
Mitochondrial cytochrome c oxidase is not the primary acceptor for near infrared light—it is mitochondrial bound water: the principles of low-level light therapy
“For an understanding of the phenomena the first condition is the introduction of adequate concepts.” —Werner Heisenberg, 1973
Low level light therapy
Low level light therapy (LLLT) is a growing field in photomedicine: 5,700 citations in PubMed at the date of writing. As a trend, more and more high impact factor journals are publishing papers related to LLLT. The key difference between LLLT (photobiostimulation, photobiomodulation) and other medical laser or light emitting diode (LED) applications is the intensity of the light. Light intensities used in LLLT are moderate and non-destructive (maximum a few kW/m2). For instance, the solar constant (full solar spectrum) above the Earth’s atmosphere corresponds to an intensity of 1.360 kW/m2. Potential clinical applications of LLLT include but are not limited to, wound healing, stroke, traumatic brain injury, neurodegenerative conditions, cancer, in vitro fertilization and pain management. In addition, there are very promising and exciting LLLT applications with enormous potentials in cell-based therapies, for instance, for end-stage liver diseases. Many of these applications exploit the reciprocal interplay between upregulation of mitochondrial adenosine triphosphate (ATP) and downregulation of reactive oxygen species (ROS) in oxidatively stressed cells. According to the mainstream theory the root cause for mitochondrial ATP upregulation in response to irradiation of cells with red-to-near infrared (R-NIR) light is the absorption of R-NIR photons by cytochrome c oxidase (CCO). Here, I show that this theory is inadequate for an explanation of the experimental results obtained in LLLT. Putting a model on a wrong concept will automatically limit its predictive capability, leading to results in disagreement with observation—as it happens today in LLLT. Excellent clinical and experimental results are contrasted by an underlying concept, i.e., the light/cell-interaction mechanism assumed in the majority of reports, which originates from a handful of articles showing incorrect data. Instead, a new theoretical basis for LLLT is presented. The resulting model describes experiments correctly and allows us to predict their outcome, thereby safeguarding future progress in LLLT.
R-NIR light-induced cell metabolism
For instance, Keshri et al. documented the effect of 810 nm laser light (40 mW/cm2, 22.6 J/cm2) applied at frequencies of 10 and 100 Hz as well as in the continuous wave (CW) mode on the healing of dermal wounds in animals. As in other studies, it was found that the therapeutic effect of the pulsed mode was significantly superior to that of the CW mode (1). Importantly, wound contraction was clearly more pronounced at 10 Hz than at 100 Hz. This result correlates well with the biochemical picture, reflected in a significant increase in the ATP levels at 10 Hz, when compared to 100 Hz or CW. The authors of the study interpret the maximum in ATP production at 10 Hz by assuming a greater absorption of 810 nm photons by mitochondrial complex-IV at this frequency. This hypothesis overlooks that the absorption of photons is an extremely fast process when compared to a pulse frequency of 10 Hz. In other words, it is not plausible that a frequency as low as 10 Hz could have an influence on the process of absorption.
In two studies exploring the effect of 830 nm laser light applied in the pulsed and CW mode—with everything else being equal—Ueda and Shimizu reported on cell proliferation and bone formation in vitro (2,3). The biological effect of a frequency of 1 Hz was significantly superior to that of CW (2) and that of 1–2 Hz was significantly superior to that of 8 Hz or CW (3). Earlier, Miyamoto et al. used moderate levels of 514.5 nm laser light (100 mW/cm2, 1–10 J/cm2, pulsed at 10 Hz and CW) in combination with a photosensitizer used in photodynamic therapy (PDT) to irradiate HeLa cells (4). Notably, there was a characteristic difference in the modality of cell death: apoptosis in the pulsed mode and necrosis at CW. This finding indicated that in comparison with CW, a greater amount of photosensitizer entered the cells during pulsed irradiation. While the authors justified their conclusion on the basis of the differences in DNA damage, a reason for the differences in the uptake of the PDT chemical was not provided.
