
Increased multidrug resistant isolates: new clinical burdens for 66 hospitals in Shanghai, 2015 to 2017
Introduction
In recent years, drug-resistant bacteria have become a major medical obstacle for hospitals and patients, particularly with the emergence of multi-drug resistant bacteria, leading to an unprecedented burden on the treatment and rehabilitation of patients (1). The correct pathogen detection is the basis for rational use of antibacterial drugs and monitoring bacterial resistance. In addition, it plays an important role in reducing the production of resistant bacteria and improving infection control. Different types of pathogens have different detection status of drug-resistant bacteria, which can impact on the clinical diagnosis and treatment to a certain extent (2). How to choose the appropriate specimen for testing and reduce the unnecessary clinical specimens, thus reducing the overuse of antibacterial and the probability of drug-resistant bacteria, has become an important issue of hospitals. In recent years, China has done a lot of work on the prevention and control of multi-drug resistant bacteria (3). As one of the most advanced cities with abundant medical resources in China, Shanghai is focusing on the correct and compliant delivery of clinical pathogens and the management of drug-resistant bacteria. This study aims to understand the current status and the trends of clinical pathogen detection rates in specimens and drug-resistant bacteria rates in Shanghai from 2015 to 2017.
Methods
Data source
In this study, the relevant data in 2015 and 2017 were obtained from 66 secondary and above-level hospitals in Shanghai. The data collection was all permitted.
Survey contents
The self-made questionnaires were used in January 2016 and January 2018 to investigate the rates of antibiotic prescription, microbial specimens and drug resistance in 66 hospitals of Shanghai in 2015 and 2017. We collected the following data in testing microbial specimens: (I) The rate of antibiotic use, which included the number of use cases and the proportion. (II) The number of cases of specimen, which included the number of cases of blood culture and its bottle number when sent, the number of cases of sputum culture and urine culture. (III) The status of the drug resistance: the number of Staphylococcus aureus, methicillin-resistant Staphylococcus aureus (MRSA), Acinetobacter baumannii, carbapenem-resistant Acinetobacter baumannii (CRAB), Pseudomonas aeruginosa, carbapenem-resistant Pseudomonas aeruginosa (CRPA), Escherichia, extended-spectrum β-lactamase-producing Escherichia (ESBL-ESC), Klebsiella pneumoniae, extended-spectrum β-lactamase Klebsiella pneumoniae (ESBL-KP), Enterococcus sp and vancomycin-resistant Enterococcus sp (VRE) strains detected in sputum culture, blood culture and urine culture and their proportion.
Data collection
The survey was conducted by the means of online submission. Before the investigation, the Shanghai Nosocomial infection Quality Control Center conducted standard training for people in participated hospitals who were responsible for the issue. After the investigation, the Shanghai Nosocomial infection Quality Control Center was responsible for the collection and verification of the results. Improper questionnaires were required to revise. Moreover, the Center cooperated with the microbiology laboratory and infection control department of participated hospitals for further verification when supervision.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data analysis
(I) The rate of antibacterial use = the number of antibiotics prescribed for inpatients/the total number of inpatients in the year ×100%. (II) The proportion of blood/sputum culture = the number of blood or sputum culture/the total number of pathogens sent for detection. (III) The P50 (P25, P75) of blood/sputum culture was calculated from the average proportion of blood/sputum culture in each hospital. (IV) The P50 (P25, P75) of the average number of bottles sent for blood culture was calculated from the average number of bottles sent for blood culture in each hospital. (V) The detection rate of multi-drug resistant bacteria= the number of strains detected of multi-drug resistant bacteria/the total number of strains detected in this pathogen ×100%. (VI) The proportion of multi-drug resistant bacteria specimen detected from the sputum samples = the number of multi-drug resistant bacteria strains detected from the sputum samples/the total number of multi-drug resistant strains detected from the all specimens ×100%. (VII) The detection rate of a certain multi-drug resistant bacteria in a certain type of specimen = the number of multi-drug resistant bacteria in a certain specimen/the total number of strains detected by this pathogen in one type of specimen ×100%.
