
Comparison between Child-Pugh score and Albumin-Bilirubin grade in the prognosis of patients with HCC after liver resection using time-dependent ROC
Introduction
Liver cancer is the seventh most prevalent malignant tumor and the world's third primary source of cancer mortality (1), of which hepatocellular carcinoma (HCC) accounts for about 90% of these cases (2). Hepatic resection is the standard therapy and potentially curative treatment for early-stage HCC according to the BCLC staging system (3), which has been reported to prolong survival in several randomized controlled trials and meta-analyses (4,5). Additionally, there is a growing amount of evidence that supports the application of hepatectomy for patients with intermediate- and advanced-stage HCC (6,7).
Due to the coefficient of multiple factors, the prognosis assessments and management of the HCC patients remain complicated and should take the hepatic function, tumor characteristic, and physical status into consideration (8,9). Among them, the hepatic function is a vital determinant related to the prognosis of HCC. Traditionally, the Child-Pugh classification has been extensively used for the evaluation of liver function and even plays an important role in most of the prevalent staging systems to guide HCC patients for treatment (10,11). However, the application of the Child-Pugh classification has several limitations (12,13). The assessment of ascites and encephalopathy is subjective, and all five parameters have the same weight.
Moreover, ascites and albumin are interrelated. Recently, a novel model based on serum albumin and bilirubin has been put forward for the evaluation of liver function (14), which has shown powerful discriminating value over Child-Pugh classification in predicting overall survival (OS) for patients with HCC undergoing the treatment of sorafenib (15). However, whether the performance of the Albumin-Bilirubin (ALBI) score could veritably reflect the liver function of HCC patients undergoing liver resection has not reached a consensus until now.
It should also be noted that the ALBI score was capable of classifying patients with TACE, stereotactic body radiation and sorafenib into two separate prognostic cohorts (16-18). Therefore, the aim of this analysis was to determine the prognostic importance of the baseline ALBI rating relative to the Child-Pugh score of hepatectomy HCC patients.
Methods
Study population
The clinical, laboratory, and imaging data were extracted from the hospital database of 196 consecutive HCC patients undergoing liver resection at our center from January 2010 to December 2017 for this retrospective study. The patients with Child-Pugh A classification undergoing initial hepatectomy with negative surgical margin proved by the pathological examination after surgery were enrolled in this research. Meanwhile, the patients meeting each of the following criteria were included: no treatment for HCC before liver resection; no other simultaneous malignancies; no cardiopulmonary, renal or cerebral dysfunction before liver resection. Patients with other untreated malignancies or other serious concurrent illnesses or who underwent liver transplantation were excluded. Written informed consent was obtained from all patients before the administration of hepatectomy, and the ethics committee approved this investigation of the hospital.
Treatment and follow-up
Tumor status and resectability were routinely assessed by abdominal ultrasound and contrast-enhanced CT or MRI before liver resection. The main steps of hepatectomy were as follows: dissect the first and second porta hepatis; find the tumor and mark the pre-cut line; tumor excision; stop bleeding if necessary.
All patients were followed up at 1 month after hepatectomy and then 3-month intervals in the first year and every 3–6 months in later years, as appropriate. Routine examinations were conducted at each follow-up, including physical examinations, blood tests [serum (α-fetoprotein) AFP level, serum biochemistry], and imaging examinations (chest X-ray, abdominal ultrasonography, abdominal CT, or MRI). Patients with recurrence received repeated liver resection, radiofrequency ablation (RFA), transcatheter arterial chemoembolization (TACE), or Sorafenib treatment, depending on the liver function, status of the tumor, and economic conditions of patients. OS was defined as the time from date of resection until death or until the last follow-up. The last visit was done on October 15, 2019.
Child-Pugh score and ALBI score calculation
The HCC was diagnosed by contrast-enhanced magnetic resonance imaging (MRI) and computed tomography (CT) according to the American Association for the Study of the Liver Disease or European Association for the Study of Liver disease (AASLD/EASL) guidelines (13,14).
