A survey of primary care physician referral to bariatric surgery in Manitoba: access, perceptions and barriers
Introduction
The obesity epidemic is an important public health challenge facing Canadians today. Statistics published by the Public Health Agency of Canada in 2007–2009 indicate that approximately one-quarter of adult Canadians live with obesity and that the rate of obesity in Canada has doubled over the last three decades. Unfortunately, the prevalence of obesity is expected to increase further (1). Obesity is defined by the World Health Organization as a body mass index (BMI) greater than 30 kg/m2 and is further subdivided into class I (BMI 30.0–34.9 kg/m2), class II (BMI 35.0–39.9 kg/m2) and class III (BMI ≥40.0 kg/m2) (2,3). Obesity is associated with many comorbidities including heart disease, type 2 diabetes, hypertension, hyperlipidemia, cardiovascular and cerebrovascular disease, osteoarthritis, and sleep apnea (4-6). It is linked to increased health care cost as well as diminished worker productivity (1). Treatments for obesity include education, counseling, dietary modification and increased physical activity (7-9). However, medical management alone results in only 3–5% of excess weight loss (EWL) (9). Bariatric surgery has therefore emerged as one of the most effective therapies to reduce weight and ameliorate or prevent obesity-related co-morbidities and mortality (2,5,10).
The management of obesity presents its own challenges for primary care physicians (PCPs). Poor outcomes may result if these challenges are not appreciated (5,11). PCPs play an instrumental role in managing obesity-related co-morbidities. Despite this, past survey-based studies have reported that many PCPs are not comfortable in discussing obesity and its related comorbidities directly with their patients (12). For those that do counsel their patients, the most frequent recommendations are daily calorie reduction, exercise, nutritional counseling and behavior modification (2). The predominant barriers to management of obesity include negative attitudes towards obese patients, inadequate time, lack of resources, and lack of formal training and competence in management (13). In addition, a study by Avidor et al. showed “most physicians report that they are ill-equipped and uneducated to treat the condition of obesity” and “may view treatment of obesity as futile, that it is significantly less effective than treating other chronic conditions” (2).
Thus, a significant gap exists between current physician practice and the optimal management of obesity. Avidor et al. report that while bariatric surgery was perceived as the most effective treatment for morbid obesity, only 21.9% of PCPs reported referring their patients for consultation (2). A lack of knowledge surrounding the efficacy and safety of bariatric surgery may be one of the main determinants of low referral rates (13). A survey of 500 family physicians from New Jersey indicates that only 44% knew that bariatric surgery existed as an option for their patients (13). Other reasons for the low referral rates were inadequate knowledge of long-term treatment, lack of understanding of National Institute of Health (NIH) morbid obesity guidelines, perceived post-operative morbidity and mortality, and lack of familiarity with local bariatric surgeons (2,12,13).
Recently there has been a greater focus on educating PCPs on the treatment of obesity but the impact of this effort remains unknown. The purpose of this study is to determine current perceptions, knowledge and limitations/barriers for bariatric surgery among PCPs physicians in a government funded provincial program.
Methods
A questionnaire-based, cross sectional study of family physicians in Manitoba, Canada, was performed between July 1 and September 30, 2015. Institutional research ethics board approval was obtained. The questionnaire was developed by bariatric surgeons and validity of the instrument was reviewed by a panel of family physicians for content and clarity. It addressed the referral pattern of family physicians in Manitoba to bariatric surgery and their familiarity with the provincial bariatric program. It also assessed their knowledge, perceptions and attitudes towards bariatric surgery. In total, 32 questions were developed to address the above points (see Supplementary file for survey questions).
The provincial health authority provided mailing labels for all family physicians in Manitoba. Practice demographics were not available so all registered family physicians were contacted and practice patterns were determined as part of the survey. A single mailing of the survey was undertaken, and responses were anonymized by study participant number. A total of 1,000 surveys were administrated. Study personnel subsequently attended the 2016 provincial conference of family physicians to administer the survey to non-respondents of the initial survey in order to increase response rate. No incentive was provided for completing the survey.
