudi Med 2008;28:442-8. [PubMed]
- Taha AZ, Sabra AA. Perceived Stresses among Male Students in University of Dammam, Eastern Saudi Arabia: A Comparative Study. J Am Sci 2012;8:291-8.
- Liao Y, Knoesen NP, Deng Y, et al. Body dysmorphic disorder, social anxiety and depressive symptoms in Chinese medical students. Soc Psychiatry Psychiatr Epidemiol 2010;45:963-71. [PubMed]
- Yang F, Meng H, Chen H, et al. Influencing factors of mental health of medical students in China. J Huazhong Univ Sci Technolog Med Sci 2014;34:443-9. [PubMed]
- Basnet B, Jaiswal M, Adhikari B, et al. Depression among undergraduate medical students. Kathmandu Univ Med J (KUMJ) 2012;10:56-9. [PubMed]
- Abramovitch H, Schreier A, Koren N. American medical students in Israel: stress and coping--a follow-up study. Med Educ 2000;34:890-6. [PubMed]
- Chan GC, Kohm D. Understanding the psychosocial and physical work environment in a Singapore medical school. Singapore Med J 2007;48:166-71. [PubMed]
- Diep PB, Knibbe RA, Giang KB, et al. Alcohol-related harm among university students in Hanoi, Vietnam. Glob Health Action 2013;6:1-10. [PubMed]
- Rodrigo C, Ranasinghe N, Wijayaratne D, et al. Problematic internet behaviours among university students in Sri Lanka. Asian J Psychiatr 2012;5:275-6. [PubMed]
- Shaikh BT, Kahloon A, Kazmi M, et al. Students, stress and coping strategies: a case of Pakistani medical school. Educ Health (Abingdon) 2004;17:346-53. [PubMed]
- Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health 2005;53:219-24. [PubMed]
- Sarokhani D, Delpisheh A, Veisani Y, et al. Prevalence of Depression among University Students: A Systematic Review and Meta-Analysis Study. Depress Res Treat 2013;2013:373857.
- Toews JA, Lockyer JM, Dobson DJ, et al. Analysis of stress levels among medical students, residents, and graduate students at four Canadian schools of medicine. Acad Med 1997;72:997-1002. [PubMed]
- Firth J. Levels and sources of stress in medical students. Br Med J (Clin Res Ed) 1986;292:1177-80. [PubMed]