Electric vs. harmonic scalpel in treatment of primary focal hyperhidrosis with thoracoscopic sympathectomy
Introduction
Thoracoscopic sympathectomy is nowadays well established one-day surgical procedure, with very good postoperative results (1,2). Patients are able to continue their everyday activities even the next day of the operation with adequate analgesics if necessary. One of the conditions for early returning to the every-day activities after the operation is absence of pain (3).
As a standardized minimal invasive operation, thoracoscopic sympathectomy is today performed through one to three incisions in diameter from 3-10 mm so the pain after this operation, is related to periosteal lesions over the ribs and under the sympathetic chain, as well as from transmission of heat in surrounding tissue.
Intraoperative complications during the thoracoscopic sympathectomy such as pneumothorax, hematothorax occurs in less than 5% patients, or the most serious Horner syndrome, occurs in less than 1% of the patients (4).
On the other side, technical details during the operation, such as smoke in pleural cavity which can diminish the visibility and linger the operation, or lateral thermal tissue damage, especially Stellate ganglion, can adduce surgeon to use electric or harmonic scalpel (1,5).
Pain is recognized to be a major source of postoperative morbidity and some degree of pain may still afflict up to 63% of patients after video thoracoscopic procedures (6).
The objective of this study is to compare severity of pain in group of patients treated with electric scalpel and the group of patients treated with harmonic scalpel.
Patients and methods
This was a retrospective uncontrolled study. From January 2008 to December of 2009 bilateral thoracoscopic sympathectomy Th2-Th4 was performed to 79 patients aged from 17 to 55, who suffered from palmar, axillar or craniofacial hyperhidrosis. All the patients were treated by the same surgical team in the same hospital with standardized surgical procedure. For the first 39 patients (group A) thoracoscopic sympathectomy was performed using electric scalpel and for the next 40 patients (group B) thoracoscopic sympathectomy was performed using harmonic scalpel.
Criteria for the operation were: primary focal hyperhidrosis (palmar, axillar or craniofacial), absence of previous thoracic surgical procedures, rib fractures, massive pneumonia or pleural empyema, good respiratory function and coagulation.
Exclude criteria for the operation were: generalized hyperhidrosis, hyperthyroidisms, diabetes mellitus, tuberculosis, menopause, bradycardia (<40/min), alcoholism or drug abuse. Six months after the operation, patients were asked to fill in the questionnaire about quality of life before and after the operation, using the hyperhidrosis disease severity scale (HDSS) (7), the location and existence of pain using evaluating scale from 0 to 10 where 0 represented no pain, 1-4 slight pain, 5-8 moderate pain and 9-10 severe pain, based on their own estimates, without intervention or advise form the interviewer.
Statistical analysis
The chi-square test and independent-samples t-tests were used to analyze the results between two groups through SPSS 11.0 for windows (SPSS Inc., IL, USA). A P value less than 0.05 was considered statistically significant.
Surgical procedure
In both groups, the operative procedure was performed in the same fashion. Patients were positioned in the lateral decubitus, with a roll pillow at the level of the scapula peak to additionally extend the intercostal spaces. Intraoperative monitoring included arterial blood pressure, electrocardiography and pulse oximetry. After intubation with double lumen endotracheal tube, having the lung on the operative side collapsed, the following instruments were introduced into the pleural space through two 5-mm operating ports (Aesculap, Tuttlingen, Germany): videothoracoscopic camera (Telescope Aesculap 5 mm 00, Tuttlingen, Germany) which was connected to the video data processing system (Richard Wolf 3CCD Camera System, Tuttlingen, Germany), electric or harmonic scalpel (Auto Sonix-Hook Probe; Auto Sonix-Ultrasonic Surgical System Tyco, International Health Care). Skin incisions were made through the third intercostal space in the middle axillary line and through the fifth intercostal space in the posterior axillary line. The patient was then rotated to allow gravity to retract the lung away from the surface of the spine.
Having identified the first rib and the sympathetic chain, it was transected by electric or harmonic scalpel over the second, third and fourth rib head. After that, the parietal pleura was resected over the body of the second and third rib, starting from the costovertebral angle onto the lateral direction, in the length of 4-5 cm, cutting off the possible accessory sympathetic nerves (Kuntz fibers). The surgery ended by introducing a single chest tube No 16F connected to the active suction of −20 cm H2O. Skin incisions were closed with tissue glue (Histoacryl). The patient was then repositioned, and the same surgical procedure was performed on the opposite side.