Survey responses were analyzed both quantitatively and qualitatively. Qualitative analysis was undertaken of free text questions in order to identify common themes within respondents’ answers. Quantitative analysis was undertaken via descriptive reporting of survey responses and via univariate analysis of PCPs based on referral to the provincial bariatric program. Continuous variables were assessed with Student’s t-test and categorical variables via Chi-square test. A P value of <0.05 was used as the threshold for statistical significance. All statistical analyses were performed using IBM SPSS Statistics Version 25 (IBM Corporation, Armonk, NY, USA).
Results
Of the 1,000 surveys administered, 131 responses were received resulting in a 13.1% response rate. The largest age cohort of PCPs was between 51–60 years old (30.5%). Most respondents were male (57.4%) and the largest proportion of years in practice was between 26–35 years (33.6%). Most respondents worked between 31–40 clinic hours per week (32.1%) and had between 1,000–2,000 patients in their practice (41.4%). A majority of respondents completed their specialty training in Canada (76.0%) and practice within the same provincial health authority as the provincial bariatric program (61.8%). Demographics of the respondents are reported in Table 1.
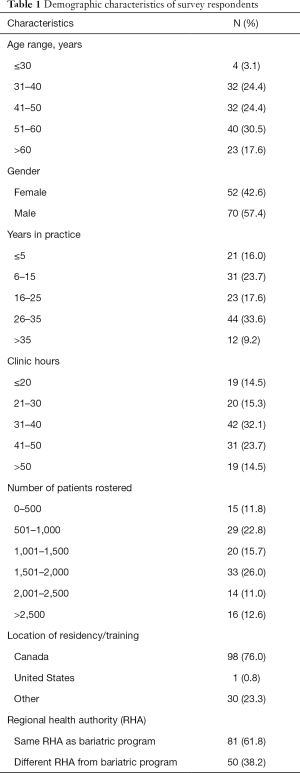
Full table
Table 2 demonstrates the trends of counselling around obesity and its management observed among PCPs. Respondents felt comfortable with counselling non-operative management of obesity (83.1%). However, a majority did not feel that they were well equipped to counsel their patients on bariatric surgery (54.6%). They also did not feel that their residency programs prepared them for the management of bariatric surgery patients (96.2%).The vast majority agreed that they would participate in continuing medical education (CME) to expand their knowledge of bariatric surgery (96.2%) and felt that the best venue for this would be at a session held at their annual provincial meeting for PCPs (41.4%). Most PCPs begin counselling on interventions for obesity at a BMI between 31–35 kg/m2 (45.4%) with the next greater proportion between 36–40 kg/m2 (23.1%; Table 2). The most common counselling performed for patients was diet modification and exercise (94.8%±16.8% and 94.8%±15.0% respectively; Table 3). Counselling for bariatric surgery was used in 11.6%±17.0% of the obese patients in the PCPs’ practice (Table 3). A majority of PCPs do not use the NIH criteria of good candidates for referral to bariatric surgery (74.0%; Table 2).
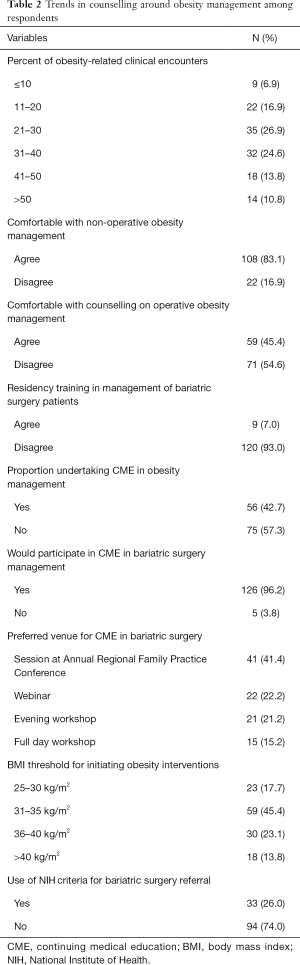
Full table
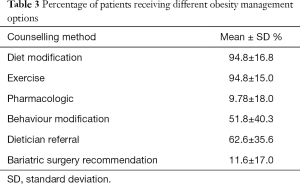
Full table
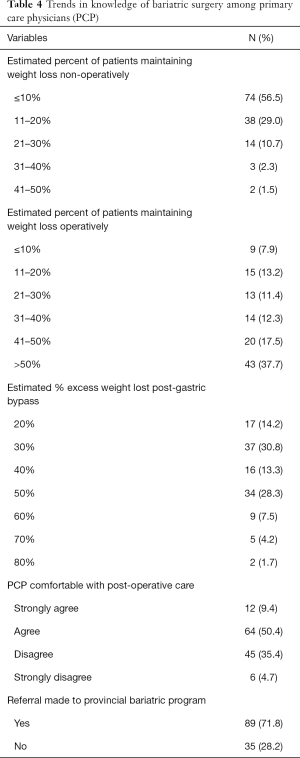
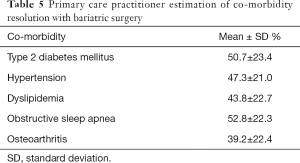