Statistical analysis
The SPSS 20.0 statistical software was used for data analysis after the data were exported and verified. The statistical description of the non-normal distribution data was expressed by the median and inter-quartile range P50 (P25, P75). The χ2 test and Z test were used to assess the differences with data comparison. The statistical significance level was set at P<0.05.
Results
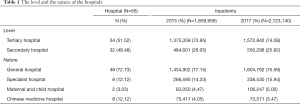
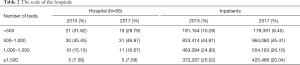
Basic information of the investigated hospitals
A total of 66 secondary and above-level hospitals in Shanghai were investigated in 2015 and 2017. The number of hospital beds had changed during 2015–2017 in some hospitals. The level, nature and scale of the hospitals surveyed are shown in Tables 1,2.
Full table
Full table
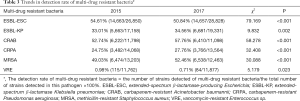
The trends of multi-drug resistant bacteria detection rate
Among the six multi-drug resistant bacteria investigated, the detection rate of CRAB, MRSA, ESBL-KP and CRPA in 2017 increased compared with 2015, the difference was statistically significant (P<0.001). By contrast, the detection rate of ESBL-ESC and VRE decreased compared with 2015, the difference was statistically significant (P<0.05), see Table 3.
Full table
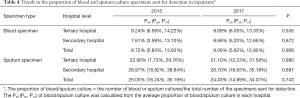
Trends of the proportion of blood and sputum culture specimens in the inpatients’ pathogen detection
As shown in Table 4, compared with 2015, there was no significant change in the proportion of blood specimens and sputum specimens in 2017 (P>0.05), no matter what level of hospital. The clinical pathogen detection still relied mainly on sputum specimens in 2017.
Full table
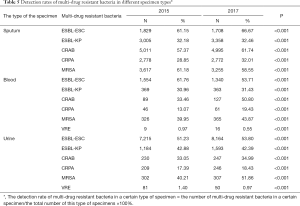
Trends in detection rates of multi-drug resistant bacteria in different specimen types
Table 5 showed that among the sputum specimens, the detection rates of ESBL-ESC, ESBL-KP, CRAB, CRPA in 2017 were increased while the MRSA was decreased than those in 2015, the difference was statistically significant (P<0.001). Among the blood samples, the detection rates of ESBL-KP, CRAB, CRPA and MRSA increased while the rates of ESBL-ESC and VRE decreased compared with 2015, the difference was statistically significant (P<0.005). Among the urine samples, the detection rates of ESBL-ESC, CRAB, CRPA, and MRSA were all lower than those in 2015 while the ESBL-KP and VRE decreased compared with 2015, the difference was statistically significant (P<0.001).
Full table
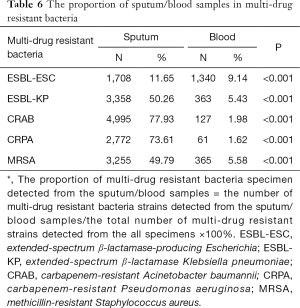
The proportion of sputum/blood samples in multi-drug resistant bacteria detection in 2017
The results of the study showed that the proportion of sputum samples in ESBL-ESC, MRSA, CRAB, ESBL-KP and CRPA were all higher than detected from the blood specimens, the difference was statistically significant (P<0.001) see Table 6.
