Robotic-assisted right middle lobectomy
Clinical data
History
The patient, a 56-year-old man, was admitted due to “a mass in the right lung found during health checkup 2 months ago”. The patient visited our outpatient department for further treatment due to a mass in the right lung found during health checkup 2 months ago. He had no symptom such as fever, chest tightness, shortness of breath, chest pain, or hoarseness. His physical performance was normal, and the body weight did not obviously change.
Physical examination
Physical examinations upon admission showed no obviously positive signs. The cervical and supraclavicular lymph nodes were not abnormally enlarged.
Auxiliary examinations
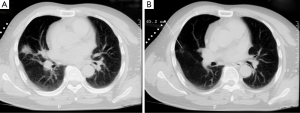
Chest CT: a soft tissue density (1.5 cm × 1.5 cm) with irregular margin was found in the right middle lobe (Figure 1).
Epigastric ultrasound, bone ECT, and head MRI did not find the evidence of remote metastasis. No obvious abnormality was found in ECG, echocardiography, pulmonary function test, blood gas analysis, and other biochemical tests.
Preoperative diagnosis
A space-occupying lesion in the right middle lung lobe.
Pre-operative preparation
Based on the imaging results, “a space-occupying lesion in the right middle lung lobe” was considered; however, the possibility of malignancy could not be ruled out. Since it is a small, peripheral lesion, localization was done pre-operatively using percutaneous CT-guided injection of methylene blue dye, followed by wedge resection. The subsequent surgical protocol was determined based on the results of intraoperative frozen section biopsy. The surgery was performed using da Vinci robotic system.
Surgical procedures
Anesthesia and body position
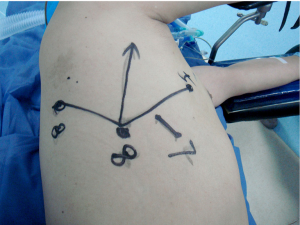
After the induction of general anesthesia, the patient was placed in a right lateral decubitus position under double-lumen endotracheal intubation. With his hands put in front of head, he was fixed in a jackknife position and provided with single-lung (left) ventilation (Figure 2).

Procedures
Incisions: a 1.5 cm camera port was created in the 8th intercostal space (ICS) right posterior axillary line, two 1.0 cm working ports were separately made in the 5th ICS right anterior axillary line and the 8th ICS scapular line, and a 4 cm auxiliary port was made in the 7th ICS midaxillary line (Figure 3).
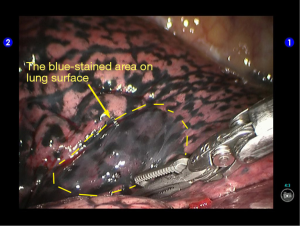
The robot manipulators were connected over the patient’s head. A 12 mm trocar was placed at the camera port in the 8th ICS right posterior axillary line to be attached with the camera arm. The 2# arm (with the left hand attached with bipolar coagulation forceps) and 1# arm (with the right hand attached with pericardial forceps) were placed via the incisions at the 5th ICS right anterior axillary line and the 8th ICS scapular line. Incision protector was applied in the auxiliary port. During the thoracic cavity exploration, the puncture site was visible on the surface of the middle lobe and the subpleural area was stained blue (Figure 4). Deep nodules at the puncture site were touched.
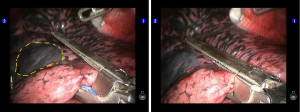
Pulmonary wedge resection: a linear cutter was inserted via the auxiliary port, and the lesion was wedged out using three blue reloads (Figure 5).
The lesion was harvested using an endoscopic retriever; after the lesion was cut open, a homogeneous and dense mass sized 1.5 cm was found inside the pulmonary parenchyma. Frozen pathology showed that it was a lung cancer to be further classified. Lobectomy and lymph node dissection were then performed.