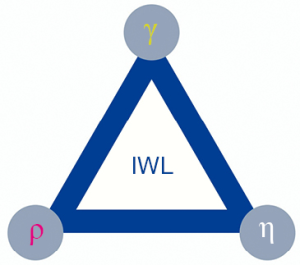
With focus on the effects: accelerated proliferation, ATP upregulation and uptake of photosensitizer in the pulsed mode, the results of recent model experiments recommend themselves for a coherent interpretation of the data reported by both the aforementioned authors and other groups. There is observational evidence that R-NIR photons and presumably other wavelengths (in model experiments we worked with 670 nm—a wavelength for which bulk water is practically transparent) interact with the bound water, i.e., nanoscopic interfacial water layers (IWL) attached to surfaces, especially to hydrophilic ones. IWL consist of 2–3 monolayers of water molecules. The interaction has at least two biologically important impacts: change in IWL density (volume expansion) (5) and reduction in IWL viscosity (6). Figure 1 is a visual synopsis of physical parameters related to IWL. When we use R-NIR lasers in LLLT to irradiate cells or tissues, the photons interact with both biomolecules and the intracellular and intramitochondrial IWL masking surfaces. This insight is of paramount importance if we want to advance with our understanding in LLLT (and PDT). Accounting to the limitations in space I report here only the results of the cited papers, results which are relevant for an understanding of the data reported in refs. (1-3).
Previously, we used biostimulatory levels of 670 nm laser light, applied in a pulsed mode to irradiate HeLa cells supplemented with anticancer agents (8). The main result of the in vitro study was that a pulse frequency of 1 Hz is instrumental in forcing the cells to uptake the drugs dissolved in the culture medium. We have identified the physical mechanism of the uptake as transmembrane convection (light-cell-pump), explained a posteriori on the basis of the expansion in IWL volume in response to laser irradiation, measured in ref. (5): drug molecules adjacent to the plasma membrane are literally sucked into the cells during the dark phase (laser off) (8). Obviously, R-NIR laser irradiation, applied at such low frequencies is capable to maintain a metabolic effect comprising the uptake of molecules, including nutrients, adjacent to the plasma membrane, thus providing an explanation to proliferative effects reported in refs. (1,2). The same mechanism applies to the PDT experiment (4). The findings that with increasing laser pulse frequencies the biological effects are less pronounced (3) could be understood on the basis of the inertia of the aqueous fraction of the cytosol: While it instantly responds to low laser pulse frequencies via expansion of its volume (5), the inertia of the aqueous ensemble in the densely crowded intracellular space opposes a similar effect when the cell is irradiated with higher laser pulse frequencies, where other modalities of interaction come into play.
R-NIR light-induced viscosity modulation
Let us turn our attention to the second key parameter which is induced by biostimulatory intensities of R-NIR laser light, the reduction in IWL viscosity. In contrast to the cytosol volume expansion which is a cumulative effect induced by variations in the volumes of individual IWLs masking the biomolecules and organelles suspended within the cytosol, a global effect which was found to operate at relatively low laser intensities, a change in viscosity is a local effect which demands for higher light intensities. In accord with the model derived from previous experimental results (6), a substantial reduction in IWL viscosity requires the prevalence of a surface covering bombardment of proximal molecules forming the IWL with R-NIR photons. This picture corresponds to higher laser intensities (number of photos per surface area). Clearly, light-induced transmembrane convection (metabolic effect) works exclusively in the pulsed mode, but pulsing is not a precondition for the reduction in IWL viscosity.
Biological effect of the viscosity modulation
What are the biological implications of local variation in IWL viscosity? In order to see the big picture, it is vital to understand the principal factor influencing IWL viscosity in a cell: ROS. ROS are the response of mitochondria to external stress. Thus, mitochondria are both source of ATP and ROS. Due to their negative polarity, ROS tend to increase the hydrophilicity of hydrophilic surfaces known to be masked with viscous, glue-like IWL (6,9). By accentuating hydrophilicity, extended ROS bombardments tend to increase IWL viscosity. A similar situation is encountered in the polystyrene Petri dish (10,11).
