Anti-atherosclerotic effects between a combined treatment with simvastatin plus hirudin and single simvastatin therapy in patients with early type 2 diabetes mellitus
Introduction
Type 2 diabetes mellitus (T2DM) is a common disease worldwide, and it has been estimated that there will be more than 640 million people with T2DM in 2040 (1). T2DM is characterized by a functional and metabolic milieu that prominently promotes the development of atherosclerosis, which not only impairs the quality of life but also increases the risks of cardiovascular diseases and related death (2). Some factors (including the coagulation cascade) have been well elaborated to participate in the progression of atherosclerotic disease, involving the endothelial function, platelet and monocyte adhesiveness, macrophage function and fibrinolysis. They are adversely associated with an inflammatory reaction to the lipid deposition (3) in the innermost layer and large-caliber artery, which leads to a pro-thrombotic environment, further exacerbating the atherothrombosis (4). The role of the coagulation cascade in the vascular pathology in case of atherosclerosis has been a focus in biomedical researches on T2DM, and treatment targeting the coagulation cascade may be helpful for the prevention of stroke relevant mortality (5). The high frequency ultrasound has become a promising tool in the early prevention and treatment of atherosclerosis due to earlier detection and accurate location of atherosclerosis.
Statins are HMG-CoA reductase inhibitors (such as simvastatin) and have been used to reduce low-density lipoprotein cholesterol (LDL-C) by inhibiting 3-hydroxy-3-methylglutaryl-coenzyme, leading to a proportionate reduction in the risk of cardiovascular diseases (6). Recent studies have indicated simvastatin can effectively and safely improve the dyslipidemia and reduce the macrophage activation in the advanced atherosclerotic plaques (7). Although beneficial effects of statins have been well shown, they are still associated with a 1.9 to 2.6 folds risk for new-onset diabetes in Asian patients (8). Furthermore, treatment with a statin usually fails to achieve at least 30% to 50% reduction in LDL-C (9). Because clot formation participates in the formation of atherosclerotic plaques and may stimulate the proliferation of arterial smooth muscle cells in T1DM and T2DM (4), the addition of anticoagulants to statins may be helpful for the anti-arteriosclerotic treatment. It has been confirmed that the hirudin, a specific thrombin inhibitor, may exert anti-arteriosclerotic effects (10). This study was to investigate the safety and anti-atherosclerotic effects of simvastatin vs simvastatin plus hirudin in patients with early T2DM.
Methods
Participants
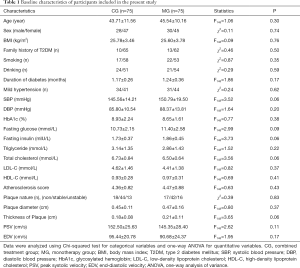
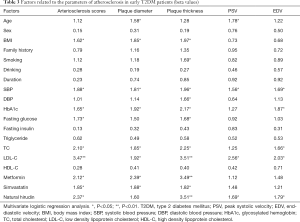
Patients were recruited from three centers (First Affiliated Hospital of Zhejiang University, Tongde Hospital of Zhejiang Province and Xiaoying Street Community Health Center) between March 2014 and July 2019. A total of 150 subjects initially diagnosed with T2DM according to the International Classification of Diseases-10 Version were included in the present study. In these patients, at least one of triglycerides, total cholesterol (TC), and LDL-C was higher than normal. Exclusion criteria were as follows: (I) patients had any significant condition affecting the pharmacokinetics of hirudin, simvastatin and anti-diabetic drugs (such as sulfonylureas); (II) patients had a family history of hypersensitivity to hirudin or statins; (III) patients had specific complications of the heart, liver (the blood alanine amino transferases higher than 80 U/L) or kidney diseases (the serum creatinine higher than 105 µmol/L and/or blood urea nitrogen higher than 8.5 mmol/L); (IV) patients had any hematologic disorder; (V) patients had use of lipid-lowering drugs within prior three months; (VI) patients had systolic blood pressure (SBP) higher than 160 mmHg and/or diastolic blood pressure (DBP) higher than 95 mmHg, or symptomatic hypertension; (VII) patients had >70% carotid artery stenosis on ultrasonography; (VIII) patients had a history of stroke; (IX) patients had concomitant vision, hearing or cognitive impairments; (X) patients had a body mass index (BMI) lower than 28 kg/m2; (XI) patients received the treatment with cortisol or cortisol analogues within prior 3 months; (XII) patients had a history of familial hyperlipidemia, and (XIII) patients were pregnant or breastfeeding. The clinical and demographic characteristics of included patients at baseline are shown in Table 1. There were no marked differences in these characteristics between two groups.