The Child-Pugh score was based on the total bilirubin, albumin, prothrombin time, and the clinical findings of encephalopathy and ascites. It was graded as 5–6 points for Child-Pugh-A; 7–9 points for Child-Pugh-B; and 10–15 points for Child-Pugh-C (15). The following formula determined the ALBI score: (log10bilirubin × 0.66) + (−0.085 × albumin). The ALBI score was graded as: score ≤−2.60 as ALBI-1; −2.60< score ≤−1.39 as ALBI-2; and score >−1.39 as ALBI-3 (16).
Statistical analysis
Categorical variables are expressed as frequencies and percentages; continuous variables are expressed as means (interquartile range). Survival analyses were performed using the Kaplan-Meier method, and the log-rank test examined the statistical differences between the ALBI grade and Child-Pugh scores. Cox proportional hazards model was used for the univariate and multivariate analyses of prognostic factors of OS. Three multivariate models with stepwise methods were separately conducted for selecting the independent prognostic factors: model 1, including the baseline characteristics; model 2 including the baseline characteristics and Child-Pugh score but excluding albumin and bilirubin; model 3 including the baseline characteristics and ALBI score but also excluding albumin and bilirubin. Model validation of different staging systems was compared using the C-index as a measure of discrimination. Statistically significant was identified as P values <0.05 for all analyses. Statistical analyses were conducted using IBM SPSS software version 23.0 (SPSS Inc., Chicago, IL, USA) and R software version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
According to the protocol, this study cohort consisted of 196 patients. Among the enrolled patients, 171 (87.2%) patients were male with a mean age of 55.7 years, and 25 (12.8%) patients were female with a mean age of 55.4 years. Based on the ALBI grade, there were 81 (41.3%), and 115 (58.7%) patients belonged to the group of ALBI-1 and ALBI-2, respectively. According to the Child-Pugh classification system, there were 136 (69.4%) patients of Child-Pugh-A5, 60 (30.6%) of Child-Pugh-A6. For patients with Child-Pugh-A5, there were 81 (59.6%) patients with ALBI-1 and 55 (40.4%) patients with ALBI-2. Among patients with Child-Pugh-A6, all patients were ALBI-2. The mean tumor size (maximum diameter of the largest tumor) was 8.02 cm, and the entire patients enrolled in this study had a unifocal tumor. The demographic and clinical features of the HCC patients were summarized in Table 1.
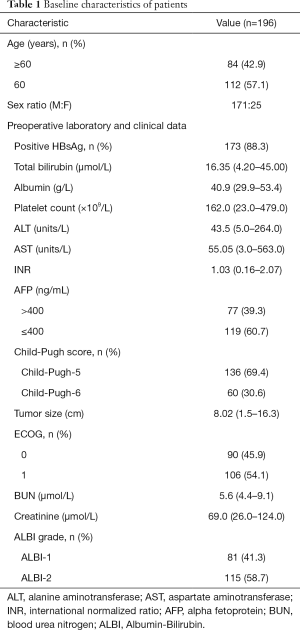
Full table
Survival analyses according to Child-Pugh score and ALBI
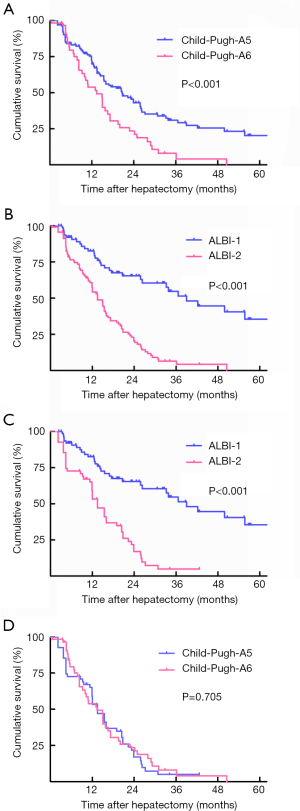
During a median follow-up of 32.8 months, 120 patients had died, and the median OS reached 16.9 months. Based on the Kaplan-Meier curves, both ALBI grade and Child-Pugh scores were significantly related to OS. According to the Child-Pugh system, patients with Child-Pugh-A5 showed better OS than those with Child-Pugh-A6, with respective OS at 1, 3 and 5 years (72.7%, 29.2%, 20.3% vs. 53.9%, 21.1%, 0%, Log-rank P<0.001; Figure 1A). Based on the ALBI grade, there was a significant difference in OS between patients with ALBI-1 and ALBI-2 grade. OS at 1, 3 and 5 years was higher in patients with ALBI-1 (82.7%, 51.5%, and 35.5%) than those with ALBI-2 (57.6%, 19.4%, and 0%; Log-rank P<0.001; Figure 1B). Among patients with Child-Pugh-A5, ALBI grade classified patients with Child-Pugh A5 into two distinct survival group and the patients with ALBI-1 had a higher OS at 1, 3 and 5 years than those with ALBI-2 (82.7%, 51.5%, 35.5% vs. 53.3%, 4.8%, 4.8%, respectively; Log-rank P<0.001; Figure 1C). Among patients with ALBI-2, there was no significant difference in OS at 1,3 and 5 years between the patients with Child-Pugh-A5 and Child-Pugh-A6 (59.2%, 4.8%, 4.8% vs. 53.9%, 4.0%, 4.0%, respectively; Log-rank P=0.7050; Figure 1D).