In a series of model experiments performed on various materials (both hydrophobic and hydrophilic) we showed that 670 nm laser light applied at biostimulatory levels was instrumental in reducing the viscosity of IWLs on hydrophilic surfaces (6). It is now simple to establish contact to the previous effect, i.e., increase in ATP synthesis upon irradiation of oxidatively stressed cells with biostimulatory levels of R-NIR light. Whenever cells are void of their native environment (in vitro) or in the vicinity of injured tissues (in vivo), they experience stress, manifesting itself in the form of extended bursts of mitochondrial ROS. An inescapable physical consequence of the associated increase in IWL viscosity in the predominantly hydrophilic intramitochondrial space is the decrease in the speed of rotation of the mitochondrial rotary motor (ATP synthase) (12), which must react sensitively to changes in viscosity because of its small inertia and very high speed of rotation (under normal conditions the nanomotor operates at ca. 9,000 rpm). The decline in the operational function of the ATP synthase is necessarily an instant drop in ATP production. This picture is derived from physical measurements and explains why biostimulatory levels of R-NIR laser light are instrumental in restoring ATP levels, both in vitro and in vivo. Moreover, it also explains why biostimulatory levels of pulsed R-NIR laser light show more effect on oxidatively stressed cells than CW: it is simply the synergistic effect of enhanced metabolism (light-cell-pump) and reduction in IWL viscosity. The instant increase in cellular ATP levels upon irradiation with R-NIR LED light reported by Quirk et al. (13)—an effect comparable to the behavior of a race engine upon fuel supplementation—supports the idea that its cause is a physical effect (instant decrease in IWL viscosity) rather than a slow chemical process.
R-NIR light absorption by CCO: a misconception
While the aforementioned drop in IWL viscosity upon irradiation with R-NIR laser light provides a simple and satisfactory explanation to the ATP upregulation in oxidatively stressed cells, current theory assumes that the intrinsic cause for the increase in ATP synthesis is the absorption of the R-NIR photons by CCO (14-16). This concept is rather ill-defined and unsatisfactory for the following reason. A closer inspection of the measurement which serves today as claim to the concept that CCO is the primary absorber for R-NIR photons shows that it consists of a number of statistically distributed points with strongly exaggerated absorbance values in the R-NIR part of the spectrum [by a factor ≥10, c.f. ref. (17)] (14). It is not possible to interpret the data in terms of an absorption spectrum. The second work which apparently provides a consistent absorption spectrum for CCO in the R-NIR range (15) refers as source to a paper (18) in which, unfortunately, the spectrum cannot be found. These papers [refs. (14,15)] form the foundation of the widely accepted concept that CCO is the primary absorber for R-NIR photons. It is perhaps a coincidence that the same group which claimed to provide an absorption spectrum for CCO in ref. (18), reported strong absorbance of CCO in the R-NIR spectral range presenting the same absorption spectrum which appears in ref. (15) in another paper (19). Here too, an absorption spectrum cannot be found in the source reference provided [ref. (20)]. The same pattern repeats itself in ref. (21) where the authors provide as source reference for the absorption of R-NIR photons by CCO ref. (15) in which the reader is guided to the aforementioned ref. (18) where an absorption spectrum cannot be found. This means, the currently accepted theory used to explain ATP upregulation by R-NIR light is based on data which cannot be considered as ascertained. If indeed, CCO is the principal absorber for the photons which eventually drive the ATP synthase, ATP upregulation must depend on the absorbance profile of CCO. Thus, irradiation with 415 nm light [maximum absorbance of both reduced CCO (17) and reduced cytochrome c (22) at 415 nm] is expected to result in an ATP output which is superior to that induced by R-NIR light. This expectation receives justification from the currently accepted mechanism of LLLT, in which the absorption of photons by CCO is the precondition for an upregulation in ATP levels (14-16). However, contrary to expectation, irradiation of human adipose stem cells with blue LED light (415 nm, 16 mW/cm2) resulted in a significant drop in intracellular ATP levels concomitant with an increase in intracellular ROS. Furthermore, ATP levels decreased with increasing light exposure time (23). The authors noted “the effects of blue light on various cellular processes are highly confusing.” This is true because the absorbance for photons is 10 times smaller for R-NIR light than that for 415 nm light—but surprisingly ATP generation is still large for the R-NIR part of the spectrum. High levels of intracellular ROS by blue laser irradiation (405 nm) but not by red (664 nm) or NIR (808 nm), all delivering an intensity of 100 mW/cm2, has been reported by Kushibiki et al. (24). So long as we do not give room to the insight that light which is strongly absorbed by CCO and has a deleterious effect on cells, and therefore, cannot be the intrinsic cause of the ATP upregulation, the confusion will continue.