Full table
Study design
This was an open, controlled, 24-week follow-up trial. One hundred and fifty outpatients who were initially diagnosed with T2DM and mild to moderate carotid atherosclerosis [peak systolic velocity (PSV) less than 230 cm/s or maximum stenosis less than 70% on ultrasonography and duplex ultrasonography (11)] were randomly assigned into the combination treatment group [combined group (CG), n=75], patients were treated with simvastatin (Shujiangzhi, Merck Sharp & Dohme Limited, UK; 40 mg once daily administered at night) plus hirudin (Maixuekang, Chongqing Duoputai Pharmaceutical Co., Ltd, China; 3 g thrice daily 30 min before three meals) or the simvastatin treatment (40 mg once daily) group [monotherapy group (MG) n=75]. All subjects received routine diet control and sulfonylurea therapy for at least two weeks to control the fasting glucose below 7.8 mmol/L and thereafter the treatment was maintained. Those with mild hypertension were treated with amlodipine (Luohuoxi, Pfizer, NY, USA; 2.5–5 mg daily once when luce prima and fasting) to lower the blood pressure less than 140/90 mmHg. Patients received a regular follow up once every two weeks for six months, during which the routine fasting blood glucose and 2 h postprandial blood glucose were measured. The dosage of sulfonylurea was adjusted according to the blood glucose and glycosylated hemoglobin (HbA1c) (upper limit 7.0%), and the drug-related adverse events were also recorded. Blood biochemical, HbA1c, coagulation function detection, electrocardiography and neck vascular ultrasonography were performed independently at three time-points: baseline, 3-month treatment and 6-month treatment. The dose of hirudin decreased to 2 g twice daily as the international normalized ratio increased to >2.5 or at one week after the treatment with hirudin at 2 g twice daily. Vitamin K as an antagonist was used intravenously once daily for three days; thereafter, patients were treated with natural hirudin at moderate dose (1–2 g/d) when serious bleeding complications appeared.
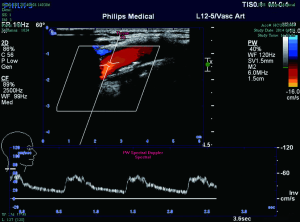
Assessment of carotid atherosclerosis
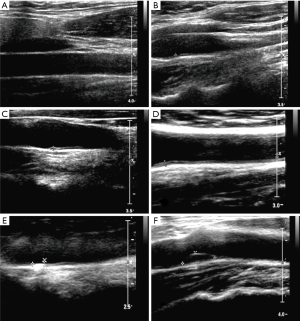
Ultrasonographic examination of the carotid arteries was performed using PHILIPS-IU Elitme color Doppler ultrasound display instrument (S12-5 probe, frequency 512 MHz). All the examinations were done by the same clinician. The carotid intima-media thickness (IMT) was measured at 1 cm below the bilateral carotid arterial bifurcations, common carotid artery, internal carotid artery and external carotid artery. IMT <1 mm means normal, IMT >1.5 mm means plaque formation, IMT 1–1.5 mm means intimal thickening of the carotid artery (12). The diameter and thickness of all the plaques were measured. Color Doppler was used to detect the blood flow spatial distribution and the carotid artery flow velocity. The PSV and end-diastolic velocity (EDV) were determined by Doppler spectrum testing to indirectly reflect the hemodynamics and arterial stenosis. On the basis of vascular intimal thickening and cavity flow distribution on ultrasonography (Figures 1,2), arteriosclerosis was scored as follows: (I) uneven thickening and the focal thickness >1 mm on 2-dimensional ultrasonography and local rough blood flow on color Doppler ultrasonography; (II) significant intimal thickening (>1 mm, but <1.5 mm); (III) focal intimal thickening and solitary plaque; (IV) multiple stable plaques; (V) intimal thickening and unstable plaques.
