Childhood colon cancer in a patient with ataxia telangiectasia
Introduction
Ataxia-telangiectasia (AT) is a rare autosomal recessive disease characterized by progressive neurologic impairment and cerebellar ataxia, which is also called as Louis-Bar syndrome (1,2). It correlates with variable immunodeficiency, especially for sinopulmonary infections (1,3). Ocular and cutaneous telangiectasia are other characteristics of this disease. In addition, patients with this disease have an inherent increased susceptibility to the development of cancer, predominantly hematologic malignancies (2,4). A hypersensitivity to X-rays seems to be relevant to the pathogenesis of malignancy in AT. The patients’ X-ray exposure dosage is positively correlated with their risk of cancer (5). We report the case of a young patient with AT who presented with bowel obstruction and was diagnosed with colon cancer.
Case presentation
A 16-year-old Russian boy was admitted to the hospital after having abdominal pain for 2 months. He was diagnosed with AT at the age of 10, and had a family history of AT. He has been treated for this disease with immunoglobulin injections in Russia. The patient underwent an examination in a Russian hospital for abdominal pain, during which a large mass obstructing the lumen of the colon was detected, and he was referred to our hospital for additional evaluation and treatment.
At initial presentation, the patient had normal vital signs, but he had general dystonia and could not walk normally. He had to use a wheel chair for ambulation and was unable to move around on his own. Moreover, because his legs were twisted to the right, he was unable to lie down straight and had to always lie on his side. He had multifocal vascular dilatations on his sclera (Figure 1).

The patient’s vital signs were stable at admission: blood pressure was 120/70 mmHg, pulse rate 80/min, body temperature 36.5 °C, and respiration rate 15/min.
Serum levels of hemoglobulin were 10.0 g/dL, white blood cell count 12,870/L, and platelet count 710,000/L. Aspartate aminotransferase was 23 IU/L, alanine aminotransferase 31 IU/L and albumin 3.6 g/dL. The glucose level was 95 mg/dL, blood urea nitrogen 14.0 mg/dL and creatinine 0.65 mg/dL. Na was 140 mmol/L, K 4.1 mmol/L, and Cl 102 mmol/L. C reactive protein was slightly increased to 1.29 mg/dL. Prothrombin time was 12.6 s, and activated partial thromboplastin time 28.7 s. Tumor markers were increased, with carcinoembryonic antigen at 20.6 ng/mL, and alpha-fetoprotein at 297 ng/mL. Tissue transglutaminase immunoglobulin A antibodies were markedly decreased to 3 mg/dL. Other immunoglobulin levels were in the normal range: IgG was 1,293.4 mg/dL, IgM 346.4 mg/dL, IgD 0.27 mg/dL, and IgE 0.1 IU/mL.
Since it is reported that exposure to radiation can speed up the progression of malignancy in AT patients, we made an effort to minimize radiological examination for this patient (5). However, a computed tomography (CT) scan had been performed in Russia, which revealed concentric wall thickening of the transverse colon, a relatively long segment that measured a maximal 2.1 cm in thickness (Figure 2). There were no detectable enlarged lymph nodes in the mesentery. Based on these findings alone, it was difficult to distinguish between lymphoma and colon cancer.
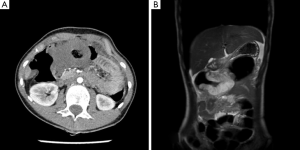
Abdominal ultrasonography was performed at our hospital to reduce the exposure to radiation and the findings showed the same concentric wall thickening in the transverse colon that was seen on the CT scan, and again, it was determined that distinguishing between lymphoma and colon cancer was difficult based solely on the diagnostic imaging results. There were no remarkable findings in the liver, gallbladder, visible pancreas, spleen, and both kidneys on ultrasonography.
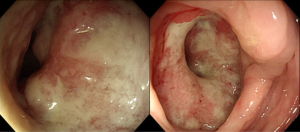
Colonoscopic examination showed a huge ulcerative fungating mass covered with thick mucous material. The lesion was hard and nearly totally obstructed the lumen of the transverse colon. The colonoscope could not be advanced into the proximal part of the colon through this site (Figure 3).
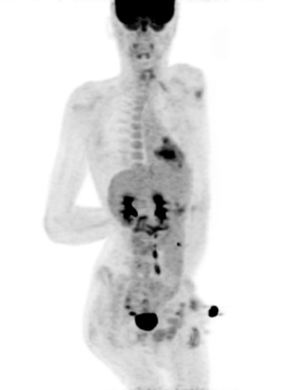
A positron emission tomography (PET) scan showed a fluorodeoxyglucose (FDG)-avid lesion in the transverse colon that was compatible with colon cancer without any definite evidence of metastasis. However, there were small amounts of ascites in the perihepatic space, and there seemed to be peritoneal carcinomatosis (Figure 4).