Recently, the Cooper laboratory presented the absorption spectra for CCO covering the complete range 400–950 nm (17). Using the spectra for interpretation of the data presented in ref. (23)—in vitro study exploring the effect of 415, 540, 660 and 810 nm light on human adipose derived stem cells and the relationship that the absorbance is equal to the negative logarithm of the transmittance, a quick calculation shows that the transmittance of oxidized CCO for 660 and 810 nm photons is 91.7% (8.7% absorbed) and 83.8% (16.2% absorbed), respectively, but for 415 and 540 nm it is 18.0% (82.0% absorbed) and 73.3% (26.7% absorbed), respectively. The wavelengths 415 and 540 nm correlate positively with the absorption spectrum of oxidized CCO shown in ref. (17) and were found to suppress ATP synthesis and produce a strong ROS signal (23). To put it in another way, the absorbance of CCO for blue 415 nm (0.744) and green 540 nm (0.106) is around 20 and 3 times higher than that for 670 nm (0.032) respectively, where the values were extracted from ref. (17). Another CCO absorption spectrum with peaks centered at 418–420 and 598–600 nm and minimal absorption for R-NIR is presented by Malatesta et al. (25). As I recently pointed out (26) the probability that the interaction of R-NIR photons with oxidatively stressed cells occurs via the CCO route is not realistic: the absorption in the R-NIR region of the CCO spectrum is too small for being the root cause for the ATP upregulation. Previously, Quirk and Whelan presented experimental evidence that calls into question the CCO activity model for R-NIR light (27), thus confirming our earlier work that challenged the CCO dogma (28,29). By assuming that the root cause for light-induced upregulation of mitochondrial ATP is not absorption by CCO but simply a physical process involving the reduction in IWL viscosity in the irradiated mitochondria we are led to a paradigm shift in LLLT. This picture is in harmony with the fact that mitochondrial ATP synthesis can be triggered by various wavelengths of light. We only have to omit those which are strongly absorbed by CCO.
Limitations of the new model
Within the model proposed here it was possible to explain both accelerated cell proliferation by R-NIR light in the pulsed mode (enhanced metabolism) as well as mitochondrial ATP upregulation in response to continuous or pulsed irradiation. In the first case, the root cause of the effect is a cytosol volume modulation, in the second, a reduction in IWL viscosity. In emergency situations defined by a high demand of mitochondrial ATP such as stroke or myocardial infarction, a synergistic interplay between enhanced cell metabolism and mitochondrial ATP upregulation by sufficiently intense R-NIR laser light (best case scenario) could help to save lives. However, there are exceptions where intermittent irradiation of cells with R-NIR light seems to have no advantage when compared with continuous exposure (30) as well as examples where the effect of high pulse frequencies is superior to that realized in the CW mode (31). The literature on the subject is meagre, specifically concerning a systematic scan of cell responses to one solitary wavelength over a wider range of pulse frequency starting at 1 Hz and ending at several kHz (32,33). Likewise, there are no reports on monitoring cell responses to biostimulatory light intensities covering a wider spectral range (blue to NIR in small steps) at different pulse frequencies (1 Hz to 10 kHz). Such data could help to verify the predictive capability of the new model.
Considering that the largest part of the cytosol is water, of which a substantial fraction persists as IWL, in particular in mitochondria (34), it is realistic to assume that a major target for photons absorbed by cells will be the water molecules constituting the IWLs on intracellular surfaces (whose physical properties can be modulated by light). The simplest physical pictures suggesting itself on the basis of the experimental results ascertained so far is this: precondition for the activation of the cellular metabolism with pulsed light is the permeability of the plasma membrane for both water and nutrient molecules. When the permeability is too low, a pulse effect related to the modulation of intracellular IWL fraction by light is absent. Cancer cells with low plasma membrane permeability for a certain drug cannot be forced in this way to take it up. Likewise, when the pulse frequency exceeds a certain value at which the intracellular IWLs expand in synchrony with the pulsation, inertia is preventing the water molecules from driving the light-cell-pump—precondition for cellular drug uptake via the convective route. Presumably, higher light pulse frequencies are capable to induce resonant processes in cells and tissues (35). External pulsing can delay, perturb or entrain oscillations, and synchronize oscillations in biological systems (36), influence neuronal activity (37) and induce morphological changes in cells and mitochondria, including changes in mitochondrial volume density per cell (observed 3 days post irradiation) (38). Representative overviews for different pulse frequencies in laboratory and clinical applications are given in refs. (32,33). Taken together, there are unsolved difficulties regarding the explanation of biological effects such as ATP generation, cell proliferation or manifestation of therapeutic effects observed at higher light pulse frequencies (31,39). The effects can have a variety of causes, which, because of the complexity of the interaction modalities between photons and cell, cannot be addressed in this model.