Univariate and multivariate analyses
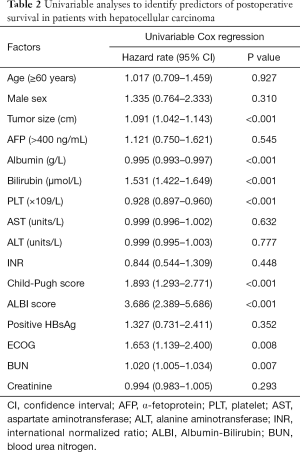
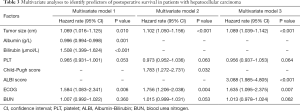
According to the univariate analysis for OS, tumor size, albumin, bilirubin, platelet (PLT), ECOG performance status, BUN as well as Child-Pugh score and ALBI grade were significant prognostic factors (P<0.05; Table 2). In multivariate model 1, tumor size (HR 1.069, P=0.010), albumin (HR 0.996, P=0.001), bilirubin (HR 1.508, P<0.001) and ECOG performance status (HR 1.584, P=0.006) were identified as independent predictors of OS. According to the multivariate model 2, the independent prognostic factors included tumor size (HR 1.102, P<0.001), ECOG performance status (HR 1.756, P=0.004), and Child-Pugh score (HR 1.783, P=0.032). For the multivariate model 3, the independent predictors of OS were tumor size (HR 1.089, P<0.001), ECOG performance status (HR 1.635, P=0.007), and ALBI grade (HR 3.088, P<0.001) (Table 3).
Full table
Full table
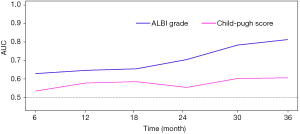
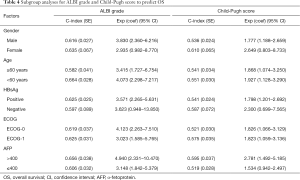
Comparison of the discriminatory abilities for Child-Pugh score and ALBI grade in predicting survival
Figure 2 shows AUCs for Child-Pugh score and ALBI grade and OS from 6 to 36 months after the start of follow-up using time-dependent ROC analysis. ALBI grade had higher predictive power than the Child-Pugh score for OS based on time-dependent AUCs. Besides, their predictive abilities were investigated in subsets of patients with different baseline characteristics, especially for long-term outcomes. The ALBI grade showed better prognostic performance than the Child-Pugh score in the entire subsets according to the subgroup analyses (Table 4).
Full table
Discussion
According to our study, we demonstrated that the ALBI grade and Child-Pugh score could separately predict the OS of HCC patients with Child-Pugh A and receiving hepatectomy, and the ALBI score showed a better discriminatory power than Child-Pugh score. Besides, the ALBI grade could classify the patients with Child-Pugh-A and Child-Pugh-A5 into two distinct prognostic cohorts.
