The effect of extension assist orthosis with pneumatic bladders on pain and function for patients with early knee osteoarthritis
Introduction
There are few non-invasive treatment options to slow the progression of knee osteoarthritis (OA) and there is no current treatment to cure or stop the disease (1). The gold standard of treatment continues to be total knee arthroplasty (TKA). Despite the success and benefits of TKA, many patients with knee pain are not candidates for surgery because they do not have end-stage structural changes. For these patients, non-invasive treatments are the standard course of care (2). Joint injections and pharmacological management for joint pain are common, but the effectiveness of these interventions is not clear (3). Although these interventions may reduce pain, they do not alter the loads within the joint, do not address biomechanical alterations associated with knee OA, and may therefore not provide protection against continued structural changes.
Unloader bracing is often used to modify joint loads, reduce joint pain, and potentially attenuate the progressive structural changes associated with knee OA (4,5). Unloader braces have traditionally achieved their effect by providing valgus or varus forces to the femur and tibia to reduce the compressive loads in the affected knee compartment. While changing the loads in the frontal plane may help to reduce frontal plane moments, these braces do not address sagittal plane motion loss during gait. Loss of knee extension is an important factor in patients with knee OA. When walking, patients with knee OA have characteristic “stiff-legged” gait pattern that is typified by reduced knee flexion motion during the loading response of the gait cycle. This stiff-legged gait pattern has been shown to be worse in individuals with more severe knee OA (6) and is a risk factor for future TKA (7,8). Maintaining normal knee range of motion during dynamic activities is a primary goal when managing patients with early or moderate knee OA.
Recently, unloader braces for knee OA have included an extension assist device in order to promote more normal sagittal planes motions (9-11). Use of these braces has been shown to normalize gait mechanics (10), and it is possible that these braces also have a larger effect on pain and function than traditional unloader braces. Recent studies of knee extension assist braces have included a sample of patients later in the course of the disease with a focus on delaying TKA. Extension assist braces may also be exceptionally important to patients earlier in the course of the disease who wish to maintain high levels of activity without pain. Therefore, the purpose of this study was to evaluate the preliminary effectiveness of using a novel unloader brace with knee extension assist to improve pain and functional outcomes for patients with early to moderate symptomatic knee OA. We hypothesized that patients who use a brace for 6 weeks would demonstrate significantly larger improvements in pain and function compared to a control group. We planned to use the magnitude of change and variability measures from our groups to power a larger clinical trial and data from the compliance outcomes to inform the procedures of future studies.
Methods
Participants
Subjects were recruited from the local community through flyers placed in senior centers, public spaces at our University, and in the waiting area of local physical therapy and orthopaedic clinics. Individuals interested in participating were screened by telephone to ensure they met the inclusion and exclusion criteria of the study. To be eligible for participation, subjects had to be between the ages of 40 and 85 and diagnosed with knee OA by a physician. Subjects were excluded from the study if they had high blood pressure that was not controlled by medication, had been diagnosed with neurological disorder that affected daily function, had any condition that reduced sensation in the leg, had a previous knee arthroplasty on either side, or had any arthritic condition other than OA. In order to obtain a sample of patients that was early in the course of OA, we also excluded any individual who was considering TKA or who were offered TKA as a treatment option by their physician. All subjects signed a consent form prior to participating in any aspect of the study. This study was approved by the Human Subjects Review Board at the University of Delaware (Federal Wide Assurance #00004379).
Assessment
Subjects participated in a baseline and follow-up testing functional session. Baseline assessment was completed prior to randomization, and follow-up testing was completed 6 weeks after baseline assessment without wearing the brace. These assessments included a variety of clinical, functional, and questionnaire-based measures. Age, height, weight, and BMI were recorded or calculated at both time points. Subjects completed the Knee Outcome Score—Activities of Daily Living Scale, which is a questionnaire that evaluates a subject’s functional limitations secondary to knee pain and symptoms. Knee pain was assessed using three separate questions. Subjects were asked to rate their knee pain on a 0–10 scale for the following conditions: (I) average pain over the past week; (II) pain at its worst; and (III) pain at its best. The Patient Specific Functional Scale (PSFS) was also administered at both testing timepoints. This test asks subject’s about activities important to them that are affected by their joint pain. This was not used as an outcome assessment, but it was used in a qualitative manner to characterize our subject sample.