Need for a new model in LLLT
That the light-cell-pump will also be operational in mitochondria can be expected from the early observations of Parsons et al.: “The outer membrane appears to be permeable to both water and sucrose. Water but not sucrose penetrates the inner membrane.” (40). The envisaged permeability was confirmed by many groups, with one of the channels being identified as aquaporin. In 1961, Mitchell made an interesting prediction: “According to the chemi-osmotic type of hypothesis, the coupling of phosphorylation to electron and hydrogen translocation would cause considerable stress in the membrane across which coupling was effected. Complex swelling and shrinkage effects would therefore be expected to accompany the activity of the system.” (41). The question arises: will mitochondria respond to pulses of R-NIR light by swelling during the “light on” phase, or will the fraction of the water which experienced a volume expansion escape through the pores before it comes to an observable swelling? Presumably both processes will take place in parallel with the result depending on the light intensity and pulse frequency. Provided that changes in mitochondrial volume can be monitored, the portrayed experiment would be an elegant test for the validity of the light-cell-pump in mitochondria. It is worth noting that the models which are currently in use to interpret the effect of pulsed light in LLLT and PDT, are inadequate to address this question.
The mitochondrial inner membrane harbors the respiratory complexes involved in ATP production, including CCO. CCO, as the terminal oxidase of cellular respiration, coupled with a proton-pumping process, reduces molecular oxygen to water (42). As noted by Yoshikawa et al.: “This … highly organized chemical process represents one of the most critical aspects of cellular respiration” (43). Because of the complexity of the proton pump it seems reasonable to assume that even minimal perturbation can become critical for its proper functioning, and that light which is absorbed by CCO represent exactly such a perturbation of the enzyme, e.g., intense R-NIR or blue light, which strongly interacts with CCO. According to the small absorbance the perturbation of the enzyme caused by low intensity R-NIR light is small and deleterious effects are minimal. Within the framework of the new model a prerequisite for ATP upregulation is that R-NIR photons reduce the viscosity of the IWL envelope inhibiting the normal rotation of the mitochondrial nanomotor in oxidatively stressed cells (6). The orthodox model which assumes upregulation of mitochondrial ATP via absorption of R-NIR light by CCO fails to correctly describe the experiment. So, the necessity for a departure from the orthodox model is driven by conflicting experimental results.
The purpose of this editorial is to suggest, that in view of the limitations of the orthodox idea, i.e., that the absorption of R-NIR light by CCO is necessary for upregulation of mitochondrial ATP, those working in the field of LLLT and PDT might profitably consider the model resulting from the measurement of light-induced variations in IWL volume and viscosity. It has the merit that it accurately describes a larger number of observables than the orthodox model allowing us to correctly explain experimental results and thereby to optimize treatment protocols using lasers or LEDs in clinical practice. Since the target of the photons are mitochondria—and mitochondria are basically the same in all mammalian cells—the wavelength with the best ATP output can be easily evaluated: it is the wavelength which causes the largest drop in IWL viscosity and is minimally absorbed by CCO. We have here a simple and beautiful road map allowing us to improve the clinical outcome of LLLT. On the basis of the CCO hypothesis, and using the CCO absorption spectra shown, or not shown in the LLLT literature, a similar prediction is not possible. A closer look at the trial and error data published in a recent paper on LLLT shows the need for a systematic optimization of R-NIR irradiation parameters (44). En route to an optimal treatment protocol in LLLT there is a further step which needs our attention. In a short paper dedicated to the question of pulsing in view of the antagonistic light effects in mitochondria—ATP synthesis (via IWL reduction) and ROS generation—we showed that the proper pulse sequence will have to take into consideration the interplay between the time the cell needs to consume its ATP reservoirs and the irradiation time for buildup of a destructive level of ROS. In simple words, once the ATP reservoir is full, we have to discontinue the irradiation because in this way we minimize deleterious effects of ROS (9). Here too we found evidence for the limitations of the model claiming that CCO acts as an absorber of R-NIR light.
