Static progressive stretch orthosis—consensus modality to treat knee stiffness—rationale and literature review
Introduction
Following knee procedures, such as total knee arthroplasty, arthroscopy anterior cruciate ligament reconstruction, or traumatic events, a percentage of patients are “at risk” for developing post-operative fibrosis and stiffness (1-3). These patients typically require additional physical therapies, rehabilitation, and use of adjunctive mechanical stretch devices to improve their range of motion (ROM) and functional outcome. The literature has shown that the earlier these patients are identified, and the earlier the adjunctive mechanical stretch devices can be prescribed, the better the outcomes can be (4). However, if these patients are identified late, they risk chronic contracture, prolonged recovery, and potential lack of full functional improvement. Therefore, identifying these patients early and starting them on appropriate adjunctive therapies, such as mechanical stretch bracing, are critical elements for successful outcomes. Additionally, early initiation of adjunctive devices can potentially result in fewer physical therapy visits, and the visits that do occur, might be more effective for the patients. Furthermore, because the adjunctive ROM therapies can be delivered at home on a repeated and daily basis rather than through outpatient therapy visits, patients are more likely to be compliant and therefore have increased odds for improved ROM and recovery (5-7).
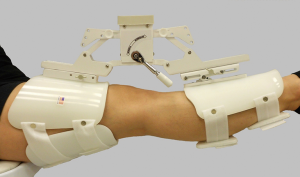
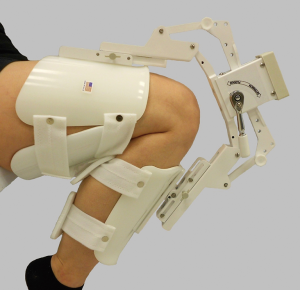
One of the first lines of treatment for these patients is to actively work on ROM to restore function. Active ROM is important for long term strength and functional results, and needs to be emphasized as opposed to passive ROM (8). It is well-documented that physical therapy helps restore ROM. Physical therapy and patient active exercise are considered first-line treatment for restoring joint ROM. However, when patients are not responding or plateau with motion improvement in physical therapy, then adjunctive bracing can be a low cost and benign treatment option. Adjunctive bracing can provide the appropriate amount of force over time, i.e., appropriate “clinical dosage” of stretch of the soft tissues to improve ROM. Bracing types for the knee typically include dynamic and static progressive stretch (SPS) devices. Dynamic braces apply a low intensity, constant load over extended periods of time (i.e., 8 to 12 hours) across the joint and usually requires 2 devices, one for each direction. However, given the low load, this bracing option can be very slow and inefficient, requiring months of continued therapy. SPS (Figures 1,2) bracing applies an incrementally adjusted static load, which can promote both relaxation and elongation of the joint tissues. SPS braces are applied for up to 30 minutes, 2 to 3 times per day, considerably less time compared to 8- to 12-hour Dynamic brace protocols, and SPS devices are typically bi-directional, requiring only one device for treatment of both directions of motion. These devices have been designed to simulate the work of a therapist, such that for the knee, a force is applied at the proximal femur and distal tibia in the plane of joint motion, but with the patient in control of how much force to apply. SPS braces can provide the appropriate amount of force over time, i.e., appropriate “clinical dosage” of stretch of the soft tissue to improve ROM.
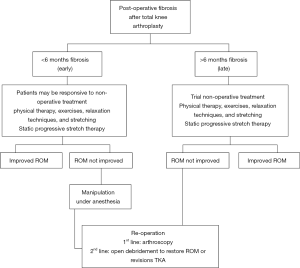
Although these different bracing types exist, there is no generalized consensus on superiority. One bracing modality, SPS, however, has been shown to be potentially more promising and is considered the standard of care for knee fibrosis. In fact, the recent international consensus on the management of knee fibrosis identified static progressive splints as a cornerstone of management (Figure 3) (9). However, despite its widespread clinical acceptance, treatment protocols for SPS therapy are subjective, variable, and potentially sub-optimally utilized across the rehabilitation community. Therefore, the purpose of this paper was to review the evidence on SPS therapy in order to determine if there is rationale to support its acceptance as the optimal and standard of care treatment approach for knee fibrosis and joint motion loss. Specifically, we: (I) describe the biomechanics of SPS; (II) detail recent literature on this adjunctive therapy for the knee; and (III) recommend optimal evidence-based treatment protocols for SPS in order to standardize effective treatment for post-operative knee fibrosis in the rehabilitation community.
