Robotic-assisted right inferior lobectomy
Clinical data
Medical history
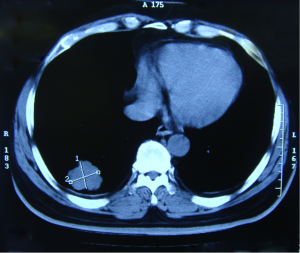
The patient, a 60-year-old man, was admitted due to “cough and expectoration lasted for 1 month and became worse in the past 2 weeks”. One month ago, the patient developed a cough productive for white sputum but without signs/symptoms such as blood in phlegm, difficulty in breathing, chest tightness, shortness of breath, fatigue, or night sweats. After oral administration with roxithromycin and cold drugs by himself, the symptoms were resolved, and no other special treatment was applied. In the past 2 weeks, the cough persisted and became worse. He then visited a local hospital, in which the chest CT showed a lobulated soft-tissue mass sized 3.5 cm in the inferior lobe of right lung. He had a history of hypertension for 9 years, which was satisfactorily controlled by the self-administration of hypotensive drugs. In 2004 and 2007, he received two sessions of heart stent implantation due to myocardial infarction, during which a total of 3 stents were implanted. However, he has stopped using anticoagulant drugs.
Physical examination
No bilateral supraclavicular lymph node enlargement was detected. Chest examination showed no positive sign.
Auxiliary examination
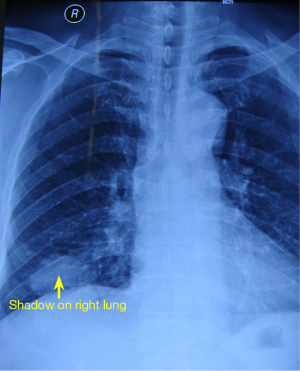
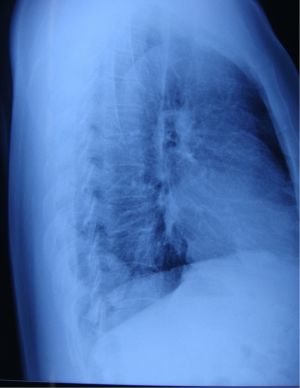
- Chest PA and LAT and CT. A lobulated high-density shadow sized 3.5 cm was seen in the posterior segment of the right inferior lobe. The bilateral pulmonary hilar and mediastinal lymph nodes were not remarkably swollen (Figures 1-3).
- Metastasis was not detected on head CT, bone ECT, and abdominal ultrasonography.
Pre-operative preparation
Same as the conventional open thoracic surgery.
Procedures
Anesthesia and body position
After the induction of general anesthesia, the patient was under double-lumen endotracheal intubation and underwent left-sided one-lung ventilation.
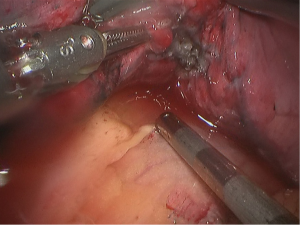
The patient was placed in the left lateral decubitus position and in a Jackknife position (Figure 4).
Surgical procedures
- Incisions. A 1.5-cm camera port was created in the 8th intercostal space at right posterior axillary line, and two 1.0-cm working ports were separately made in the 5th intercostal space at anterior axillary line and the 8th intercostal space at scapular line. A 4-cm auxiliary port was made in the 7th intercostal space at midaxillary line (Figure 5).
- Connection of robot Patient cart. The robot Patient cart is positioned directly above the operating table and then connected. Its left hand was attached to bipolar cautery forceps, and its right hand was attached to a unipolar cautery hook. Incision protector was applied in the auxiliary port.
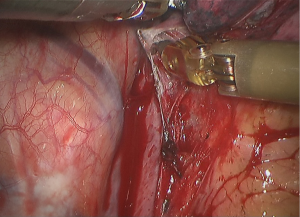
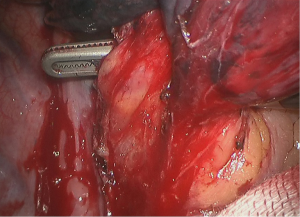
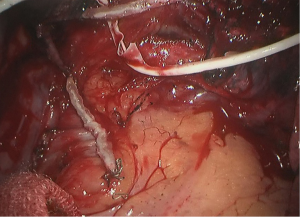
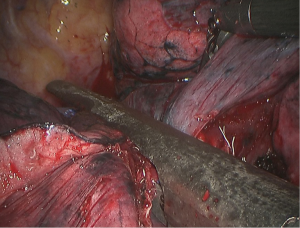
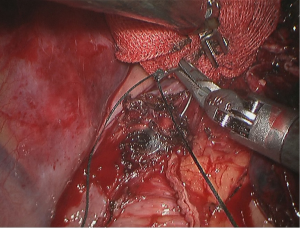
- The adhesion between the inferior lobe and diaphragm was divided using the cautery hook, and the inferior pulmonary ligament was dissociated using the unipolar cautery hook till the inferior pulmonary vein level (Figures 6,7).
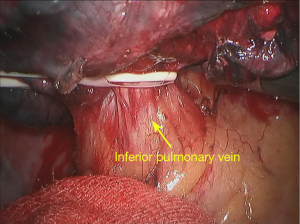
- Dissociate the inferior pulmonary vein (Figure 8).
- Pull the inferior pulmonary vein using elastic cuffs (Figure 9).