Full table
Discussion
There is global economic and clinical concern that antimicrobial resistance, especially multi-drug resistance is a major threat to healthcare (4). Antibiotic resistance causes people to be sick for longer and increases the risk of death (5) and are associated with higher mortality rates, longer hospitalizations, and increased health care expenditures (6). In China, the national average detection rate of ESBL-ESC, ESBL-KP, CRAB, CRPA and MRSA was 55.9%, 24.3%, 52.1%, 22.3% and 39.2%, respectively (7). In our study, the detection rate of multiple drug resistance in Shanghai was far higher than the national average level. Although as one of the most developed cities in China, Shanghai needs to undertake more critical patients, the detection rate of multiple drug resistance may be relatively high, but for its part, health-care workers in Shanghai still need to strengthen their own standards, reduce the rate of multiple drug resistance.
The frequency of antimicrobial resistance has increased globally due to misuse and overuse of antibiotics, and multi-drug resistant (MDR) bacteria are now recognized as a major cause of hospital-acquired infections (HAI) (8). During the clinical diagnosis and treatment, untimely or incorrect clinical specimen collection often leads to difficulties in the early detection of multi-drug resistant bacteria, or is misleading as the colonization can be treated as an infection (6). Accurate and timely clinical pathogen detection is very important for the appropriate prescribing of antimicrobial agents, and thereby can reduce the selective pressure of antibacterial drugs, delay and decrease the production of multi-drug resistance (9).
Sputum specimens often account for a large part of clinical examination, because they are one of the fast and simple methods to detect pathogens of respiratory infection (7,10,11). Sampling sputum specimens is relatively easy and non-invasive. But in fact, it is also difficult to get good sputum specimens. Patients often do not have a good deep cough, but mix a lot of saliva (12). The pathogens detected in this kind of sputum specimen may be the oral colonization (13). In view of the recognition of qualified semi quantitative sputum culture by Infectious Diseases Society of America (IDSA) and the advance of microbial laboratory in China, high quality sputum specimens and sterile specimens obtained by bronchoscopy are essential for the etiology diagnosis (9). At the same time, for sputum specimens, it is more difficult to identify whether the pathogen is a colonized or an infected strain, thus misleading the clinical medication (14). Repeated sputum specimen detection may result in different bacteria, which may cause confusion to clinicians (15). Sterile site samples, such as blood samples, can better reflect the real infection situation. Therefore, sputum specimens are more likely to overestimate drug resistance than blood specimens. Attention should be paid to the examination of clinical specimens from sterile sites, which is one of the requirements of WHO in the prevention of multiple drug resistance (5). The global antibacterial drug experts have increased emphasis on increasing the rate of inspection of sterile parts (16). In this study, we found that among the sputum specimens, the detection rates of ESBL-ESC, ESBL-KP, CRAB, CRPA in 2017 were increased than those in 2015, indicating that health-care workers in Shanghai still need to be more stringent and standardized in indication for sending inspection of sputum specimen.
The disadvantage of this paper lies in the lack of analysis of data in Carbapenem Resistant Enterobacteriaceae (CRE) of Shanghai. Because the difference between China and the global is that VRE is less detected than CRE (2). In recent years, CRE has been the focus of attention in China. In future research, we will add data analysis of CRE.
In summary, continuing to reduce inappropriate antibiotic prescribing has great clinical significance on delaying the production of drug-resistant bacteria. It is necessary to tighten the supervision of antimicrobial drugs in tertiary hospitals to improve their management in this area. Moreover, identifying the correct clinical pathogens is not only important to the drug-resistant bacteria supervision, but also has great clinical significance on treatment options, even delaying the spread of drug-resistant bacteria.
Conclusions
The average rate of antibacterial use in Shanghai’s 66 hospitals from 2015 to 2017 showed a downward trend. However, the detection of multi-drug-resistant bacteria still mainly comes from sputum samples, which easily leads to overestimation of the detection rate of multi-drug-resistant bacteria and affects clinical diagnosis and treatment. Therefore, it is still necessary to continue to strengthen the proportion of sterile sites while sending for examination.
Acknowledgments
We are grateful for infection control practitioners in all participated hospitals for their hard work on collecting data and performing interviews. We appreciate the great support of the medical staff from Shanghai’s 66 hospitals who participated in the survey.