Methods
A systematic PubMed literature search was performed to identify studies on SPS braces for all joints, including the elbow, knee, and shoulder joints. Boolean operators, along with the following search terms were utilized to query the index: “brace”, “static”, “progressive”, “knee”, “joint”, “consensus”, “protocol”, “fibrosis”, “biomechanics”, and “total end-range time”.
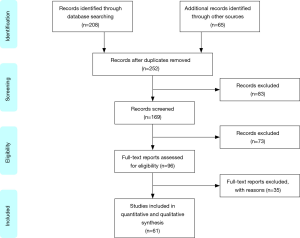
The initial search resulted in 273 studies (Figure 4). Two authors (*, **) conducted the initial search and screened the titles and abstracts of identified articles in order to identify those that were most pertinent to the study aims. After this initial screening process, the full-text of selected articles were evaluated, in addition to references from all included studies. Studies were included if they addressed clinical outcomes, relied primarily on the brace for improvement of patient outcomes and not on surgery or physical therapies, described treatment protocols, and were written in English. Individually-fabricated braces were not included in our analysis, because these can be costly and are customized to a single patient. Therefore, the results from these braces are not as generalizable as compared to universal braces. After exclusionary criteria were considered, 61 studies were included for analysis.
Studies were evaluated to determine if there is rationale to support the acceptance of SPS as the optimal and standard of care treatment approach for knee fibrosis and joint motion loss. Specifically, definitions, descriptions, and, recommended optimal evidence-based treatment protocols for SPS are reported in order to help standardize effective treatment for post-operative knee fibrosis in the rehabilitation community. Additionally, correlative and comparative findings from each study are reported in addition to a summative discussion relating study findings to clinical practice recommendations.
Results
Biomechanics of SPS
The “total end-range time”, or TERT, principle states that the increase in passive ROM in stiff joints is directly proportional to the time the joint is held at the end of range (10). Therefore, TERT is determined by multiplying the frequency and duration of time spent at end-range daily (11). The TERT dose necessary to increase range-of-motion varies by the condition of each joint. This is comprised of, the duration, frequency, and intensity of the force, which also play critical roles (12).
The duration of force is the amount of time tissues are held in a stretched position. Duration is calculated based on the amount of time applied per day, e.g., 4 sessions of 30 minutes each session is a TERT of 120 minutes. The duration of low stress force must be applied long enough to produce biologic remodeling of joint tissues, which results in tissue elongation. High stress, short duration loading has a greater risk of exceeding pain limits and/or producing tissue tearing and injury.
Frequency has two components: daily and weekly. Intensity is the amount of force applied by the splint or device. Inadequate intensity may result in a temporary or elastic tissue response with little or no gain in range-of-motion. Excessive intensity can result in ischemia or microscopic tears which stimulate inflammation and pain. Because patients experience stretch before they feel pain, intensity is usually limited by the patient’s pain tolerance.
SPS technology was pioneered by Joint Active Systems (JAS) (Effingham, Illinois), with principles of open architecture, triangulation, patient directed force, and short treatment protocols (up to 30 minutes) to stretch tissue and increase range-of-motion. SPS devices use inelastic components to apply stress-relaxation (SR) loading to stiff tissues (13). SR is the force load that also forms the basis for manual therapy stretching techniques. Stress relaxation loading utilizes a low-intensity force to position a joint at its end ROM and hold joint tissues at their maximal therapeutic length (14). It is a constant displacement variable force, so that the tissue is stretched to a maximal position, then the force drops over time, resulting in relaxation. This action allows maximum time at the end ROM to optimize tissue lengthening. One device (JAS SPS) avoids direct contact with the knee allows immediate post-operative use as needed. The device is a single plane that triangulated the force, so that it is always applied in the angle of the joint through ROM, as opposed to hinges at the joint, which force the joint to follow a mechanical hinge that is non-anatomic.