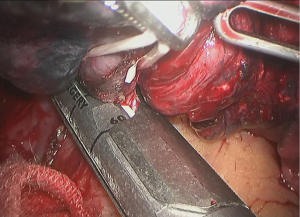
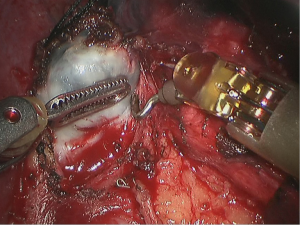
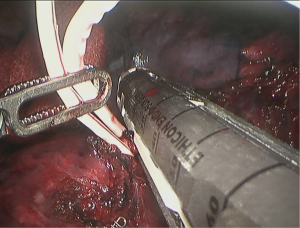
- Cut off the inferior pulmonary vein, and then the vein of the left inferior lobe of the lung was clamped and divided using the single-use endoscopic linear cutter/stapler (white reload) (Figures 10,11).
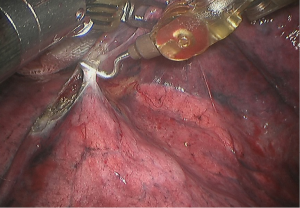
- Dissect the interlobar fissure using the cautery hook (Figure 12).
- Remove the interlobar lymph nodes (Figure 13).
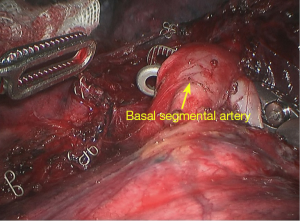
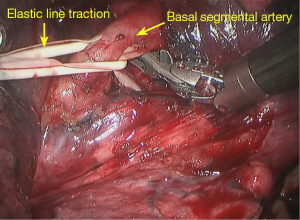
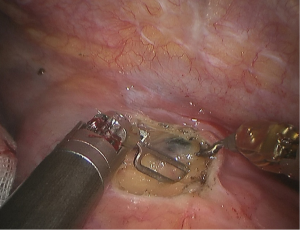
- Dissociate the arteries in the basal segments of lower lobe (Figure 14).
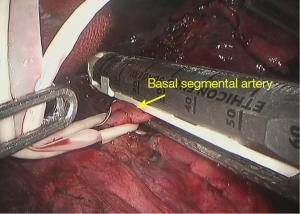
- Pull the arteries in the basal segments using elastic cuffs (Figure 15).
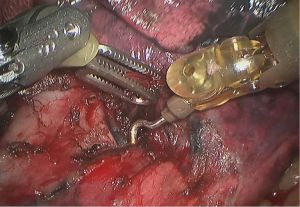
- The arteries in the basal segments were clamped and divided using the single-use endoscopic linear cutter/stapler (white reload) (Figure 16).
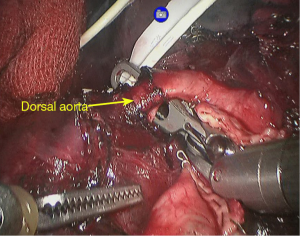
- Dissociate the arteries in the dorsal segments of inferior lobe, and then the elastic cuffs were applied (Figure 17).
- The arteries in the doral segments were clamped and divided using the single-use endoscopic linear cutter/stapler (white reload) (Figure 18).
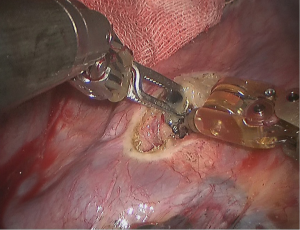
- The lower lobe bronchus was clamped and divided using the single-use endoscopic linear cutter/stapler (golden reload) (Figure 19).
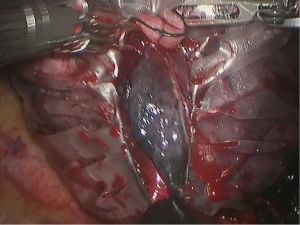
- An extraction bag was inserted to harvest the completely resected right inferior lobe via the incision (Figure 20).
- Remove the lymph nodes in the inferior pulmonary ligament (Figure 21).
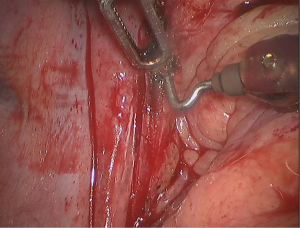
- Dissociate the subcarinal lymph nodes and close the supporting line (Figure 22).
- Completely remove the subcarinal lymph nodes (Figure 23).
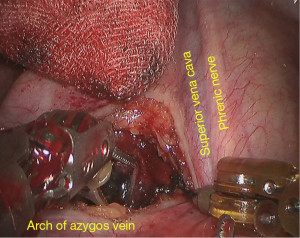
- Remove the lymph nodes near the trachea (Figure 24).
- Remove the lymph nodes near the tracheal bronchus (Figure 25).
- Remove the lymph nodes in front of trachea (Figure 26).
- Saline is then injected to expand the lungs to identify potential leakage of the bronchial stumps (Figure 27).
- Wash the thoracic cavity with warm saline. The robotic arms were withdrawn after the bleeding was stopped. Close the chest after a closed chest drainage tube was placed at the camera port.
Postoperative treatment
Postoperative treatment was similar to that after the conventional open lobectomy.
Pathological diagnosis
The lesion was a poorly differentiated adenocarcinoma (4.2 cm in diameter) in the inferior lobe of right lung. No metastasis was seen at the bronchial stump. While cancer metastasis was found in station 11 lymph nodes (4/5), it was not detected in other stations. Postoperative pathologic staging: pT2aN1M0.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.