Statistical analysis
Statistical analysis was performed with SPSS version 19.0 statistical package (SPSS, Chicago, IL, USA). Means were compared using one-way analysis of variance (ANOVA), rates or proportions were compared using Chi-square test or Fisher exact test, and the correlations between carotid atherosclerosis and other variables (such as blood lipids, fasting glucose, etc.) were evaluated with multivariate logistic regression analysis. A value of P<0.05 was considered statistically significant.
Results
Patients’ characteristics
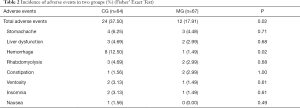
The baseline demographic and clinical characteristics, laboratory findings, and concomitant medications are shown in Table 1. There were no significant differences in the demographics, time interval between T2DM diagnosis and recruitment, and risk factors (age, gender, dyslipidemia, BMI, hypertension, course of T2DM and HbA1c) between two groups. One hundred and fifty patients participated in this trial and 19 (11 in CG and 8 in MG) withdrew from this study due to drug unavailability. No difference (Fisher’ Exact Test) was observed in the drop-out rate between two groups (CG: 14.67%, MG: 10.67%, P=0.62). The reasons for drop-out included adverse events (6/75 vs. 3/75, P=0.49), requests of the patients (3/75 vs. 4/75, P=1.00) and loss to follow-up (2/75 vs. 1/75; P=1.00). Significant difference was indicated in the incidence of adverse events between CG and MG (37.50% vs. 17.91%, P=0.02) due to the marked statistical difference in the higher risk of hemorrhage in CG than in MG (12.50% vs. 1.49%, P=0.02; Table 2).
Full table
Blood glucose controlling
As shown in Figure 3, the fasting glucose and HbA1c decreased progressively to normal upper limit in both groups (fasting glucose <7.8 mmol/L; HbA1c <7%). No significant differences were found in the fasting glucose and HbA1c between two groups at each time point.

Atherosclerosis score
The atherosclerosis score increased since the beginning of treatments in both groups. The change of arterial stiffness score in the CG was significantly lower than in the MG at the 12th week (0.12±0.09 vs. 0.26±0.11, P=0.00, F138=67.71), although the degree of atherosclerosis increased in both groups. A similar result was observed in the arterial stiffness score at the endpoint (0.18±0.13 in the CG vs. 0.24±0.17 in the MG, P=0.03, F129=5.11).
Plaque size
The plaque thickness reduced significantly at week 12 in the CG in comparison to the MG (–0.03±0.09 vs. 0.01±0.12, P=0.03, F138=4.96) and this improvement maintained thereafter to the end of study (0.03±0.11 vs. 0.10±0.13, P=0.03, F129=2.24) but the change of plaque diameter remained unaffected at week 12 (0.11±0.10 vs. 0.14±0.13, P=0.14, F129=2.18) and at the endpoint (0.15±0.12 vs. 0.16±0.12, P=0.63, F129=0.23).
PSV and EDV
As shown in Figure 4, significant differences were found in the changes of PSV and EDV between CG and MG at week 12 (12.64±7.72 vs. 15.35±5.86, P=0.02, F138=5.49 for PSV and 10.22±4.18 vs. 12.26±4.51, P=0.01, F138=7.69 for EDV). Significant differences were also noted at the endpoint (21.20±7.75 vs. 28.35±8.92, P=0.03, F129=4.64 for PSV and 14.60±6.95 vs. 18.28±8.13, P=0.01, F129=7.52 for EDV).