Performance-based functional measures included the stair climbing test (SCT) and the six-minute walk (6MW). For the SCT, subjects were instructed to ascend and descend a flight of stairs as quickly as possible, while still being safe. Subjects were allowed to use the handrail for balance only if necessary. For the 6MW, subjects walked on a rectangular loop and were informed of the time remaining at one-minute intervals.
Knee strength and range of motion were also assessed at all testing sessions. Active knee extension range of motion was tested with the subject lying supine on a table with the heels extended on a foam bolster. Subjects were asked to “straighten the knee as much as possible”. For knee flexion, subjects remained in a supine position and were asked to “bend the knee as much as possible” and “bring the heel towards the buttocks”. Maximal range of motion was recorded for two trials using a long-arm goniometer and the average of the two trials was used for the analysis. Isometric quadriceps strength was tested using a dynamometer (Biodex Systems, Shirley, NY, USA). Subjects were seated with their hips flexed approximately 85 degrees and the knee flexed to 75 degrees. After 3 warm-up trials, subjects provided maximal knee extension force against the immobile dynamometer arm. The maximal knee extension force (N) from the three trials was used in the analysis. All strength values were normalized to body weight (N/kg).
Treatment groups
After baseline testing, subjects were randomized into one of two groups: (I) stretching or (II) brace plus Stretching. For the purposes of this paper we will define these groups as either No brace or brace groups because the stretching protocol was identical between groups and the use of the brace was our independent variable of interest. Subjects randomly assigned to the stretching group were asked to perform a stretching program of the legs at least 3 times a week for 6 weeks. Each session was set up to take approximately 20 minutes. This program consisted of stretching the calf muscles, hamstrings, quadriceps and hips. It was reviewed with the subjects after the baseline testing by a licensed physical therapist. Subjects received handouts with written instructions and pictures.
Subjects randomly allocated to the bracing group were instructed to perform the same stretching routine, but also were given a knee brace to wear during the 6-week duration. This brace was fit to the subject at the baseline session and the type of brace was dependent on the individual’s limb alignment. Subjects who had a valgus alignment were given a lateral unloader brace, subjects with varus alignment were given a medial unloader brace, and subjects in neutral alignment were given a neutral brace. Varus and valgus were defined as more than a 3-degree angulation in the frontal plane as measured along the length of the femur and tibia, using the center of the patella as the axis. All braces were from the same company [Ongoing Care Solutions Inc. (OCSI), Pinellas Park, FL, USA]. The unloader braces were OA Rehabilitator™ braces and the neutral braces were the Sport Rehabilitator™ braces. All braces utilized a pneumatic bladder that could be used to adjust the snugness and the unloading capability of the brace (for the unloader braces). All braces also contained elastic bands that encouraged end-range knee extension during gait. Subjects were instructed to wear the brace one hour per day and increase their wear time by one hour per day up to a maximum of 8 hours per day as tolerated. Three weeks after the initial fitting the subjects in the brace group returned to review brace fit and use with a licensed physical therapist.
Compliance
The wear time of the brace may affect outcomes for this type of intervention. For this reason, all subjects wore an activity monitor (FitBit Zip, FitBit Corp. San Francisco, CA, USA) on the brace, which was able to track the number of steps taken while wearing the brace. To validate this placement, we performed a validation analysis prior to enrolling subjects into the clinical trial. Four individuals wore an activity monitor on their hip as well as on different variations of the brace. Each individual wore the activity monitors simultaneously on two or three separate days for 1–2 hours. The root mean square of the percentage difference in number of steps between the hip and brace was evaluated. Eleven separate validation trials were used in the analysis. The root mean square percentage difference was 1.8% (range, 0.0–5.6% difference). Given the low difference between location of the step monitor, we were confident in using the activity monitor on the brace as a measure of compliance.
Adherence to the stretching protocol was also assessed. Each subject received an exercise log and the number of completed exercises was recorded on a daily basis. Subjects were instructed to complete the exercise log honestly, and we reinforced there was no penalty for not completing the exercises. Subjects were instructed to bring the completed exercise log with them to the follow-up testing session.
Analysis
Separate repeated measure ANOVAs were used to identify differences in group and time. In the presence of an interaction effect, follow-up paired t-tests were performed to evaluate for changes over time for each group separately. To evaluate the effect of brace wear time on change in outcomes, Pearson correlation coefficients were calculated for average number of steps in the brace and change in clinical scores. Similarly, Pearson correlation coefficients were calculated for exercise compliance and change in clinical scores for each group separately. P values <0.05 were considered significant for this analysis.