The key issue in predicting the outcomes of HCC patients is to assess the liver function reserve to select proper candidates for liver resection. For many years, the traditional Child-Pugh rating system is the most widely used method for assessing liver function and predicting therapeutic efficacy. However, the accuracy of the Child-Pugh score has become controversial recently in consideration of its limitations. Previous studies tried to assess the ALBI grade for patients treated with hepatectomy, but the reliability of the research was weakened by its retrospective specialty, single-center data, and comparably small sample (19). More importantly, previous studies did not use time-dependent receiver operating characteristic (ROC) curves to compare the ability to predict survival between ALBI grade and Child-Pugh score for censored data and compared the area under the ROC curve (AUC) (20).
In this study, we proved that the ALBI grade and Child-Pugh score could separately predict the OS of HCC patients with Child-Pugh A undergoing liver resection. In the patients included in our research, all patients with Child-Pugh-A5 were graded as ALBI-1. However, patients with ALBI-2 had different Child-Pugh score. In the entire cohort, according to the Kaplan-Meier curves, there was a significant difference in OS between ALBI-1 grade and ALBI-2 grade. Moreover, in patients with Child-Pugh A, the patients with Child-Pugh-6 had a worse prognosis than patients with Child-Pugh-5. In addition, the same category based on Child-Pugh-A5 could be further divided into distinct prognostic groups by the ALBI grade. It is worth noting that the Child-Pugh class could not discriminate between distinguishing prognostic groups within the same category of ALBI-2. As a result, the ALBI grade might be a more reasonable and exact evaluation tool for liver function.
Univariable and multivariable analyses were conducted to revealed factors with OS. For multivariable analysis, the albumin and total bilirubin, the Child-Pugh score and the ALBI grade were entered in three different Cox proportional hazards regression models to avoid collinearity. The patients with poor prognosis were relevant with a high grade of Child-Pugh and ALBI. Tumor size and ECOG performance status could also be independent predictors of OS except the Child-Pugh score and the ALBI grade through univariable and multivariable analyses. Nevertheless, positive HBsAg, ALT, AST, and AFP levels were regarded as no statistical significance, which might be caused by the small sample size.
Time-dependent ROC curves have been introduced to assess the predictive power of diagnostic markers for time-dependent disease outcomes (21). Although both Child-Pugh score and ALBI grade have been confirmed as independent factors associated with OS utilizing multivariate analysis, in this study, time-dependent ROC analysis showed that ALBI grade was superior to Child-Pugh score in terms of the discriminatory ability for OS more than 3 years, especially in the long-term outcomes. Additionally, subgroup analysis revealed that both ALBI grade and Child-Pugh scores were significant predictors of OS in the entire subsets; however, ALBI grade showed better prognostic performance than the Child-Pugh score in the entire subsets other than a female subgroup.
However, there were several limitations to this study, which should be declared here. Firstly, although the quality control was ensured because the same experienced team conducted all procedures and administrations, the single-center and retrospective nature of this study might still introduce some bias. Secondly, this study concluded a small sample size in which patients with Child-Pugh B, C and ALBI-3 grade were not included. Whether the results of our study could be applied to the patients with a poorer liver function, further studies with a large sample and effective multivariable controls are necessary. Finally, most of the patients in our study were Chinese with an infection of hepatitis B virus as the cause of HCC, compared with most Western countries where the etiologies of HCC were mainly hepatitis C virus infection and alcoholic liver disease. Thus, the generalization of our findings should be cautious, and future prospective studies are needed.