Primary care practitioners had a wide range of estimates on the efficacy of bariatric surgery in maintaining sustained weight loss (Table 4). Additionally, there was large distribution in the estimated percent EWL (%EWL) of laparoscopic roux-en-y gastric bypass, ranging from 20% to 50% EWL (86.6% of respondents; Table 4). Most PCPs were comfortable with providing post-operative care for bariatric surgery patients (59.8%) and a majority had made previous referrals to the provincial program (71.8%; Table 4). PCPs estimated that obstructive sleep apnea, diabetes and hypertension had the highest rates of resolution post-bariatric surgery (52.8%±22.3%, 50.7%±23.4% and 47.3%±21.0% respectively; Table 5).
Full table
Full table
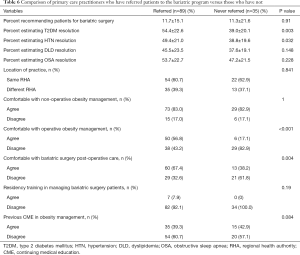
Univariate analysis was performed comparing PCPs who referred patients to the provincial program versus those who had not (Table 6). PCPs with prior referrals to the program estimated higher rates of resolution of diabetes (54.4%±22.6% vs. 39.0%±20.1%; t-test, P=0.003) and hypertension (49.4%±21.0% vs. 38.8%±19.6%; t-test, P=0.032). They were also more comfortable with providing counselling around bariatric surgery as an obesity intervention (56.8% vs. 17.1%; χ2=15.9, P<0.001) and in providing post-operative care (67.4% vs. 38.2%; χ2=8.68; P=0.004). There was no difference in the rates of patients being recommended bariatric surgery based on a PCPs referral patterns. Similarly, referral to the provincial bariatric program did not differ based on practice location, prior residency education in bariatric surgery or previous participation in CME in obesity management.
Full table
Qualitative analysis was performed for the free text question of methods to improve care in the provincial bariatric program. Seven themes were determined from the provided comments. The most common theme was that wait lists were perceived to be too long (33.3% of respondents) followed by improving PCP education around bariatric surgery (30.6%) and that referral thresholds were too high (22.2%). Other less common themes were furthering provincial advocacy for bariatric surgery (5.6%), improving communication between PCP and surgeons (2.8%) and providing patient handouts that could be administered by the PCP (2.8%).
Discussion
This study evaluated the perceptions and referral patterns of primary care practitioners around obesity management and bariatric surgery in a provincially funded bariatric surgery program. Though most respondents were comfortable discussing the non-operative management of obesity with their patients, nearly half felt they could not adequately discuss the role of bariatric surgery. Consequently, PCPs only counsel about 1 in 10 of their obese patients for consideration of bariatric surgery and three quarters of respondents do not follow the NIH criteria for referral for bariatric surgery. Overall underestimates of the potential health benefits and resultant EWL from bariatric surgery suggests a knowledge gap potentially contributing to lower referral rates. Respondents who had referred patients to the provincial bariatric program estimated higher rates of resolution of diabetes and hypertension. They were also more comfortable in pre and postoperative counselling around bariatric surgery. Additionally, one third of respondents felt that better education around bariatric surgery, as well as better access, would improve overall care provided by the provincial bariatric program.