Results
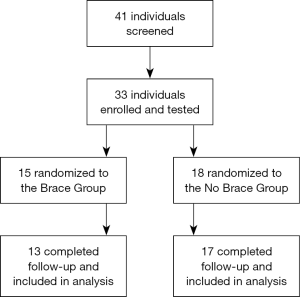
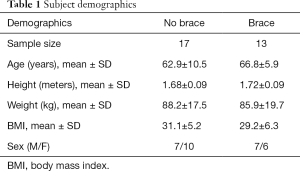
Thirty-three subjects were enrolled and tested at baseline (Figure 1). Three subjects voluntarily withdrew or were unable to be contacted for the follow-up assessment (2 in brace group, 1 in control group). Therefore, 30 subjects were included in this analysis: 17 in the control group and 13 in the brace group. Two subjects in the control group were unable to complete strength testing due to time constraints. Subject demographics for each group are shown in Table 1. Based on the results from the Patient Specific Functional Scale, 63% of subjects reported problems with navigating stairs, 56% reported difficulty walking, 41% had impairments in sport-related activities, and 30% had issues with squatting. Sport activities included a variety of higher-impact activities, including mogul skiing, downhill skiing, basketball, kickboxing, softball and dancing.
Full table
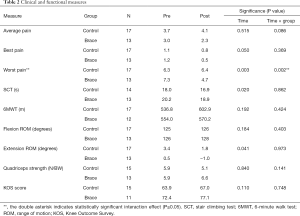
There was a significant interaction effect for knee pain at its worst (P=0.002; Table 2). Post hoc testing revealed the brace group improved from a 7.3/10 at baseline to 4.7/10 at follow-up (P=0.006), while there was no change for the control group (6.3/10 at baseline to 6.4/10 at follow-up, P=0.849). There was an effect of time for the SCT (P=0.02), knee pain at best (P=0.050), and knee extension range of motion (P=0.041). All of these measures demonstrated significant improvement between timepoints, regardless of group assignment.
Full table
In the brace group, average steps per day when using the brace ranged from 587±522 to 9,831±3,098. The average steps per day when using the brace was 3,045±1,796. There were no significant correlations between steps per day in the brace and change in any clinical outcome measure. Exercise compliance ranged from 2% to 100%. The average exercise compliance was 55%±28%. Exercise compliance was 61%±34% in the Brace group and 48%±24% in the no brace group. There were no significant correlations between exercise compliance and change in outcomes when the groups were separated, but when the groups were collapsed there was a significant correlation between compliance and change in knee extension range of motion (r=0.526; P=0.025). There was a greater improvement in knee extension range of motion with higher exercise compliance.
Conclusions
Individuals in the brace group demonstrated a 36% reduction in their worst pain, which is both clinically meaningful and statistically significant. This may indicate that wearing the brace reduced painful flares in the experimental group. As pain is the primary symptom of OA and the number one reason to undergo a replacement (12,13), significantly reducing pain is an important clinical outcome and impactful for patient’s quality of life. This may also be exceptionally important for a group of individuals who remain very active. Forty-one percent of the subjects in our study reported that pain limited their ability to participate in sports-related activities. While the other pain questions we asked, such as best pain and average pain are important, reducing the very symptomatic flares may be best at allowing individuals to continue in higher level recreational activities.
Interestingly, both groups showed improvements in stair climb time, knee pain at best, and knee extension range of motion (ROM). It is important to consider that we did not have a passive control group. Subjects allocated to the control group still participated in an intervention (stretching) that is known to improve knee range of motion. When the groups were collapsed in our statistical analysis, we found that greater compliance with the stretching program was related to greater improvements in knee extension range of motion. This suggests the stretching program is an important and impactful intervention for patients with OA, with or without a brace. Loss of knee extension ROM is highly related to impaired gait (6) and future total knee replacement (8), so maintaining normal motion should be included in any comprehensive intervention. Because the control group used a focused stretching program, it is not possible to ascertain whether using the brace alone would have led to similar improvement in knee extension range. Future work should evaluate the effects of bracing alone on range of motion outcomes.
Interestingly there was no correlation to brace wear time and outcomes. In this study, the average steps per day was approximately 3,000, which is only 30% of the daily recommended 7,000–10,000 steps (14). It is possible that subjects in this study may have been underdosed. This is particularly true for some individuals who walked few than 1,000 steps per day in the brace. There is no current evidence to support an ideal dosage of time for wearing a brace to produce the best outcomes. A recent meta-analysis of brace studies found that dosing was often under-reported and should be included in studies of this nature (15). Future work should assess differing dosing strategies to increase compliance and increase wear time for all participants. It is also possible that we did not see larger treatment effects for functional changes because our intervention was limited to 6 weeks. This is the minimum amount of time needed to see changes in muscle strength and a longer trial period may have produced larger treatment effects.