Multivariate regression analysis
Multivariate regression analysis was employed to investigate the relationship of atherosclerosis parameters with treatment and clinical risk factors (age, gender, dyslipidemia, BMI, hypertension, duration of diabetes and HbA1c). As shown in Table 3, hirudin treatment was able to independently predict the carotid artery atherosclerosis scores (β=2.37, P<0.05), the plaque thickening (β=3.51, P<0.01) and the change of PSV (β=1.69, P<0.05) and EDV (β=1.79, P<0.05).
Full table
Discussion
T2DM is a complex disease affecting almost all tissues and organs, with metabolic complications extending far beyond the impaired glucose metabolism. Early diagnosis and interventions are critical to prevent its progression and can delay or even prevent the serious complications of T2DM (13). Oral anti-diabetic drugs (OAD) are the most frequently used drugs in T2DM patients with HbA1c of 8–9% (14). Among these drugs, metformin is the most widely used OAD with high safety and can significantly reduce HbA1c and fasting plasma glucose (15). In this study, sulfonylurea was used to control blood glucose to a normal level. The BMI of patients in our study was lower than that in most clinical studies mainly due to the treatment recommendation in Chinese guidelines that metformin is preferentially given to the patients with high BMI and mild or early diabetes. There were no significant differences in the baseline demographics, clinical manifestations and ultrasound findings between two groups. Although the incidence of adverse reactions in the CG was higher than in the MG due to the increased risk of bleeding, it did not affect the treatment compliance. The drop-out rate was also comparable between two groups suggesting that adjunction hirudin to statin treatment is safe and have tolerable adverse reactions.
Carotid IMT can be used for the early diagnosis of systemic atherosclerosis. The superficial location of carotid artery makes its ultrasonography easy and convenient. Thus, ultrasonography of the carotid artery has been used to evaluate atherosclerosis. Color Doppler ultrasonography is a simple, non-invasive, economical and reproducible tool for the assessment of carotid atherosclerosis (16), and can directly measure the IMT in the absence of changes in hemodynamics an d morphology. Thus, it can predict and detect the early vascular changes in T2DM patients and therefore has been widely used for the assessment of systemic atherosclerosis and cardiovascular risk in adults (17). In this study, on the basis of arteriosclerosis scores, plaque size, PSV and EDV, our results indicated that atherosclerosis is a progressive process in T2DM, even with drug treatment, and treatment is to delay its progression and deterioration. This is consistent with clinical findings. Currently, the accurate mechanism of diabetic atherosclerosis is still poorly understood, and specific treatment has been developed for the atherosclerosis in T2DM patients. A hallmark of atherosclerosis is the uptake of modified forms of LDL via scavenger receptors, leading to the transformation of macrophages and smooth muscle cells into foam cells. LDL particles are modified in the arterial intima and the circulation by several mechanisms, such as glycation, lipolysis, aggregation, oxidation and adaptive immune mechanisms (18). Statins treatment has been recommended in the treatment of T2DM by most clinical guidelines due to their favorable lipid-lowering activity. Reports have highlighted the underutilization of statins in clinical practice and the suboptimal adherence to the guideline recommendations (19). Simvastatin is able to rapidly reduce LDL by 20–48%, which reduces cardiac vascular risks, stabilizes atherosclerotic plaque, and prevents organ damage (cardiac remodeling after ischemic and non-ischemic injury) (3). Considering other reasons, such as reduction of selection bias and local medical insurance restrictions, simvastatin was used as an anti-arteriosclerotic drug, and the efficacy and safety of hirudin plus simvastatin vs. simvastatin alone were investigated in patients initially diagnosed with T2DM. Simvastatin was administered at 40 mg/d because it at this dose is enough to achieve therapeutic effects without increasing the adverse events. Our results showed that, after treatment, simvastatin plus hirudin was better to improve the arteriosclerosis score and plaque thickness than simvastatin alone, which further confirms the role of blood coagulation in the occurrence and development of atherosclerosis. It has been known that the atherosclerotic lesions have cholesterol deposition, infiltration of monocytes, accumulation of extracellular matrix, proliferation and migration of vascular smooth muscle cells as well as increased coagulation factors, anti-fibrinolytic