As tissues lengthen in response to the applied stress, the SPS device is adjusted to position the joint tissues at their new maximal therapeutic length, which can increase ROM (15,16). This process of stretching and holding is repeated several times during a treatment session, and sessions are performed daily to improve tissue elasticity and achieve plastic deformation to lengthen soft tissue. Stretching with an orthosis does not cause the tissue to lengthen by growing. The only time tissue can grow by lengthening is when the tissue has been cut and then stressed. Stretching the tissue in its plastic ROM can help restore ROM. Therefore, the dose in therapy or the force over time is critical. SPS braces can apply an adequate force to get tissue through its plastic ROM to optimize stretching.
Recent literature
Our search yielded over 50 publications on SPS use, with 13 references to use in patients with knee pathologies (9,13,17-39) (Table 1). The studies consisted of prospectively and retrospectively collected data, reporting on patient outcomes following SPS use (40-63).
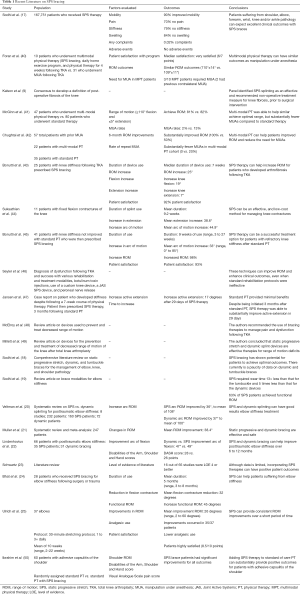
Full table
McGinn et al. compared 47 patients who received a combined innovative multi-modal physical therapy (IMMPT) regimen that included standard of care plus SPS bracing and neuromuscular electrical stimulation to 80 patients who underwent standard of care therapy alone (41). All patients were post primary total knee arthroplasty. The group found the IMMPT and control cohorts achieved a similar desired ROM (≥110 degrees flexion and ≤5 degrees extension). However, the IMMPT cohort had substantially fewer patients require manipulation under anesthesia (2% vs. 13%). A similar study compared 57 total patients who underwent manipulation under anesthesia following total knee arthroplasty (42). A total of 22 of these patients underwent multi-modal physical therapy, which included SPS bracing and standard physical therapy, while the remaining 35 underwent standard physical therapy alone. After 6 months, 100% of patients in the multi-modal cohort achieved desired ROM, while only 50% of patients (P=0.005) in the standard physical therapy cohort achieved the same outcome. Furthermore, patients in the multi-modal cohort achieved a statistically significant higher mean flexion ROM as compared to those who were in the standard of care group (116 vs. 106; P=0.005).
Another study evaluated 25 patients who underwent TKA and had persistent knee stiffness without improvement after standard therapy were then treated with SPS bracing (43). After a median of 7 weeks (range, 3–16 weeks), the median increase in ROM was 25 degrees (range, 8–82 degrees), the median gain in knee active flexion was 19 degrees (range, 5–80 degrees), and 92% of patients reported that they were satisfied with their results.
Suksathien et al. evaluated 11 patients who underwent SPS treatment for knee flexion contractures, and found after 9 weeks, the mean increase in knee extension was 38.6 degrees, and the average arc of motion increased by 44.9 degrees (44). Another study by Bonutti et al. evaluated 41 patients treated with SPS therapy and found after 9 weeks of use, total arc of motion increased by a mean of 33 degrees (range, 0–85 degrees) (45). An increase in motion was also seen in 98% of patients, and 93% of patients with satisfied with their outcomes. Importantly, compared to the literature, the positive outcomes occurred at a shorter mean treatment time than for historic controls.
The use of SPS therapy has also been found to be effective for other joints, such as the elbow, shoulder, wrist/forearm and ankle. In one of the largest studies to date, 167,751 who were treated with SPS bracing were evaluated over a 10-year period (17). Outcomes measured were: (I) mobility; (II) pain; (III) stiffness; (IV) swelling; and (V) any adverse events of patients treated with an SPS brace. The group found that patients who utilized the brace consistently reported excellent (roughly 90%) improvements in mobility, with only a small portion (<10%) of patients reporting no improvements. Comparing pain, patients continuously reported decreasing pain, with over 70% of patients reporting no pain at final follow up. Similarly, for stiffness, at final follow up, 84% of patients reported no stiffness. For swelling as well, 84% of patients reported no joint swelling after SPS therapy use. Importantly, during the most recent year, only three patients (0.02%) reported any device complaints. Throughout the 10-year study period, none of the 167,751 patients experienced any device related serious injuries.