Although there was not a systematic effect of the brace across all outcome measures, there were several very positive responders in the brace group. Two individuals in the brace group gained 12 degrees of knee extension in 6 weeks. This is an impressive improvement and may be effective at improving long-term outcomes and reducing the need for TKA (8). There may be a need for future responder analyses to identify the characteristics of individuals who have the best response to the brace intervention.
In summary, this unloader brace is a promising non-invasive treatment option for patients with OA who experience high levels of knee pain, but who have no immediate plans to undergo joint replacement. Although bracing and stretching produced improvements in range of motion, the brace had the added benefit of reducing pain at its worst. Clinicians should consider incorporating bracing as a complementary intervention in the physical therapy management of knee OA.
Acknowledgments
This study was made possible by Ongoing Care Solutions, Incorporated who provided funding for subject testing and provided the braces for use in the study. The study sponsors had no influence or input on the research design, analysis, or interpretation of the study results.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Human Subjects Review Board at the University of Delaware (Federal Wide Assurance #00004379). All subjects signed a consent form prior to participating in any aspect of the study.
References
- Hunter DJ, Felson DT. Osteoarthritis. BMJ 2006;332:639-42. [PubMed]
- Taylor N. Nonsurgical Management of Osteoarthritis Knee Pain in the Older Adult: An Update. Rheum Dis Clin North Am 2018;44:513-24. [Crossref] [PubMed]
- Gregori D, Giacovelli G, Minto C, et al. Association of Pharmacological Treatments With Long-term Pain Control in Patients With Knee Osteoarthritis: A Systematic Review and Meta-analysis. JAMA 2018;320:2564-79. [Crossref] [PubMed]
- Petersen W, Ellermann A, Zantop T, et al. Biomechanical effect of unloader braces for medial osteoarthritis of the knee: a systematic review (CRD 42015026136). Arch Orthop Trauma Surg 2016;136:649-56. [Crossref] [PubMed]
- Steadman JR, Briggs KK, Pomeroy SM, et al. Current state of unloading braces for knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2016;24:42-50. [Crossref] [PubMed]
- Zeni JA Jr, Higginson JS. Dynamic knee joint stiffness in subjects with a progressive increase in severity of knee osteoarthritis. Clin Biomech (Bristol, Avon) 2009;24:366-71. [Crossref] [PubMed]
- Zeni JA Jr, Flowers P, Bade M, et al. Stiff knee gait may increase risk of second total knee arthroplasty. J Orthop Res 2019;37:397-402. [Crossref] [PubMed]
- Zeni JA Jr, Axe MJ, Snyder-Mackler L. Clinical predictors of elective total joint replacement in persons with end-stage knee osteoarthritis. BMC Musculoskelet Disord 2010;11:86. [Crossref] [PubMed]
- Cherian JJ, Bhave A, Kapadia BH, et al. Strength and Functional Improvement Using Pneumatic Brace with Extension Assist for End-Stage Knee Osteoarthritis: A Prospective, Randomized trial. J Arthroplasty 2015;30:747-53. [Crossref] [PubMed]
- Kapadia BH, Cherian JJ, Starr R, et al. Gait Using Pneumatic Brace for End-Stage Knee Osteoarthritis. J Knee Surg 2016;29:218-23. [Crossref] [PubMed]
- Chughtai M, Bhave A, Khan SZ, et al. Clinical Outcomes of a Pneumatic Unloader Brace for Kellgren-Lawrence Grades 3 to 4 Osteoarthritis: A Minimum 1-Year Follow-Up Study. J Knee Surg 2016;29:634-8. [Crossref] [PubMed]
- Mannion AF, Kämpfen S, Munzinger U, et al. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther 2009;11:R139. [Crossref] [PubMed]
- Glass NA, Torner JC, Frey Law LA, et al. The relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: a 5-year longitudinal study. Osteoarthritis Cartilage 2013;21:1154-9. [Crossref] [PubMed]
- Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act 2011;8:80. [Crossref] [PubMed]
- Moyer RF, Birmingham TB, Bryant DM, et al. Valgus bracing for knee osteoarthritis: a meta-analysis of randomized trials. Arthritis Care Res (Hoboken) 2015;67:493-501. [Crossref] [PubMed]