In conclusion, for HCC patients with preserved liver function (Child-Pugh A) and diagnosed with hepatectomy, our study shows that the ALBI level could be an acceptable measure of liver function and could be better for stratifying prognosis than the Child-Pugh score. Such findings may have significant implications for the future design of research, and to improve its predictability, it is important to adapt this high-quality, evidence-based model to the existing HCC staging process.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.02.85). LL serves as the unpaid editorial board member of Annals of Translational Medicine from Apr 2020 to Mar 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from all patients before the administration of hepatectomy. This investigation was approved by the Clinical Research Ethics Committee of the Tangdu Hospital.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Galle PR, Forner A, Llovet JM, et al. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 2018;69:182-236. [Crossref] [PubMed]
- Cillo U, Vitale A, Grigoletto F, et al. Prospective validation of the Barcelona Clinic Liver Cancer staging system. J Hepatol 2006;44:723-31. [Crossref] [PubMed]
- Chen J, Huang J, Chen M, et al. Transcatheter arterial chemoembolization (TACE) versus hepatectomy in hepatocellular carcinoma with macrovascular invasion: a meta-analysis of 1683 patients. J Cancer 2017;8:2984-91. [Crossref] [PubMed]
- Tsilimigras DI, Bagante F, Sahara K, et al. Prognosis After Resection of Barcelona Clinic Liver Cancer (BCLC) Stage 0, A, and B Hepatocellular Carcinoma: A Comprehensive Assessment of the Current BCLC Classification. Ann Surg Oncol 2019;26:3693-700. [Crossref] [PubMed]
- Garancini M, Pinotti E, Nespoli S, et al. Hepatic resection beyond barcelona clinic liver cancer indication: When and how. World J Hepatol 2016;8:513-9. [Crossref] [PubMed]
- Komatsu S, Kido M, Tanaka M, et al. Clinical Relevance of Reductive Hepatectomy for Barcelona Clinic Liver Cancer Stages B and C Advanced Hepatocellular Carcinoma: A Single-Center Experience of 102 Patients. World J Surg 2019;43:2571-8. [Crossref] [PubMed]
- Subramaniam S, Kelley RK, Venook AP. A review of hepatocellular carcinoma (HCC) staging systems. Chin Clin Oncol 2013;2:33. [PubMed]
- Bruix J, Reig M, Sherman M. Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology 2016;150:835-53. [Crossref] [PubMed]
- Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020-2. [Crossref] [PubMed]
- European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43. [Crossref] [PubMed]
- Wu JJ, Zhang ZG, Zhu P, et al. Comparative liver function models for ruptured hepatocellular carcinoma: A 10-year single center experience. Asian J Surg 2019;42:874-82. [Crossref] [PubMed]
- Wang YY, Zhao XH, Ma L, et al. Comparison of the ability of Child-Pugh score, MELD score, and ICG-R15 to assess preoperative hepatic functional reserve in patients with hepatocellular carcinoma. J Surg Oncol 2018;118:440-5. [PubMed]
- Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 2015;33:550-8. [Crossref] [PubMed]
- Ogasawara S, Chiba T, Ooka Y, et al. Liver function assessment according to the Albumin-Bilirubin (ALBI) grade in sorafenib-treated patients with advanced hepatocellular carcinoma. Invest New Drugs 2015;33:1257-62. [Crossref] [PubMed]
- Murray LJ, Sykes J, Brierley J, et al. Baseline Albumin-Bilirubin (ALBI) Score in Western Patients With Hepatocellular Carcinoma Treated With Stereotactic Body Radiation Therapy (SBRT). Int J Radiat Oncol Biol Phys 2018;101:900-9. [Crossref] [PubMed]
- Lee IC, Hung YW, Liu CA, et al. A new ALBI-based model to predict survival after transarterial chemoembolization for BCLC stage B hepatocellular carcinoma. Liver Int 2019;39:1704-12. [Crossref] [PubMed]
- Tada T, Kumada T, Toyoda H, et al. Impact of albumin-bilirubin grade on survival in patients with hepatocellular carcinoma who received sorafenib: An analysis using time-dependent receiver operating characteristic. J Gastroenterol Hepatol 2019;34:1066-73. [Crossref] [PubMed]
- Zhang ZQ, Xiong L, Zhou JJ, et al. Ability of the ALBI grade to predict posthepatectomy liver failure and long-term survival after liver resection for different BCLC stages of HCC. World J Surg Oncol 2018;16:208. [Crossref] [PubMed]
- Wang YY, Zhong JH, Su ZY, et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg 2016;103:725-34. [Crossref] [PubMed]
- Lambert J, Chevret S. Summary measure of discrimination in survival models based on cumulative/dynamic time-dependent ROC curves. Stat Methods Med Res 2016;25:2088-102. [Crossref] [PubMed]