Having obtained the radiological verification of the pulmonary parenchyma re-expansion, the chest tubes were removed on the 0th and 1st postoperative day and patients were discharged from the hospital. Postoperatively, orally administered analgesics (paracetamol or NSAIL) were adequate for pain control.
Results
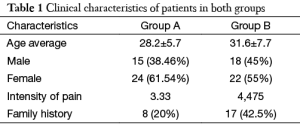
All patients successfully underwent bilateral thoracoscopic sympathectomy with electric or harmonic scalpel and no death or conversion to open surgical procedures occurred in either group. Neither bradycardia nor Horner’s syndrome was encountered. General demographics were similar in both groups (Table 1)
Full table
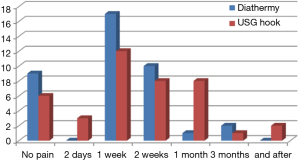
There has been no differences in occurrence and duration of postoperative pain in both groups (Figure 1) and no statistically significant difference between electric and harmonic scalpel (P>0.05). The majority of patients from both groups (69.2% from group A and 50% from group B) claim that pain lasted 1-2 weeks. Two patients from group B claims that they have pain after 6 months, and 23% patients from group A and 15% patients from group B have no pain after the operation.
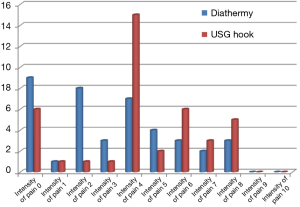
Intensity of postoperative pain was similar in both group (Figure 2) and majority of the patients measured their postoperative pain as slight pain- evaluating scale 4 (17.9% patients from group A and 37.5% patients from group B). It can be noticed that some patients from group B measured their pain as moderate (evaluating scale 6-8). After statistical analysis of the results, there is a statistical difference of the intensity of postoperative pain between two group (P<0.05) but, the deviations are minimal (P=0.04).
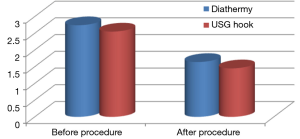
There was a significant difference in of quality of life (using HDSS) before and after the thoracoscopic sympathectomy in both groups of patients (Figure 3). Patients from group A estimate their quality of life as 2.74 average, and patients from group B 2.55 which emphasize their everyday problems with hyperhidrosis. After the operation the significant improvement of quality of life has been seen in both groups of patients, for group A it was 1.64 and for group B it was 1.45. There was no statistical difference for quality of life in both groups comparing electric and harmonic scalpel (P>0.05).
Discussion
Thoracoscopic sympathectomy is considered today a highly effective minimal invasive surgical procedure in the treatment of primary palmar, axillar and craniofacial hyperhidrosis.
Primary hyperhidrosis is a socially embarrassing and functionally incapacitating condition (8) that affects person’s everyday life. It is estimated that about 1-3% of population suffers from this embarrassing condition. It affects both sexes equally and predominately adolescents or young adults (9,10).
Approximately 95% of patients were satisfied with the results of the operation and only a small fraction of patients regretted having the operation, mostly due to severe compensatory sweating of other parts of the body (1,10).
Predominant female patients in both groups in this study can be explained with the fact that female patients care more about the outside appearance than male, despite the fact that primary hyperhidrosis affects equally both sexes (11-13).
The usage of harmonic scalpel during the thoracoscopic sympathectomy is related with some advantages such as less smoke in operative field and less lateral thermal injury and no neuromuscular stimulation (1) which is very important for avoiding the complications like Horner’s Syndrome or hematothorax. On the other hand, electric scalpel-electrocautery hook is non-disposable and costs less then disposable harmonic scalpel (1).
The surgical technique for this minimal invasive operation is standardized, but during time the technique varied only in relation to the level of sympathetic trunk resection, according to the hyperhidrosis symptoms (10). At the start of this study, we performed sympathectomy at level Th2-Th4 but with the evolution of the operation and the aim to diminish the incidence of compensatory sweating, nowadays we perform sympathectomy according to the symptoms. For craniofacial hyperhidrosis at level Th2-Th3 and for combination of palmar and axillar hyperhidrosis at level Th3-Th4 (10,14).