Based on the above data, it is clear that SPS therapy has a critical role in the management of knee pathologies. Particularly patients suffering from knee fibrosis have been found to achieve substantial improvements in function and ROM. This treatment type is also simple and easy to use, so can be utilized widely for all types of patients.
Recommended protocol
Given the proven and optimal biomechanics behind the design of the SPS brace and the clinical evidence suggesting efficacy, there is a clear need for a standardized protocol for this therapy. Some studies report protocols for patients to participate in daily treatment sessions for the first 5 days of treatment (43). These treatment sessions then increase to a maximum of 3 treatment sessions per day. Patients then continued this protocol for up to 7 weeks (range, 3–16 weeks). Another study followed a similar protocol, except patients continued therapy until no further improvements were seen for at least 1 week. In this study, patients underwent treatment for a mean of 9 weeks (range, 3–27 weeks) (45).
Based on the reported literature, patients should utilize SPS therapy for 5-minute incremental stretches for up to a 30-minute session applied up to 3 times per day. The force applied is best determined by the patient as each joint or stiffness varies and patient has full control to adjust the force to tolerance. The goal is to avoid pain, while achieving the maximum stretch tolerable. The therapy should be continued for as long as the patient experiences improvements, which is likely around 8 weeks, though in cases of chronic stiffness/contracture, might be longer (8 to 12 weeks).
Critical to success is early identification and initiation of brace use, prior to the onset of fibrotic tissue buildup. Importantly, as is recommended by the recent consensus on the definition and classification of fibrosis, it is critical to identify these patients early, and begin intervention promptly. Managing patients with SPS bracing within the first 12 weeks (i.e., those with stiffness), when connective tissues are most responsive to remodeling, instead of those with chronic contractures (>6 months) can yield more optimal results. The longer a patient waits, the more connective tissue remolding and fibrotic development, the less progress can potentially be made. In any case, SPS braces should be utilized in cases of acute or chronic fibrosis prior to any surgical procedures.
Conclusions
Improving ROM is critical to optimize function in patients following knee surgery, injury, arthroplasty, or any other traumatic events. SPS therapies have clearly shown to have meaning benefits in the number of clinical trials that report on their effects on patient outcomes. The recent consensus on knee fibrosis also recommends that patients with acute or chronic knee fibrosis utilize SPS therapy as a standard of care prior to any surgical intervention. However, to date, there a standardized protocol of use for SPS knee braces has not been reported. We recommend sessions lasting 5 to 30 minutes, up to 3 times per day. Additionally, it is important to realize that the earlier the device is utilized, the better results patients can expect. Providers should note if patients are not making appropriate gains in ROM through other therapeutic measures, SPS can be used earlier for potentially better and faster results. Although these braces can be effective at any time point, identifying patient need within the first 12 weeks (i.e., those with stiffness) instead of those with chronic contractures (>6 months) can yield enhanced outcomes. Adjunctive utilization of SPS therapy can help patients achieve optimal ROM and function, and should be part of routine care when managing patients with knee fibrosis.