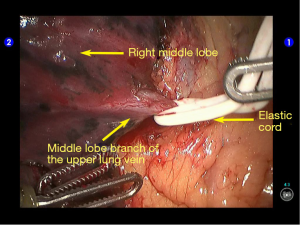
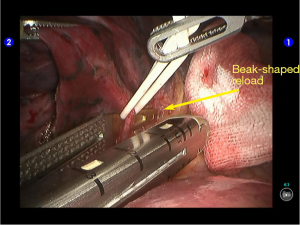
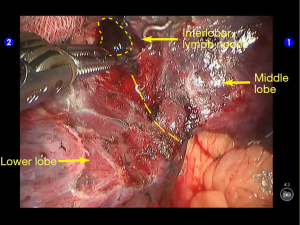
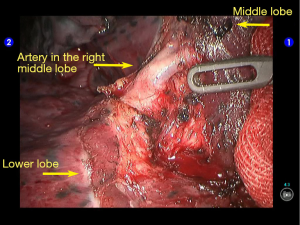
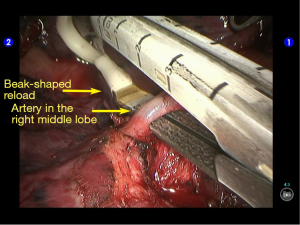
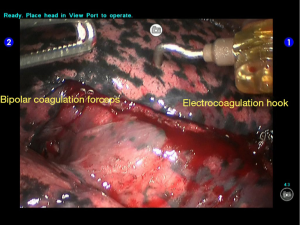
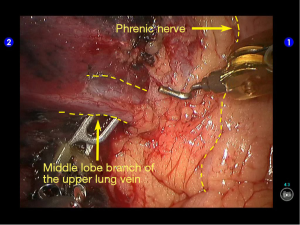
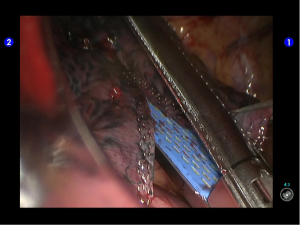
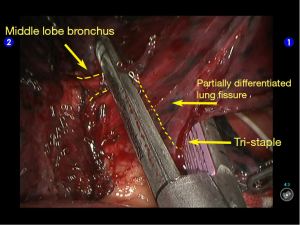
Lobectomy: the left hand was still attached with the bipolar coagulation forceps, whereas the right hand was attached with electrocoagulation hook instead (Figure 6). Further exploration showed that the anterior part of the oblique fissure partially developed while the horizontal fissure basically did not develop. The mediastinal pleura was cut open behind the phrenic nerve to dissociate the middle lobe vein (Figure 7), which was tracted with elastic cord and then dissected using a beak-shaped golden reload (Figures 8,9). The anterior part of the oblique fissure was then dissected to remove the interlobar lymph nodes near the lung artery (Figure 10). The artery in the right middle lobe was dissociated (Figure 11) and then transected with the beak-shaped golden reload (Figure 12). The anterior part of the oblique fissure and the horizontal fissure were separately dissected with one blue reload (Figure 13). A Tri-staple purple reload was applied to clamp the root of the middle lobe bronchus, together with the residual parts of the oblique fissure (Figure 14). An anesthesiologist was asked to suction sputum and ventilate the operated lung, and the ventilation was found to be good in the lower lobe. The middle lobe was dissected using the reload and then removed with the endoscopic retriever.
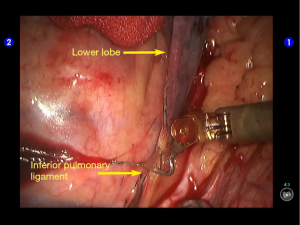
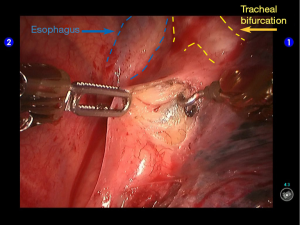
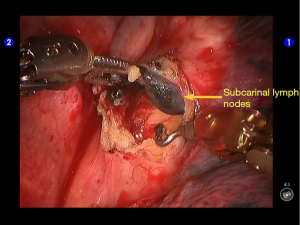
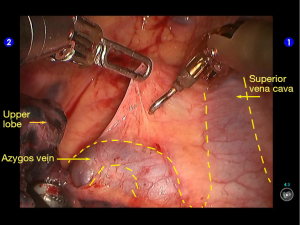
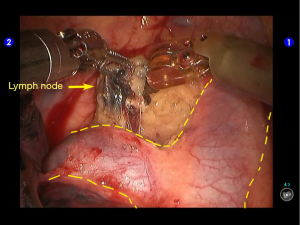
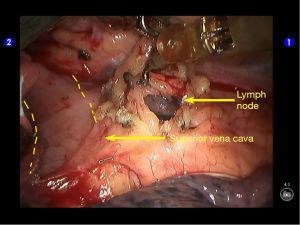
Lymph node removal: after the lower pulmonary ligament was dissected, no obvious lymph node enlargement was observed (Figure 15). Open the posterior mediastinal pleura (Figure 16) to remove several subcarinal lymph nodes (Figure 17). Open the upper mediastinal pleura (Figure 18) to remove several lymph nodes around the trachea (Figure 19) and before the superior vena cava (Figure 20).
Wash the thoracic cavity. If no air leakage was observed during lung recruitment, suction all the rinsing water. When no obvious bleeding was observed at all the trauma surfaces, the Tistat absorbable hemostatic gauze was applied at each trauma surface, followed by the withdrawal of robot arms. Latex drainage tube was inserted via the 5th ICS incision and placed at the residual cavity of the middle lobe. After having been well fixed, the bottle was sealed with water, and the silicone drainage tube was indwelled at the camera port. Close the chest after lung recruitment.
Postoperative treatment
Postoperative treatment is similar to that after the conventional open lobectomy. The latex drainage tube was withdrawn 5 days after the surgery, and the silicone drainage tube was removed 11 days after the surgery. The patient was discharged on the 12th post-operative day.
Pathological diagnosis
Moderately and well-differentiated adenocarcinoma at the right middle lung lobe, without lymph node metastasis. Post-operative pTNM stage: T1aN0M0, Ia stage.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.