Duration of postoperative pain did not depend on the type of scalpel (electric/harmonic) used in this study and this results are comparable with some other studies (5,15). Most of the patients of both groups had postoperative pain that lasts between 1 or 2 weeks. However, there was a difference in intensity of postoperative pain in those two groups of patients. In the group of patients treated with harmonic scalpel, superior intensity of pain was observed comparing with the group treated with electric scalpel (1,5,16).
Many studies showed variations in evaluation of postoperative pain among patients. Factors as gender, age, individual tolerance to pain can affect the final results of the survey, as well as the fact that the pain is a subjective category and depends on individual sensitivity. The variability seen in literature shows the need to standardize evaluations relating the pain (17).
In this comparative study, based on our results we did not find any significant differences between electric or harmonic scalpel usages for thoracoscopic sympathectomy. Moreover, there was no significant difference between complications and the severity of pain, with slightly higher intensity of pain with harmonic scalpel usage. Both electric and harmonic scalpel provided adequate treatment for primary hyperhidrosis, with the fact that non-disposable electric scalpel costs were less than that of the disposable harmonic scalpel.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Weksler B, Pollice M, Souza ZB, et al. Comparison of ultrasonic scalpel to electrocautery in patients undergoing endoscopic thoracic sympathectomy. Ann Thorac Surg 2009;88:1138-41. [PubMed]
- Dumont P, Denoyer A, Robin P. Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 2004;78:1801-7. [PubMed]
- Molins L, Fibla JJ, Pérez J, et al. Outpatient thoracic surgical programme in 300 patients: clinical results and economic impact. Eur J Cardiothorac Surg 2006;29:271-5. [PubMed]
- Rodríguez PM, Freixinet JL, Hussein M, et al. Side effects, complications and outcome of thoracoscopic sympathectomy for palmar and axillary hyperhidrosis in 406 patients. Eur J Cardiothorac Surg 2008;34:514-9. [PubMed]
- de Campos JR, Wolosker N, Yazbek G, et al. Comparison of pain severity following video-assisted thoracoscopic sympathectomy: electric versus harmonic scalpels. Interact Cardiovasc Thorac Surg 2010;10:919-22. [PubMed]
- Sihoe AD, Manlulu AV, Lee TW, et al. Pre-emptive local anesthesia for needlescopic video-assisted thoracic surgery: a randomized controlled trial. Eur J Cardiothorac Surg 2007;31:103-8. [PubMed]
- Kowalski JW, Eadie N, Daggett S, et al. Validity and reliability of the Hyperhidrosis Disease Severity Scale (HDSS). Poster presented at the 62nd Annual Meeting of the American Academy of Dermatology, 2004, Washington, DC. Poster P198.
- Wang FG, Chen YB, Yang WT, et al. Comparison of compensatory sweating and quality of life following thoracic sympathetic block for palmar hyperhidrosis: electrocautery hook versus titanium clip. Chin Med J (Engl) 2011;124:3495-8. Erratum in: Chin Med J (Engl) 2011;124:4108. [PubMed]
- Lear W, Kessler E, Solish N, et al. An epidemiological study of hyperhidrosis. Dermatol Surg 2007;33:S69-75. [PubMed]
- Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 2011;91:1642-8. [PubMed]
- Dewey TM, Herbert MA, Hill SL, et al. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg 2006;81:1227-32; discussion 1232-3. [PubMed]
- Doolabh N, Horswell S, Williams M, et al. Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg 2004;77:410-4; discussion 414. [PubMed]
- Chou SH, Kao EL, Lin CC, et al. The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc 2006;20:1749-53. [PubMed]
- Deng B, Tan QY, Jiang YG, et al. Optimization of sympathectomy to treat palmar hyperhidrosis: the systematic review and meta-analysis of studies published during the past decade. Surg Endosc 2011;25:1893-901. [PubMed]
- Callejas MA, Rubio M, Iglesias M, et al. Video-assisted thoracoscopic sympathectomy for the treatment of facial flushing: ultrasonic scalpel versus diathermy. Arch Bronconeumol 2004;40:17-9. [PubMed]
- Kopelman D, Bahous H, Assalia A, et al. Upper dorsal thoracoscopic sympathectomy for palmar hyperhidrosis. The use of harmonic scalpel versus diathermy. Ann Chir Gynaecol 2001;90:203-5. [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [PubMed]