Acknowledgments
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Abdul N, Dixon D, Walker A, et al. Fibrosis is a common outcome following total knee arthroplasty. Sci Rep 2015;5:16469. [Crossref] [PubMed]
- Huleatt J, Gottschalk M, Fraser K, et al. Risk Factors for Manipulation Under Anesthesia and/or Lysis of Adhesions After Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med 2018;6:2325967118794490. [Crossref] [PubMed]
- Schiavone Panni A, Cerciello S, Vasso M, et al. Stiffness in total knee arthroplasty. J Orthop Traumatol 2009;10:111-8. [Crossref] [PubMed]
- Fitzsimmons SE, Vazquez EA, Bronson MJ. How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res 2010;468:1096-106. [Crossref] [PubMed]
- Deyle GD, Allison SC, Matekel RL, et al. Physical Therapy Treatment Effectiveness for Osteoarthritis of the Knee: A Randomized Comparison of Supervised Clinical Exercise and Manual Therapy Procedures Versus a Home Exercise Program. Phys Ther 2005;85:1301-17. [PubMed]
- Coke T, Alday R, Biala K, et al. The new role of physical therapy in home care. Home Healthc Nurse 2005;23:594-9. [Crossref] [PubMed]
- Tao X, Chow SKY, Wong FK. The effects of a nurse-supervised home exercise programme on improving patients’ perceptions of the benefits and barriers to exercise: A randomised controlled trial. J Clin Nurs 2017;26:2765-75. [Crossref] [PubMed]
- Song YD, Jain N, Kang YG, et al. Active Flexion in Weight Bearing Better Correlates with Functional Outcomes of Total Knee Arthroplasty than Passive Flexion. Knee Surg Relat Res 2016;28:118-29. [Crossref] [PubMed]
- Kalson NS, Borthwick LA, Mann DA, et al. International consensus on the definition and classification of fibrosis of the knee joint. Bone Joint J 2016;98-B:1479-88. [Crossref] [PubMed]
- Flowers KR, LaStayo P. Effect of total end range time on improving passive range of motion. J Hand Ther 1994;7:150-7. [Crossref] [PubMed]
- Kelley MJ, McClure PW, Leggin BG. Frozen shoulder: evidence and a proposed model guiding rehabilitation. J Orthop Sports Phys Ther 2009;39:135-48. [Crossref] [PubMed]
- Jacobs CA, Sciascia AD. Factors that influence the efficacy of stretching programs for patients with hypomobility. Sports Health 2011;3:520-3. [Crossref] [PubMed]
- Bonutti PM, Windau JE, Ables BA, et al. Static progressive stretch to reestablish elbow range of motion. Clin Orthop Relat Res 1994.128-34. [PubMed]
- McHugh MP, Magnusson SP, Gleim GW, et al. Viscoelastic stress relaxation in human skeletal muscle. Med Sci Sports Exerc 1992;24:1375-82. [Crossref] [PubMed]
- Cyr LM, Ross RG. How controlled stress affects healing tissues. J Hand Ther 1998;11:125-30. [Crossref] [PubMed]
- Frost HM. Skeletal structural adaptations to mechanical usage (SATMU): 1. Redefining Wolff’s law: the bone modeling problem. Anat Rec 1990;226:403-13. [Crossref] [PubMed]
- Sodhi N, Yao B, Anis HK, et al. Patient satisfaction and outcomes of static progressive stretch bracing: a 10-year prospective analysis. Ann Transl Med 2019;7:67. [Crossref] [PubMed]
- Sodhi N, Yao B, Khlopas A, et al. A Case for the Brace: A Critical, Comprehensive, and Up-To-Date Review of Static Progressive Stretch, Dynamic, and Turnbuckle Braces for the Management of Elbow, Knee, and Shoulder Pathology. Surg Technol Int 2017;31:303-18. [PubMed]
- Sodhi N, Khlopas A, Vaughn MD, et al. Manufactured Brace Modalities for Elbow Stiffness. Orthopedics 2018;41:e127-35. [Crossref] [PubMed]