proteins and the fibrin network that is resistant to lysis and readily promotes plaque formation, plaque rupture and atherothrombotic events in DM patients. Anti-coagulation therapy has long proved to be able to prevent thrombus extension or embolization, inhibit new thrombus formation and eventually reduce the risk of long-term complications such as alterations of coagulation, platelet reactivity, and microparticle release. Hirudin, a direct oral anticoagulant, can be given at fixed doses without routine monitoring and has the same efficacy to conventional anti-coagulation treatment (heparin or warfarin). In addition, there is evidence showing that hirudin can inhibit the thrombosis, decrease the platelet aggregation, reduce the serum cholesterol and triglyceride and improve the cerebral microcirculation (20). In this study, results showed combined treatment with hirudin and simvastatin was better to improve the atherosclerosis scores and plaque thickness as compared to simvastatin alone, which means the synergistic anti-atherosclerotic effects by directly acting on the hypercoagulable state (21) or other pathological processes related to atherosclerosis.
PSV and EDV were measured in the present to indirectly evaluate the degree of stenosis. PSV is the peak velocity during systolic period. EDV is the velocity at the end of diastolic period. Both PSV and EDV can be recognized easily on Doppler ultrasonography and measurement of PSV and EDV provides a rapid, reliable and sensitive tool (16) for the detection of the elasticity of local artery and the resistance at the distal circulation. DM often leads to pathological increases in PSV and EDV which may be related to thrombosis (22), poor blood flow (23), increased peripheral resistance (24), and decreased elasticity due to the endothelial dysfunction in T2DM. Our results showed combined treatment could delay the increase in PSV and EDV and had better anti-atherosclerosis effect than simvastatin monotherapy. Thus, hirudin combined with simvastatin is a better choice for the treatment of atherosclerosis induced by T2DM. Our study failed to indicate more potential improvement on the diameter of atherosclerotic plaques in CG than in MG. This may be explained as follows: (I) there are some confounding factors including the traditional risk factors (such as age and history of DM, coronary artery disease, hypertension, stable angina pectoris, and chronic kidney disease), novel risk factors (such as shear stress, nature of atherosclerotic plaque, and biochemical risk factors in the carotid atherosclerotic plaques and blood), and risk factors of infection. These confounding factors have been reported to be associated with human carotid atherosclerosis; (II) there are differences in the sensitivity of ultrasonography and the mechanisms of sclerosis involved in the extension and growth of atherosclerotic plaques in T2DM patients. For example, diabetic retinopathy has a significant positive correlation with the Credit-Control-Answer (CCA) diameter, but not the mean IMT or plaque. Therefore, more studies are needed to elucidate the possible mechanisms underlying the therapeutic effects of hirudin (25); (III) the sample size was small in this study.
Our study has several limitations. First, the follow up period was relatively short because atherosclerosis is a long process, and the sample size was small. Second, our study only partially reflected the real conditions in routine clinical practice because there is still controversy on the criteria for the evaluation of therapeutic efficacy of statins in atherosclerosis patients. More studies with elegant design and large sample size are needed to confirm our findings in the future. Third, the effect of anti-hypertension treatment must be considered because 68.7% of patients had concomitant mild hypertension in our study, and hypertension has long been proposed as a risk factor of atherosclerosis. However, only mild hypertension patients were selected in this study and therefore small vessels are more likely to be affected than the big ones (26). Hypertension may promote the hormone (such as glucagon) secretion via the renin-angiotensin system to increase the blood glucose (27) and indirectly affect the treatment outcomes of diabetes, which may also bias our results. Fortunately, the proportions of patients with hypertension was comparable between groups in this study, and the calcium antagonists were used for the treatment of hypertension in patients except for amlodipine at unfixed doses. Multivariate regression analysis was used to further assess the contribution of hirudin therapy to the protective effects on atherosclerosis. However, the impact of hypertension on the arteriosclerosis was not excluded, and thus the explanation of our conclusions should be cautious.