A biopsy was performed from ulcerative mass where located at 45 cm from the anal verge. On immunohistochemistry, it was negative for Cytokeratin 7 (CK7), and diffusely positive for Cytokeratin 20 (CK20) and CDX2. The result was consistent with adenocarcinoma of lower gastrointestinal (GI) tract origin. Therefore, the pathologist concluded that it was an adenocarcinoma with predominantly signet ring cell features (Figure 5A).
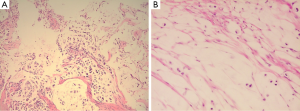
The patient underwent surgery for curative resection of the colon cancer. However, multiple nodular lesions were found in the peritoneal cavity and omentum. The frozen biopsy revealed metastatic signet ring cell carcinoma from the colon (Figure 5B).
Two weeks later, a self-expandable metal stent was inserted in order to relieve the symptoms of obstruction. The patient was discharged after several days and returned home to Russia.
Discussion
AT is a rare autosomal recessive immunodeficiency disease caused by an AT gene mutation. It has a wide range of clinical features, including progressive truncal ataxia, oculocutaneous telangiectasias, bronchopulmonary infections, cancer predisposition, and radiation sensitivity (1,2,5,6). Telangiectasia develops mainly on the conjunctiva, but it can also develop in areas exposed to friction. Insulin resistant diabetes and liver function abnormalities may also occur. There is some immunity impairment in this disease, including cell-mediated and humoral immunity. Patients with this disease have decreased levels of IgA, and have a high incidence of sinopulmonary infections (3). The life span of patient with AT likely to have been prolonged by antibiotics and regular injection of immunoglobulins. This Russian boy also has been injected immunoglobulin in monthly basis. The median age at death is reported to be approximately 20 years. There is report that the longest survival in patient with AT is 34 years (7). The mutated gene causing AT is called ataxia telangiectasia mutated (ATM) gene that has been localized to band 11q22-23. It is a member of a family of phosphatidylinositol-3-kinase related gene involved in cell cycle control and DNA damage response, and it is also associated with increased susceptibility to the development of cancer, approximately 100-fold in comparison to the general population (8). The most common types of malignancies are non-Hodgkin’s lymphoma and leukemia (64%), other solid tumors (26%), and Hodgkin’s disease (10%) (2,4). Adenocarcinoma is a relatively uncommon form of cancer in patients with AT. There have been a few cases of gastric cancer reported in young patients with AT, which had been diagnosed as adenocarcinoma with signet ring cell components from biopsy results. Although most of these patients presented with obstruction of the gastric outlet as the primary symptom, some had a chief complaint of non-specific abdominal pain and nausea, and most of the patients were young, between the ages of 14–26 years (5,9,10).
Even if the patient with AT could have solid tumor such as stomach cancer or breast cancer, it is less likely to have colon cancer, especially signet ring cell type. Actually, no case of colon cancer has ever been reported, especially in young patient and hence, we have focused on this point and are hereby reporting this unique case.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Frais MA. Gastric adenocarcinoma due to ataxia-telangiectasia (Louis-Bar syndrome). J Med Genet 1979;16:160-1. [PubMed]
- Lohmann E, Krüger S, Hauser AK, et al. Clinical variability in ataxia-telangiectasia. J Neurol 2015;262:1724-7. [PubMed]
- Murphy RC, Berdon WE, Ruzal-Shapiro C, et al. Malignancies in pediatric patients with ataxia telangiectasia. Pediatr Radiol 1999;29:225-30. [PubMed]
- Tomioka H, Kaneoya A, Mochizuki Y, et al. Primary Diffuse Large B-cell Lymphoma Arising in the Tongue Accompanied by Ataxia-telangiectasia: A Case Report. J Clin Diagn Res 2015;9:ZD25-7. [PubMed]
- Otabor IA, Abdessalam SF, Erdman SH, et al. Gastric outlet obstruction due to adenocarcinoma in a patient with Ataxia-Telangiectasia syndrome: a case report and review of the literature. World J Surg Oncol 2009;7:29. [PubMed]
- Patiroglu T, Eke Gungor H, Arslan D, et al. Gastric signet ring carcinoma in a patient with ataxia-telangiectasia: a case report and review of the literature. J Pediatr Hematol Oncol 2013;35:e341-3. [PubMed]
- Opeskin K, Waterston J, Nirenberg A, et al. Ataxia telangiectasia with long survival. J Clin Neurosci 1998;5:471-3. [PubMed]
- Su Y, Swift M. Mortality rates among carriers of ataxia-telangiectasia mutant alleles. Ann Intern Med 2000;133:770-8. [PubMed]
- Swift M, Morrell D, Massey RB, et al. Incidence of cancer in 161 families affected by ataxia-telangiectasia. N Engl J Med 1991;325:1831-6. [PubMed]
- Teive HA, Moro A, Moscovich M, et al. Ataxia-telangiectasia - A historical review and a proposal for a new designation: ATM syndrome. J Neurol Sci 2015;355:3-6. [PubMed]