Significant misconceptions persist about the outcomes and perceived risk of bariatric surgery despite its increased use for long term obesity management (6,11,12). Laparoscopic Roux-en-y gastric bypass and laparoscopic vertical sleeve gastrectomy result in EWL of approximately 50–80% (14). Resolution of diabetes, hypertension, hyperlipidemia and sleep apnea are reported as 60–80% with either procedure (15-20). Despite these known outcomes, many PCPs underestimate EWL and co-morbidity resolution at less than 60% (6). A survey of family physicians undertaken in Ontario, Canada, also demonstrates the overestimated risk of bariatric surgery. Of 165 PCPs surveyed, only 10% of respondents correctly identified the 30-day morbidity (0–5%) and mortality (0.1–0.2%) of either laparoscopic vertical sleeve gastrectomy or gastric bypass (21). Overall, our study and the existing body of literature suggest that misconceptions contribute to PCP reluctance to refer for bariatric surgery (6,12,21).
Our study also supports the common theme that education regarding bariatric surgery is lacking for PCPs. A study from 2007 reported that practitioners who completed CME in obesity were more likely to refer their patients for bariatric surgery (12). This study demonstrated that the majority of respondents (54.6%) had not participated in CME in obesity management, but that nearly all (96.2%) would consider it if it was available. This is similar to the survey of Ontario PCPs, where 92.5% felt that CME would be a useful endeavour (21). Respondents in our survey felt that education was one of the biggest barriers to care and believed a session in bariatric surgery at the annual provincial family practice meeting would be the most effective method of CME.
CME for practicing physicians is an invaluable tool for addressing knowledge gaps and disseminating new medical information. However, time constraints and other non-clinical responsibilities likely limit their efficacy. Educational interventions during residency training may be of more significant benefit. Ninety-three percent of respondents in our study did not receive training in bariatric surgery during residency. Many respondents were older and therefore might have completed their formal training before the emergence of laparoscopic bariatric surgery as a safe and effective treatment for obesity. However, a third of respondents would have completed residency in the last 5 years. A study out of Massachusetts General Hospital previously reported the results of a survey of PCPs with at least 1 hour of obesity training versus those without. They found that those with training scored higher on knowledge assessments of bariatric surgery and were more likely to be confident in treating obesity (22). Unfortunately, a survey of 99 clerkship directors in the US and Canada has demonstrated that time constraints limit the adoption of obesity teaching and that bariatric surgery only makes up 17.9% of the obesity curriculum. Their study also reported that most (59%) clerkship directors had no plans to change their existing curricula (23). Our own institution can echo this as we have seen no change in the annual regional referral rate since performing this survey. This is unfortunate as increasing education around obesity and bariatric surgery in undergraduate and postgraduate medical education could be an effective intervention to improve PCP knowledge and positively impact the future care of patients living with obesity.
Study respondents also identified access to care as a significant perceived barrier for referral to bariatric surgery. Our study did not demonstrate an effect of location on attitude or referral pattern to the bariatric program. This is an important finding in a province with wide variation in population density and geographic proximity to health care. The biggest concern for care among respondents was the lengthy waitlist associated with referral to the provincial program. Wait times were previously as high as 5 years in Manitoba but have now improved to 1 to 2 years. This is in line with previously reported wait lists for bariatric surgery in Canada from over a decade ago (24). Greater communication to PCPs about accurate wait times is another strategy to improve referral patterns.
This study has several limitations. The response rate was approximately 10%. We had access to mailing addresses for all PCPs in Manitoba but we were not able to distinguish by practice type or volume for the survey administration. We were also unable to assess differences between respondents and non-respondents in order to mitigate this potential confounder. This makes it difficult to determine whether our respondent sample was representative of the family physician base. The low response rate might also reflect the voluntary nature of the survey. The retrospective nature of the study also relied on recall of practice patterns with inherent bias. Additionally, it was cost prohibitive to perform a second round of surveys as we had to rely on paper mail out and could not identify specific practice patterns for more directed mailing. Despite these limitations, we feel the information reported remains important in understanding how obesity management and bariatric surgery is viewed among family physicians in this provincially funded bariatric surgery program.
Conclusions
Laparoscopic bariatric surgery remains a safe and effective means of obesity management. This survey of PCPs reiterates the knowledge deficit that has been reported in previous investigations of bariatric programs. Education around comprehensive obesity management including bariatric surgery is one of the largest identified barriers in caring for individuals living with obesity. CME activities targeted to PCPs offer an opportunity to address this concern. Furthermore, adoption of a modernized obesity management curriculum in medical school and family practice specialty training represents an important method of tackling the knowledge deficit for current trainees.