Conclusions
Taken together, this study indicates that simvastatin plus hirudin has more advantages than simvastatin alone in inhibiting the intimal thickening and plaques growth in patients with early T2DM, especially those with concomitant mild hypertension. This combined therapy is safe, tolerable and better to delay the deterioration of atherosclerosis, offering a promising strategy for the clinical therapy of early T2DM.
Acknowledgments
None.
Footnote
Conflict of Interests: The authors have no conflicts of interest to declare.
Ethical Statement: This study was carried out in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang University (ID: KYKS130).
References
- Eilenberg W, Stojkovic S, Piechota-Polanczyk A, et al. Neutrophil gelatinase associated lipocalin (NGAL) is elevated in type 2 diabetics with carotid artery stenosis and reduced under metformin treatment. Cardiovasc Diabetol 2017;16:98. [Crossref] [PubMed]
- Marín-Peñalver JJ, Martín-Timón I, Sevillano-Collantes C, et al. Update on the treatment of type 2 diabetes mellitus. World J Diabetes 2016;7:354-95. [Crossref] [PubMed]
- Tarantino N, Santoro F, De Gennaro L, et al. Fenofibrate/simvastatin fixed-dose combination in the treatment of mixed dyslipidemia: safety, efficacy, and place in therapy. Vasc Health Risk Manag 2017;13:29-41. [Crossref] [PubMed]
- King RJ, Grant PJ. Diabetes and cardiovascular disease: pathophysiology of a life-threatening epidemic. Herz 2016;41:184-92. [Crossref] [PubMed]
- Soma P, Pretorius E. Interplay between ultrastructural findings and atherothrombotic complications in type 2 diabetes mellitus. Cardiovasc Diabetol 2015;14:96. [Crossref] [PubMed]
- Whitaker EJ, Alshammari A. Bacteriostatic Effect of Simvastatin on Selected Oral Streptococci in Vitro. Contemp Clin Dent 2017;8:59-63. [Crossref] [PubMed]
- Alaarg A, Senders ML, Varela-Moreira A, et al. A systematic comparison of clinically viable nanomedicines targeting HMG-CoA reductase in inflammatory atherosclerosis. J Control Release 2017;262:47-57. [Crossref] [PubMed]
- Ooba N, Setoguchi S, Sato T, et al. Lipid-lowering drugs and risk of new-onset diabetes: a cohort study using Japanese healthcare data linked to clinical data for health screening. BMJ Open 2017;7:e015935. [Crossref] [PubMed]
- Luo P, Wang L, Zhu H, et al. Impact of Atorvastatin Combined with Ezetimibe for the Treatment of Carotid Atherosclerosis in Patients with Coronary Heart Disease. Acta Cardiol Sin 2016;32:578-85. [PubMed]
- Fichter AM, Ritschl LM, Robitzky LK, et al. Impact of different antithrombotics on the microcirculation and viability of perforator-based ischaemic skin flaps in a small animal model. Sci Rep 2016;6:35833. [Crossref] [PubMed]
- Avci A, Fidan S, Tabakci MM, et al. Association between the Gensini Score and Carotid Artery Stenosis. Korean Circ J 2016;46:639-45. [Crossref] [PubMed]
- Steinbuch J, van Dijk AC, Schreuder F, et al. Definition of common carotid wall thickness affects risk classification in relation to degree of internal carotid artery stenosis: the Plaque At RISK (PARISK) study. Cardiovasc Ultrasound 2017;15:9. [Crossref] [PubMed]
