Mid-term outcomes of titanium modular neck femoral stems in revision total hip arthroplasty
Introduction
The incidence of revision total hip arthroplasty (THA) is increasing worldwide due to an aging population and expansion of indications for primary THA (1). It has been estimated in 2016 that revision THA represented nearly 15% of all hip arthroplasty procedures in the United States and is projected to increase by 137% by 2030 (1). Different stem designs have been proposed for revision THA, including standard (primary) stems, long stems, modular or distally locked stems, either cemented or uncemented (2-4).
Modular stems have been studied by many authors as they allow intraoperative adjustments of femoral neck anteversion, offset, and limb length to better restore muscle tensions and hip biomechanics (5-8). In primary THA, several modular stems have been associated with corrosion or fracture at their junctions, though models made of titanium bodies and necks seem to obviate these problems, and grant satisfactory mid-term survival and excellent clinical outcomes at 10 years (9).
Many authors reported outcomes of revision THA using modular stems with metaphyseal-diaphyseal junctions, and though several authors investigated modular neck femoral stems (MNFS) with metaphyseal-epiphyseal junctions for primary THA, only one study evaluated their outcomes for revision THA (10). The purpose of this study was therefore to report clinical outcomes and implant survival of a MNFS in a consecutive series of revision THA at a minimum follow-up of 5 years.
Methods
The authors reviewed a consecutive series of revision THAs performed between February 2010 and March 2012. The inclusion criteria covered both single- and multi-stage revision THAs performed using an uncemented modular stem (Optimal®, Amplitude, Valence, France). The exclusion criteria were femoral or acetabular deformities, documented prior to the index THA, due to congentital hip dysplasia or previous fracture malunions. Eleven hips underwent femoral revision only, while seventeen hips underwent femoral and acetabular revisions, for which an uncemented dual mobility cup was used (Saturne®, Amplitude, Valence, France) (Table 1).

Full table
Implant
The femoral stem used has an anatomical design with 4° metaphyseal anteversion and anterior curvature of femoral shaft. The stem body is made of anodized titanium and is coated with hydroxyapatite (HA) along its superior two-thirds (Figure 1). The stem body is available in standard and long versions and can be locked distally with one or two threaded pins. The modular necks are also made of anodized titanium and feature two Morse tapers: the upper for the neck-to-head junction and the lower for the neck-to-body junction. The modular necks are available in different lengths, anteversions and neck shaft angles (NSA), allowing 24 different combinations for hip reconstruction.
Surgical technique
The indications for revision of the stem were femoral aseptic loosening in 15 hips (53.6%), femoral periprosthetic fracture (PPF) in 10 hips (35.7%), and infection in 3 hips (10.7%). Femoral bone loss of Paprosky (11) grade I in 13 hips (46.4%), grade II in 6 hips (21.4%), grade IIIA in 4 hips (14.3%), grade IIIB in 4 hips (14.3%), and grade IV in 1 hip (3.6%). All patients were operated through a posterolateral approach. The femoral stem implantation is divided in two steps: the intramedullary implantation of the stem with a classic ‘press-fit’ method, and the extramedullary choice of modular neck to reconstruct the native centre of rotation. Stems were locked distally using one threaded pin in 1 hip (3.6%) and using two threaded pins in 19 hips (67.9%).
Rehabilitation
Structured physical therapy with passive and active motion exercises of the hip started the day after surgery and continued during hospitalization. Patients could walk using two crutches or a walker with partial weight-bearing on the operated limb for 6 weeks post-operatively and full weight bearing thereafter.
Postoperative assessment
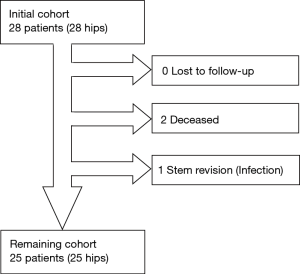
Patients were evaluated during their routine follow-up visits. If patients were deceased, their general practitioner was contacted to confirm the date and cause of death, and whether any of their THA components had been revised. From the initial 28 patients, 1 patient (3.6%) had isolated stem revision, and 2 patients (7.1%) had died with their original stems in place (Figure 2). This left a study cohort of 25 patients living with their original components at a mean follow-up of 68.4±7.4 months (range, 60.0–82.0 months), aged 67.7±11.6 years (median, 68.8 years; range, 36.5–83.7 years) at index operation that were assessed both clinically and radiographically.
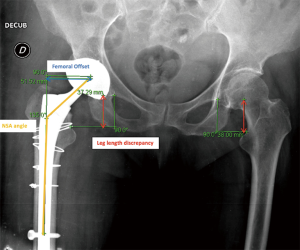
The final cohort was clinically evaluated using the Harris Hip Score (HHS) (12) and the Postel Merle d’Aubigné score (PMA) (13). Patients were evaluated radiographically, on anteroposterior plain radiographs, to assess NSA, femoral offset, limb length discrepancy (LLD, measured by the distance between the U-landmark to the lesser trochanter), as well as the position of the centre of rotation in the horizontal and vertical directions according to the Pierchon index (14-16) (Figure 3). Radiolucent lines >2 mm wide and LLD ≥10 mm were considered as adverse radiographic findings. All X-rays were performed in the standing position with controlled rotation of the lower limb. The anatomical parameters of the operated hip were compared to the contralateral native hip using Centricity™ software (GE Healthcare, Barrington, IL, USA). Radiological features suggesting corrosion due to modular necks were defined as periprosthetic proximal femoral osteolysis in Gruen zones 1 and 7 (17). PPF were classified according to Masri et al. (18) (Vancouver classification).