Supplementary
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Muhammed Ashraf Memon) for the focused issue “Bariatric Surgery” published in Annals of Translational Medicine. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: The focused issue “Bariatric Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional research ethics board [No. HS19101 (H2015:418)].
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Public Health Agency of Canada. Obesity in Canada: A joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. Ottawa, 2011.
- Avidor Y, Still CD, Brunner M, et al. Primary care and subspecialty management of morbid obesity: Referral patterns for bariatric surgery. Surg Obes Relat Dis 2007;3:392-407. [Crossref] [PubMed]
- Deitel M. Overweight and obesity worldwide now estimated to involve 1.7 billion people. Obes Surg 2003;13:329-30. [Crossref] [PubMed]
- Afonso BB, Rosenthal R, Li KM, et al. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis 2010;6:16-21. [Crossref] [PubMed]
- Li Z, Bowerman S, Heber D. Health ramifications of the obesity epidemic. Surg Clin North Am 2005;85:681-701. [Crossref] [PubMed]
- Perlman SE, Reinhold RB, Nadzam GS. How do family practitioners perceive surgery for the morbidly obese? Surg Obes Relat Dis 2007;3:428-33. [Crossref] [PubMed]
- Wadden TA, Anderson DA, Foster GD, et al. Obese women’s perceptions of their physicians’ weight management attitudes and practices. Arch Fam Med 2000;9:854-60. [Crossref] [PubMed]
- Galuska DA, Will JC, Serdula MK, et al. Are health care professionals advising obese patients to lose weight? JAMA 1999;282:1576-8. [Crossref] [PubMed]
- Padwal RS, Damjanovic S, Schulze KM, et al. Canadian Physicians' Use of Antiobesity Drugs and Their Referral Patterns to Weight Management Programs or Providers: The SOCCER Study. J Obes 2011;2011:686521.
- Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240:416-24. [Crossref] [PubMed]
- Bardia A, Holtan SG, Slezak JM, et al. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc 2007;82:927-32. [Crossref] [PubMed]
- Balduf LM, Farrell TM. Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res 2008;144:49-58. [Crossref] [PubMed]
- Ferrante JM, Piasecki AK, Ohman-Strickland PA, et al. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity 2009;17:1710-6. [Crossref] [PubMed]
- Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014.CD003641. [PubMed]
- Osland E, Yunus RM, Khan S, et al. Diabetes improvement and resolution following laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: A systematic review of randomized controlled trials. Surg Endosc 2017;31:1952-63. [Crossref] [PubMed]
- Schiavon CA, Bersch-Ferreira AC, Santucci EV, et al. Effects of Bariatric Surgery in Obese Patients With Hypertension. Circulation 2018;137:1132-42. [Crossref] [PubMed]
- Cazzo E, Gestic MA, Utrini MP, et al. Control of hypertension after roux-en-y gastric bypass among obese diabetic patients. Arq Gastroenterol 2014;51:21-4. [Crossref] [PubMed]
- Sillo TO, Lloyd-Owen S, White E, et al. The impact of bariatric surgery on the resolution of obstructive sleep apnoea. BMC Res Notes 2018;11:385. [Crossref] [PubMed]
- Varela JE, Hinojosa MW, Nguyen NT. Resolution of obstructive sleep apnea after laparoscopic gastric bypass. Obes Surg 2007;17:1279-82. [Crossref] [PubMed]
- Nguyen NT, Varela E, Sabio A, et al. Resolution of hyperlipidemia after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg 2006;203:24-9. [Crossref] [PubMed]
- Auspitz M, Cleghorn MC, Azin A, et al. Knowledge and perception of bariatric surgery among primary care physicians: A survey of family doctors in Ontario. Obes Surg 2016;26:2022-8. [Crossref] [PubMed]
- Stanford FC, Johnson ED, Claridy MD, et al. The Role of Obesity Training in Medical School and Residency on Bariatric Surgery Knowledge in Primary Care Physicians. Int J Family Med 2015;2015:841249.
- Holman H, Dey S, Drobish I, et al. Obesity education in the family medicine clerkship: A US and Canadian survey of clerkship directors’ beliefs, barriers, and curriculum content. BMC Med Educ 2019;19:169. [Crossref] [PubMed]
- Christou N V, Efthimiou E. Bariatric surgery waiting times in Canada. Can J Surg 2009;52:229-34. [PubMed]