Predictive capability of the new model
For a longer period, the irradiation protocols used in laser medicine were restricted besides wavelength to two key-parameters: energy density or dose (E) and time of irradiation (t), interconnected by the equation E = I × t, where I is the intensity of the light. According to the Mester group reproducible photobiological effects required a dose in the 1–4 J/cm2 range. However, their experimental and clinical success involved the use of powerful lasers (45). Ignoring the intensity of the laser beam (power divided by beam cross section) used by the LLLT pioneers, people were unable to reproduce their results. Many groups reached the 1–4 J/cm2 range by the use of weak lasers and extension of the irradiation time. The results were often negative or artefacts. The importance of the laser intensity and the concept of an intensity threshold which has to be surpassed to achieve reproducible biostimulatory effects, first mentioned in a patent (46), was comprehensively described in a cornerstone paper addressing the importance of the light intensity in LLLT. The relationship between the irradiation parameters were described by the LILAB-equation (47). Before its consideration, positive results in LLLT were often realized by trial and error. A very similar situation prevails today when it comes to the photon/cell-interaction mechanism. The new model presented by the author is designed to be used as a road map in LLLT. For this we will need support from the nanotechnology side, i.e., systematic experimental determination of wavelength at which the drop in IWL viscosity is greatest. The experiments would involve the use of a nanoindenter or atomic force microscope (AFM) following the protocol published for the wavelength 670 nm (6). The experiment is simple because only those wavelengths are to be considered which (a) are not absorbed by CCO and (b) for which the absorption of bulk water is small. Once these data are clear, we can leave the present path of trial and error and proceed with a generalized scheme offering us the following benefits: (I) assessment of the optimal light wavelength for biostimulation, (II) the minimum threshold intensities required for reproducible results in LLLT, (III) physical explanation for the complete bell-shaped dose dependency of the cellular response to light (the empirical Arndt-Schultz rule), which is perhaps the most fundamental element in LLLT, where the minimum dose is related to the minimum light intensity necessary to reduce IWL viscosity and the maximum dose is related to interference of the photons with CCO, either directly or via ROS generation. These results pave the way for progress in both experimental and clinical work.
Conclusions
There is substantial evidence that various wavelength of light, including R-NIR delivered by lasers or LEDs are instrumental in upregulating mitochondrial ATP levels. Conflicting data cast serious doubt on the validity of the concept that CCO is the primary photoacceptor for R-NIR light being causal for the ATP upregulation. At the same time there is conclusive evidence that both ATP upregulation and cell proliferation by R-NIR light occurs via the interaction of photons with intracellular IWL. We have here a reason for taking the conflicts between theory and experimental evidence seriously, allowing us to design better therapies, including cell-based therapies where rapid cell proliferation and high demand of mitochondrial ATP concomitant with suppression of ROS release are critical. By exploiting the described synergistic interplay between enhanced metabolism and mitochondrial ATP upregulation by R-NIR light, LLLT shows an enormous potential for the success of cell-based therapies, for instance, for end-stage liver diseases (48), in particular in view of the good water permeability of liver mitochondria, demonstrated in animal models (49).