Statistical analysis
Shapiro-Wilk tests were used to assess the normality of distributions. Differences between operated hips and contralateral hips were evaluated using the t-test for gaussian quantitative data or using Wilcoxon rank-sum test for non-gaussian quantitative data. Paired t-test (for gaussian data) or Wilcoxon signed rank test (for non-gaussian data) were used to evaluate differences between pre- and postoperative quantitative data. Implant survival was assessed using the Kaplan-Meier (KM) method with stem revision for any reason as endpoint. Statistical analyses were performed using R version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria). P values <0.05 were considered statistically significant.
Results
Clinical and Radiographic assessments
The HHS improved from 39.1±19.2 (median, 35.0; range, 7.0–83.0) preoperatively to 78.1±18.3 (median, 81.0; range, 26.0–100.0) post-operatively (P<0.001) (Table 2). Likewise, the PMA score improved from 9.8±3.0 (median, 10.0; range, 4.0–15.0) preoperatively to 14.8±2.8 (median, 16.0; range, 8.0–18.0) post-operatively (P<0.001).
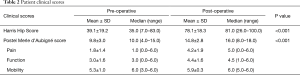
Full table
At last follow-up, the mean LLD was 4.3±5.0 mm (median, 1.5 mm; range, 0–16.4 mm). The LLD was >5 mm in 45.5%, and >10 mm in 18%. The HHS was almost equal in hips with LLD >10 mm than to those with LLD <10 mm (78.5±11.6 vs. 78.2±20.3, respectively; P=0.701). There were no significant differences of femoral offset and NSA between operated and contralateral hips (Table 3).

Full table
Radiolucent lines were observed distally (Gruen zones 3, 4 and 5) around 5 stems (20.0%) and proximally (Gruen zones 1, and 7) around 1 stem (4.0%). Considering the pre-revision osteolysis, only 2 hips (8.0%) showed new periprosthetic radiolucent lines, both of which were located distally.
Complications
One revision (3.6%) was performed during the study period, with retrieval of the revision stem for acute periprosthetic infection, which occurred 27 months after surgery. Periprosthetic fractures (PPF) occurred in 3 hips (12%), of which 2 were graded B2 (8.0%) and 1 graded C (4.0%). No subluxations, dislocations or implant breakages were reported.
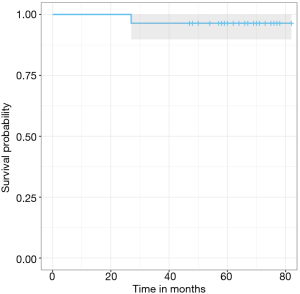
Survival
Using the KM method and stem revision for any reason as endpoint, survival at 5 years was 96.0% (95% confidence interval, 90% to 100%) (Figure 4).
Discussion
The principal finding of this study was that using MNFS in revision THA demonstrated satisfactory clinical outcomes and survival rate at a minimum follow-up of 5 years. To our knowledge, this is the first study to report clinical and radiographic outcomes of revision THA using femoral stems with metaphyseal-epiphyseal modular junctions.
Our reported postoperative HHS of 78.1 and PMA of 14.8 compare well with scores published in other studies of revision THA using modular stems: 69.0–93.0 and 7.0–16.7 respectively (Table 4). In our series, LLD was <5 mm in 54.5% of the hips, which is within the range of 28–78% reported in the literature (8,24). LLD >10 mm was observed in 4 hips but was not associated with inferior clinical scores.
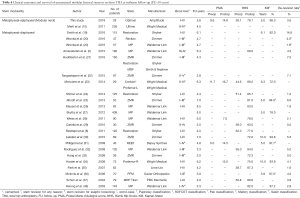
Full table
Badarudeen et al. (39) estimated the global rate of failure in revision THA to be around 15.8%. Springer et al. (40) found that instability was the main cause for failure of revision THA in 35% of the cases. There is still a controversy as to whether modular femoral stems reduce dislocation rates after revising a failed primary THA. Restrepo et al. (8) reported a low dislocation rate of 3%, and attributed it to the use of modular stems, which allowed accurate restoration of the hip architecture. Likewise, Wirtz et al. (41) reported dislocations in 3.5%, which had been successfully managed by exchanging the modular necks, without removing the stem body. However, dislocation rates were found to be higher in other revision THA series using modular stems, ranging from 9% (25) to 19% (28). Regis et al. (42) stated that modular stems alone are not effective in decreasing the risk of dislocation. In our series, the absence of dislocations could be attributed to adequate restoration of the native hip architecture allowed by the modular necks (used for all hips) and to the improved joint stability granted by dual mobility cups (used in 60% of hips) (43).