- Veltman ES, Doornberg JN, Eygendaal D, et al. Static progressive versus dynamic splinting for posttraumatic elbow stiffness: a systematic review of 232 patients. Arch Orthop Trauma Surg 2015;135:613-7. [Crossref] [PubMed]
- Müller AM, Sadoghi P, Lucas R, et al. Effectiveness of bracing in the treatment of nonosseous restriction of elbow mobility: a systematic review and meta-analysis of 13 studies. J Shoulder Elbow Surg 2013;22:1146-52. [Crossref] [PubMed]
- Lindenhovius AL, Doornberg JN, Brouwer KM, et al. A prospective randomized controlled trial of dynamic versus static progressive elbow splinting for posttraumatic elbow stiffness. J Bone Joint Surg Am 2012;94:694-700. [Crossref] [PubMed]
- Schwartz DA. Static progressive orthoses for the upper extremity: a comprehensive literature review. Hand (N Y) 2012;7:10-7. [Crossref] [PubMed]
- Bhat AK, Bhaskaranand K, Nair SG. Static progressive stretching using a turnbuckle orthosis for elbow stiffness: a prospective study. J Orthop Surg (Hong Kong) 2010;18:76-9. [Crossref] [PubMed]
- Ulrich SD, Bonutti PM, Seyler TM, et al. Restoring range of motion via stress relaxation and static progressive stretch in posttraumatic elbow contractures. J Shoulder Elbow Surg 2010;19:196-201. [Crossref] [PubMed]
- Doornberg JN, Ring D, Jupiter JB. Static progressive splinting for posttraumatic elbow stiffness. J Orthop Trauma 2006;20:400-4. [Crossref] [PubMed]
- Gelinas JJ, Faber KJ, Patterson SD, et al. The effectiveness of turnbuckle splinting for elbow contractures. J Bone Joint Surg Br 2000;82:74-8. [Crossref] [PubMed]
- Green DP, McCoy H. Turnbuckle orthotic correction of elbow-flexion contractures after acute injuries. J Bone Joint Surg Am 1979;61:1092-5. [Crossref] [PubMed]
- Nandi S, Maschke S, Evans PJ, et al. The stiff elbow. Hand (N Y) 2009;4:368-79. [Crossref] [PubMed]
- Issack PS, Egol KA. Posttraumatic contracture of the elbow: current management issues. Bull Hosp Jt Dis 2006;63:129-36. [PubMed]
- Charalambous CP, Morrey BF. Posttraumatic elbow stiffness. J Bone Joint Surg Am 2012;94:1428-37. [Crossref] [PubMed]
- Evans PJ, Nandi S, Maschke S, et al. Prevention and Treatment of Elbow Stiffness. J Hand Surg Am 2009;34:769-78. [Crossref] [PubMed]
- Kim PD, Grafe MW, Rosenwasser MP. Elbow Stiffness: Etiology, Treatment, and Results. J Am Soc Surg Hand 2005;5:209-16. [Crossref]
- Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am 1998;80:1603-15. [Crossref] [PubMed]
- Phillips BB, Strasburger S. Arthroscopic treatment of arthrofibrosis of the elbow joint. Arthroscopy 1998;14:38-44. [Crossref] [PubMed]
- Ring D, Jupiter JB. Fracture-dislocation of the elbow. J Bone Joint Surg Am 1998;80:566-80. [Crossref] [PubMed]
- Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am 1990;72:601-18. [Crossref] [PubMed]
- McGrath MS, Ulrich SD, Bonutti PM, et al. Static progressive splinting for restoration of rotational motion of the forearm. J Hand Ther 2009;22:3-8. [Crossref] [PubMed]
- Lucado AM, Li Z. Static progressive splinting to improve wrist stiffness after distal radius fracture: a prospective, case series study. Physiother Theory Pract 2009;25:297-309. [Crossref] [PubMed]
- Foran J, Stevens-Lapsley J, Bade M. Multimodal conservative management of stiffness after total knee arthroplasty: A pilot study with retrospective historical cohort comparison. In: Combined Sections Meeting of the APTA, 2019.