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Keshri GK, Gupta A, Yadav A, et al. Photobiomodulation with pulsed and continuous wave near-infrared laser (810 nm, Al-Ga-As) augments dermal wound healing in immunosuppressed rats. PLoS One 2016;11:e0166705. [Crossref] [PubMed]
- Ueda Y, Shimizu N. Pulse irradiation of low-power laser stimulates bone nodule formation. J Oral Sci 2001;43:55-60. [Crossref] [PubMed]
- Ueda Y, Shimizu N. Effects of pulse frequency of low-level laser therapy (LLLT) on bone nodule formation in rat calvarial cells. J Clin Laser Med Surg 2003;21:271-7. [Crossref] [PubMed]
- Miyamoto Y, Umebayashi Y, Nishisaka T. Comparison of phototoxicity mechanism between pulsed and continuous wave irradiation in photodynamic therapy. J Photochem Photobiol B 1999;53:53-9. [Crossref] [PubMed]
- Sommer AP, Hodeck KF, Zhu D, et al. Breathing volume into interfacial water with laser light. J Phys Chem Lett 2011;2:562-5. [Crossref]
- Sommer AP, Haddad MKh, Fecht HJ. Light effect on water viscosity: Implication for ATP biosynthesis. Sci Rep 2015;5:12029. [Crossref] [PubMed]
- Koos E, Dittmann J, Willenbacher N. Capillary Forces in Suspensions: Rheological Features und Potential Applications. Chem Ing Tech 2011;83:1305-9. [Crossref]
- Sommer AP, Zhu D, Scharnweber T. Laser modulated transmembrane convection: Implementation in cancer chemotherapy. J Control Release 2010;148:131-4. [Crossref] [PubMed]
- Sommer AP, Mester AR, Trelles MA. Tuning the mitochondrial rotary motor with light. Ann Transl Med 2015;3:346. [PubMed]
- Sommer AP, Jaganathan S, Maduro MR, et al. Genesis on diamonds II: contact with diamond enhances human sperm performance by 300%. Ann Transl Med 2016;4:407. [Crossref] [PubMed]
- Diamond dishes could boost IVF success rates. Available online: https://www.sciencemag.org/news/2017/04/diamond-dishes-could-boost-ivf-success-rates
- Sommer AP. Aging is a sticky business. Photomed Laser Surg 2018;36:284-6. [Crossref] [PubMed]
- Quirk BJ, Sannagowdara K, Buchmann EV, et al. Effect of near-infrared light on in vitro cellular ATP production of osteoblasts and fibroblasts and on fracture healing with intramedullary fixation. J Clin Orthop Trauma 2016;7:234-41. [Crossref] [PubMed]
- Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B 1999;49:1-17. [Crossref] [PubMed]
- Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem 2005;280:4761-71. [Crossref] [PubMed]
- Passarella S, Karu T. Absorption of monochromatic and narrow band radiation in the visible and near IR by both mitochondrial and non-mitochondrial photoacceptors results in photobiomodulation. J Photochem Photobiol B 2014;140:344-58. [Crossref] [PubMed]
- Mason MG, Nicholls P, Cooper CE. Re-evaluation of the near infrared spectra of mitochondrial cytochrome c oxidase: Implications for non invasive in vivo monitoring of tissues. Biochim Biophys Acta 2014;1837:1882-91. [Crossref] [PubMed]
- Cooper CE, Springett R. Measurement of cytochrome oxidase and mitochondrial energetics by near-infrared spectroscopy. Philos Trans R Soc Lond B Biol Sci 1997;352:669-76. [Crossref] [PubMed]
- Whelan H, Desmet K, Buchmann E, et al. Harnessing the cell's own ability to repair and prevent neurodegenerative disease. SPIE Newsroom 2008;2008:1-3. [PubMed]
- Beauvoit B, Evans SM, Jenkins TW, et al. Correlation between the light scattering and the mitochondrial content of normal tissues and transplantable rodent tumors. Anal Biochem 1995;226:167-74. [Crossref] [PubMed]
- Desmet KD, Paz DA, Corry JJ, et al. Clinical and experimental applications of NIR-LED photobiomodulation. Photomed Laser Surg 2006;24:121-8. [Crossref] [PubMed]
- Koch HG, Schneider D. Folding, assembly, and stability of transmembrane cytochromes. Current Chem Biol 2007;1:59-74.
- Wang Y, Huang YY, Wang Y, et al. Red (660nm) or near-infrared (810nm) photobiomodulation stimulates, while blue (415nm), green (540nm) light inhibits proliferation in human adipose-derived stem cells. Sci Rep 2017;7:7781. [Crossref] [PubMed]
- Kushibiki T, Hirasawa T, Okawa S, et al. Blue laser irradiation generates intracellular reactive oxygen species in various types of cells. Photomed Laser Surg 2013;31:95-104. [Crossref] [PubMed]
- Malatesta F, Antonini G, Sarti P, et al. Structure and function of a molecular machine: cytochrome c oxidase. Biophys Chem 1995;54:1-33. [Crossref] [PubMed]
- Sommer AP. Diamonds are for men, too. Ann Transl Med 2017;5:509. [Crossref] [PubMed]
- Quirk BJ, Whelan HT. Effect of red-to-near infrared light on the reaction of isolated cytochrome c oxidase with cytochrome c. Photomed Laser Surg 2016;34:631-7. [Crossref] [PubMed]
- Sommer AP, Haddad MKh, Fecht HJ. Tuning the wheel of life with light. Proceedings of the International Conference on Laser Applications in Life Sciences. Ulm, Germany, 2014:145.