Funding: This work was supported by the 4th Three-year Action Plan for Public Health of Shanghai (The Project No: 15GWZK0101) and the Research project plan of Shanghai Municipal Commission of Health and Family Planning Funding (201640313).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Merli M, Lucidi C, Di Gregorio V, et al. The spread of multi drug resistant infections is leading to an increase in the empirical antibiotic treatment failure in cirrhosis: a prospective survey. PLoS One 2015;10:e0127448. [Crossref] [PubMed]
- Gould IM, Wang GQ, Wu JJ, et al. MDRO Beijing Consensus Meeting Report: Global burden of multidrug-resistant organisms' current antimicrobial resistance problems in Asia-Pacific. J Glob Antimicrob Resist 2014;2:7-9. [Crossref] [PubMed]
- Xiao YH. National action plan on antimicrobial resistance: a great blueprint based on "One Health". Chin J Clin Infect Dis 2016;9:289-93.
- Cooke J, Stephens P, Ashiru-Oredope D, et al. Longitudinal trends and cross-sectional analysis of English national hospital antibacterial use over 5 years (2008-13): working towards hospital prescribing quality measures. J Antimicrob Chemother 2015;70:279-85. [Crossref] [PubMed]
- WHO. WHO’s first global report on antibiotic resistance reveals serious, worldwide threat to public health. World Health Organization, 2015.
- Patel SJ, Oliveira AP, Zhou JJ, et al. Risk factors and outcomes of infections caused by extremely drug-resistant gram-negative bacilli in patients hospitalized in intensive care units. Am J Infect Control 2014;42:626-31. [Crossref] [PubMed]
- Tang X, Xiao M, Zhuo C, et al. Multi-level analysis of bacteria isolated from inpatients in respiratory departments in China. J Thorac Dis 2018;10:2666-75. [Crossref] [PubMed]
- Wang M, Wei H, Zhao Y, et al. Analysis of multidrug-resistant bacteria in 3223 patients with hospital-acquired infections (HAI) from a tertiary general hospital in China. Bosn J Basic Med Sci 2019;19:86-93. [Crossref] [PubMed]
- Wang J, Wang X, Xu H. Antimicrobial resistance and dissemination of multidrug resistant organisms-A review. Wei Sheng Wu Xue Bao 2016;56:1671-9. [PubMed]
- Sharifi-Rad J, Belkum AV, Fallah F, et al. Rising Antimicrobial Resistance in Iran. Der Pharmacia Lettre 2016;8:31-3.
- Sharifi-Rad M, Iriti M, Sharifi-Rad M, et al. Anti-methicillin-resistant Staphylococcus aureus (MRSA) activity of Rubiaceae, Fabaceae and Poaceae plants: A search for new sources of useful alternative antibacterials against MRSA infections. Cell Mol Biol (Noisy-le-grand) 2016;62:39-45. [PubMed]
- Willinger B, Haase G. State-of-the-Art Procedures and Quality Management in Diagnostic Medical Mycology. Curr Fungal Infect Rep 2013;7:260-72. [Crossref]
- Horie H, Ito I, Konishi S, et al. Isolation of ESBL-producing Bacteria from Sputum in Community-acquired Pneumonia or Healthcare-associated Pneumonia Does Not Indicate the Need for Antibiotics with Activity against This Class. Intern Med 2018;57:487-95. [Crossref] [PubMed]
- Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health 2015;109:309-18. [Crossref] [PubMed]
- Alanazi MQ, Al-Jeraisy MI, Salam M. Prevalence and predictors of antibiotic prescription errors in an emergency department, Central Saudi Arabia. Drug Healthc Patient Saf 2015;7:103-11. [PubMed]
- Calfee DP, Salgado CD, Milstone AM, et al. Strategies to prevent methicillin-resistant Staphylococcus aureus transmission and infection in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:772-96. [Crossref] [PubMed]