- Salek-Maghsoudi A, Vakhshiteh F, Torabi R, et al. Recent advances in biosensor technology in assessment of early diabetes biomarkers. Biosens Bioelectron 2018;99:122-35. [Crossref] [PubMed]
- Weng W, Tian Y, Kimball ES, et al. Treatment patterns and clinical characteristics of patients with type 2 diabetes mellitus according to body mass index: findings from an electronic medical records database. BMJ Open Diabetes Res Care 2017;5:e000382. [Crossref] [PubMed]
- Vijayakumar TM, Jayram J, Meghana Cheekireddy V, et al. Safety, Efficacy, and Bioavailability of Fixed-Dose Combinations in Type 2 Diabetes Mellitus: A Systematic Updated Review. Curr Ther Res Clin Exp 2017;84:4-9. [Crossref] [PubMed]
- Zou C, Jiao Y, Li X, et al. Differences between healthy adults and patients with type 2 diabetes mellitus in reactivity of toe microcirculation by ultrasound combined with a warm bath test. Medicine (Baltimore) 2017;96:e7035. [Crossref] [PubMed]
- Liu DS, Wang SL, Li JM, et al. Allicin improves carotid artery intima-media thickness in coronary artery disease patients with hyperhomocysteinemia. Exp Ther Med 2017;14:1722-6. [Crossref] [PubMed]
- Hörl G, Froehlich H, Ferstl U, et al. Simvastatin Efficiently Lowers Small LDL-IgG Immune Complex Levels: A Therapeutic Quality beyond the Lipid-Lowering Effect. PLoS One 2016;11:e0148210. [Crossref] [PubMed]
- Elnaem MH, Mohamed MHN, Huri HZ, et al. Statin Therapy Prescribing for Patients with Type 2 Diabetes Mellitus: A Review of Current Evidence and Challenges. J Pharm Bioallied Sci 2017;9:80-7. [PubMed]
- Li DQ, Zhou YP, Yang H. Donepezil combined with natural hirudin improves the clinical symptoms of patients with mild-to-moderate Alzheimer's disease: a 20-week open-label pilot study. Int J Med Sci 2012;9:248-55. [Crossref] [PubMed]
- Ferroni P, Della-Morte D, Pileggi A, et al. Impact of statins on the coagulation status of type 2 diabetes patients evaluated by a novel thrombin-generation assay. Cardiovasc Drugs Ther 2012;26:301-9. [Crossref] [PubMed]
- Eibenberger K, Schmetterer L, Rezar-Dreindl S, et al. Effects of Intravitreal Dexamethasone Implants on Retinal Oxygen Saturation, Vessel Diameter, and Retrobulbar Blood Flow Velocity in ME Secondary to RVO. Invest Ophthalmol Vis Sci 2017;58:5022-9. [Crossref] [PubMed]
- Vercellin Alice C V, Cutolo CA, Dellafiore C, et al. Inter-device reproducibility of retrobulbar blood flow velocity measurements in healthy subjects using color Doppler imaging. J Ultrasound 2016;19:125-30. [Crossref] [PubMed]
- Batista PR, Gobello C, Rube A, et al. Reference range of gestational uterine artery resistance index in small canine breeds. Theriogenology 2018;114:81-4. [Crossref] [PubMed]
- Miyamoto M, Kotani K, Okada K, et al. The correlation of common carotid arterial diameter with atherosclerosis and diabetic retinopathy in patients with type 2 diabetes mellitus. Acta Diabetol 2012;49:63-8. [Crossref] [PubMed]
- Blanco PJ, Muller LO, Spence JD. Blood pressure gradients in cerebral arteries: a clue to pathogenesis of cerebral small vessel disease. Stroke Vasc Neurol 2017;2:108-17. [Crossref] [PubMed]
- Skov J, Persson F, Frøkiær J, et al. Tissue Renin-Angiotensin systems: a unifying hypothesis of metabolic disease. Front Endocrinol (Lausanne) 2014;5:23. [Crossref] [PubMed]