- Sommer AP. A mechanism for ultrasound/light-induced biostimulation. Ann Transl Med 2015;3:291. [PubMed]
- Wu X, Moges H, DeTaboada L, et al. Comparison of the effects of pulsed and continuous wave light on axonal regeneration in a rat model of spinal cord injury. Lasers Med Sci 2012;27:525-8. [Crossref] [PubMed]
- Kim HB, Baik KY, Seonwoo H, et al. Effects of pulsing of light on the dentinogenesis of dental pulp stem cells in vitro. Sci Rep 2018;8:2057. [Crossref] [PubMed]
- Gavish L, Houreld NN. Therapeutic Efficacy of Home-Use Photobiomodulation Devices: A Systematic Literature Review. Photomed Laser Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Hashmi JT, Huang YY, Sharma SK, et al. Effect of pulsing in low-level light therapy. Lasers Surg Med 2010;42:450-66. [Crossref] [PubMed]
- Ford RC, Ruffle SV, Ramirez-Cuesta AJ, et al. Inelastic incoherent neutron scattering measurements of intact cells and tissues and detection of interfacial water. J Am Chem Soc 2004;126:4682-8. [Crossref] [PubMed]
- Ando T, Xuan W, Xu T, et al. Comparison of therapeutic effects between pulsed and continuous wave 810-nm wavelength laser irradiation for traumatic brain injury in mice. PLoS One 2011;6:e26212. [Crossref] [PubMed]
- Pogodaev AA, Wong ASY, Huck WTS. Photochemical control over oscillations in chemical reaction networks. J Am Chem Soc 2017;139:15296-9. [Crossref] [PubMed]
- Herman AM, Huang L, Murphey DK, et al. Cell type-specific and time-dependent light exposure contribute to silencing in neurons expressing Channelrhodopsin-2. eLife 2014;3:e01481. [Crossref] [PubMed]
- Kim HB, Baik KY, Choung PH, et al. Pulse frequency dependency of photobiomodulation on the bioenergetic functions of human dental pulp stem cells. Sci Rep 2017;7:15927. [Crossref] [PubMed]
- Brondon P, Stadler I, Lanzafame RJ. Pulsing influences photoradiation outcomes in cell culture. Lasers Surg Med 2009;41:222-6. [Crossref] [PubMed]
- Parsons DF, Williams GR, Chance B. Characteristics of isolated and purified preparations of the outer and inner membranes of mitochondria. Ann N Y Acad Sci 1966;137:643-66. [Crossref] [PubMed]
- Mitchell P. Coupling of phosphorylation to electron and hydrogen transfer by a chemi-osmotic type of mechanism. Nature 1961;191:144-8. [Crossref] [PubMed]
- Ryan MT, Hoogenraad NJ. Mitochondrial-nuclear communications. Annu Rev Biochem 2007;76:701-22. [Crossref] [PubMed]
- Yoshikawa S, Muramoto K, Shinzawa-Itoh K. Proton-pumping mechanism of cytochrome c oxidase. Annu Rev Biophys 2011;40:205-23. [Crossref] [PubMed]
- Zein R, Selting W, Hamblin MR. Review of light parameters and photobiomodulation efficacy: dive into complexity. J Biomed Opt 2018;23:1-17. [Crossref] [PubMed]
- Mester E, Mester AF, Mester A. The biomedical effects of laser application. Lasers Surg Med 1985;5:31-9. [Crossref] [PubMed]
- Sommer A. Fast Surface Covering Beam Distributor for Lasers. German Patent Office. 1993, Patent number DE4308474A1.
- Sommer AP, Pinheiro AL, Mester AR, et al. Biostimulatory windows in low-intensity laser activation: lasers, scanners, and NASA's light-emitting diode array system. J Clin Laser Med Surg 2001;19:29-33. [Crossref] [PubMed]
- Feng R, Morine Y, Ikemoto T, et al. Photobiomodulation with red light-emitting diodes accelerates hepatocyte proliferation through reactive oxygen species/extracellular signal-regulated kinase pathway. Hepatol Res 2018;48:926-36. [Crossref] [PubMed]
- Calamita G, Gena P, Meleleo D, et al. Water permeability of rat liver mitochondria: A biophysical study. Biochim Biophys Acta 2006;1758:1018-24. [Crossref] [PubMed]