- McGinn T, Chughtai M, Bhave A, et al. Innovative Multi-Modal Physical Therapy Reduces Incidence of Manipulation Under Anesthesia (MUA) in Non-Obese Primary Total Knee Arthroplasty. Surg Technol Int 2016;29:328-33. [PubMed]
- Chughtai M, McGinn T, Bhave A, et al. Innovative Multimodal Physical Therapy Reduces Incidence of Repeat Manipulation under Anesthesia in Post-Total Knee Arthroplasty Patients Who Had an Initial Manipulation under Anesthesia. J Knee Surg 2016;29:639-44. [Crossref] [PubMed]
- Bonutti PM, Marulanda GA, McGrath MS, et al. Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2010;18:194-9. [Crossref] [PubMed]
- Suksathien R, Suksathien Y. A new static progressive splint for treatment of knee and elbow flexion contractures. J Med Assoc Thai 2010;93:799-804. [PubMed]
- Bonutti PM, McGrath MS, Ulrich SD, et al. Static progressive stretch for the treatment of knee stiffness. Knee 2008;15:272-6. [Crossref] [PubMed]
- Seyler TM, Marker DR, Bhave A, et al. Functional problems and arthrofibrosis following total knee arthroplasty. J Bone Joint Surg Am 2007;89 Suppl 3:59-69. [PubMed]
- Jansen CM, Windau JE, Bonutti PM, et al. Treatment of a knee contracture using a knee orthosis incorporating stress-relaxation techniques. Phys Ther 1996;76:182-6. [Crossref] [PubMed]
- McElroy MJ, Johnson AJ, Zywiel MG, et al. Devices for the prevention and treatment of knee stiffness after total knee arthroplasty. Expert Rev Med Devices 2011;8:57-65. [Crossref] [PubMed]
- Millett PJ, Johnson B, Carlson J, et al. Rehabilitation of the arthrofibrotic knee. Am J Orthop (Belle Mead NJ) 2003;32:531-8. [PubMed]
- Ibrahim M, Donatelli R, Hellman M, et al. Efficacy of a static progressive stretch device as an adjunct to physical therapy in treating adhesive capsulitis of the shoulder: a prospective, randomised study. Physiotherapy 2014;100:228-34. [Crossref] [PubMed]
- Lucado AM, Li Z, Russell GB, et al. Changes in impairment and function after static progressive splinting for stiffness after distal radius fracture. J Hand Ther 2008;21:319-25. [Crossref] [PubMed]
- McGrath MS, Ulrich SD, Bonutti PM, et al. Evaluation of static progressive stretch for the treatment of wrist stiffness. J Hand Surg Am 2008;33:1498-504. [Crossref] [PubMed]
- Parent-Weiss NM, King JC. Static progressive forearm rotation contracture management orthosis design: a study of 28 patients. J Prosthet Orthot 2006;18:63-7. [Crossref]
- Smith DW, Brou KE, Henry MH. Early active rehabilitation for operatively stabilized distal radius fractures. J Hand Ther 2004;17:43-9. [Crossref] [PubMed]
- Bell SN, Benger D. Management of radioulnar synostosis with mobilization, anconeus interposition, and a forearm rotation assist splint. J Shoulder Elbow Surg 1999;8:621-4. [Crossref] [PubMed]
- Hussein AZ, Ibrahim MI, Hellman MA, et al. Static progressive stretch is effective in treating shoulder adhesive capsulitis: Prospective, randomized, controlled study with a two-year follow-up. Eur J Physiother 2015;17:138-47. [Crossref]
- Ibrahim MI, Johnson AJ, Pivec R, et al. Treatment of adhesive capsulitis of the shoulder with a static progressive stretch device: a prospective, randomized study. J Long Term Eff Med Implants 2012;22:281-91. [Crossref] [PubMed]
- Johnson AJ, McKenzie SA, Ulrich SD, et al. Assessment of static progressive stretch for the treatment of shoulder stiffness: a prospective case series. J Long Term Eff Med Implants 2012;22:293-303. [Crossref] [PubMed]
- Donatelli R, Ruivo RM, Thurner M, et al. New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Phys Ther Sport 2014;15:3-14. [Crossref] [PubMed]
- LaStayo P, Jaffe R. Assessment and management of shoulder stiffness: a biomechanical approach. J Hand Ther 1994;7:122-30. [Crossref] [PubMed]
- Costa CR, McElroy MJ, Johnson AJ, et al. Use of a static progressive stretch orthosis to treat post-traumatic ankle stiffness. BMC Res Notes 2012;5:348. [Crossref] [PubMed]
- Sharma NK, Loudon JK. Static progressive stretch brace as a treatment of pain and functional limitations associated with plantar fasciitis: a pilot study. Foot Ankle Spec 2010;3:117-24. [Crossref] [PubMed]
- Grissom SP, Blanton S. Treatment of upper motoneuron plantarflexion contractures by using an adjustable ankle-foot orthosis. Arch Phys Med Rehabil 2001;82:270-3. [Crossref] [PubMed]