Postoperative PPF occurred in 3 hips (12%) and were of grade B in 2 hips and of grade C in 1 hip. Our PPF rate is higher than the 2–5% rate reported by Restrepo et al. (8) and Huddleston et al. (21). This higher rate can be due to the use of anatomic stems, which are known to be more filling than straight stems (44). Moreover, it is worth noting that one of the three hips with PPF had severe preoperative bone loss (Paprosky IIIb).
We found no new radiolucent lines in the femoral metaphysis suggesting that there were no corrosion signs at the neck-stem junction. Such as previous published studies (8,25,37), we found no complications related to the Morse taper junction. Fretting and corrosion occurred on all modular neck-stem regardless of design, but homogenous metal couples suffered less from corrosion than mixed couples (45). As in our series, titanium-titanium junctions appeared to be a suitable solution to corrosion issues (45-48).
The MNFS KM survival at 5 years of 96% is within the 72–97.2% survival range at 3.3–7 years reported in other studies (19,23,27,30,34,38) using modular stems revision for any reason as endpoint (Table 4). It is worth noting that most of these published studies on revision THA investigated a femoral stem designed with a metaphyseal-diaphyseal junction, while we analysed a femoral stem designed with a metaphyseal-epiphyseal junction (modular neck). It is still controversial whether modular stems in revision THA are more efficient than monolithic stems. Huddleston et al. (21) reported lower revision rate for modular stems, whilst Mertl et al. (10) found a higher rate of failure for MNFS. However, compared to monolithic stems, modular implants greatly simplify strategies for revision THA and following failures of revision as the modular neck can be removed, facilitating exposure and replaced easily to adapt offset, limb length and NSA while leaving the intra-medullary part of the stem stably fixed within the femur, which has relatively good bone quality at mid-term follow-up (42,49-51).
The current study has some limitations. First, it is a retrospective study with a small sample size. However, series of revision THA in the literature are usually small (3,23,29,52). Second, though none of the patients showed or reported any adverse reactions or symptoms of metallosis, we did not test serum metal ion levels to demonstrate that these were within normal safe ranges. Further studies with longer follow-up and greater sample size will be needed to confirm our findings. Nevertheless, this study is the first to report clinical and radiographic outcomes of a unique modular stem design in revision THA.
Conclusions
The Optimal® uncemented modular neck stem seems to provide a satisfactory survival and satisfactory clinical outcomes at 5 years, with no noticeable adverse effects resulting from the additional modular junction. In this series, neck modularity enabled restoration of patient-specific femoral offset and limb length, though greater follow-up is required to confirm the long-term benefits and safety of this design concept.
Acknowledgements
The authors are grateful to Prof. J Bejui-Hugues, Prof. JP Carret, Prof. O Guyen, Prof. F Rongieras for providing data, and to Mr. J Creton for his help in statistical analyses.
This work was supported by Amplitude SAS, Valence, France.
Footnote
Conflicts of Interest: Dr. Ouanezar received fees for consulting from Amplitude SAS during the conduct of the study; Dr. Pibarot received royalties from Amplitude SAS; Dr. Piton is a consultant for Amplitude SAS. The other authors have no conflicts of interest to declare.
Ethical Statement: All patients provided informed consent for the use of their data for research and publications and the study was performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Guild GN 3rd, Runner RP, Rickels TD, et al. Anthropometric Computed Tomography Reconstruction Identifies Risk Factors for Cortical Perforation in Revision Total Hip Arthroplasty. J Arthroplasty 2016;31:2554-8. [Crossref] [PubMed]
- Amanatullah DF, Howard JL, Siman H, et al. Revision total hip arthroplasty in patients with extensive proximal femoral bone loss using a fluted tapered modular femoral component. Bone Joint J 2015;97-b:312-7.
- Pinaroli A, Lavoie F, Cartillier JC, et al. Conservative femoral stem revision: avoiding therapeutic escalation. J Arthroplasty 2009;24:365-73. [Crossref] [PubMed]
- Reikeras O. Femoral revision surgery using a fully hydroxyapatite-coated stem: a cohort study of twenty two to twenty seven years. Int Orthop 2017;41:271-5. [Crossref] [PubMed]
- Benazzo FM, Piovani L, Combi A, et al. MODULUS Stem for Developmental Hip Dysplasia: Long-term Follow-up. J Arthroplasty 2015;30:1747-51. [Crossref] [PubMed]
- Cooper HJ, Urban RM, Wixson RL, et al. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am 2013;95:865-72. [Crossref] [PubMed]
- Lanting BA, Teeter MG, Vasarhelyi EM, et al. Correlation of corrosion and biomechanics in the retrieval of a single modular neck total hip arthroplasty design: modular neck total hip arthroplasty system. J Arthroplasty 2015;30:135-40. [Crossref] [PubMed]
- Restrepo C, Mashadi M, Parvizi J, et al. Modular femoral stems for revision total hip arthroplasty. Clin Orthop Relat Res 2011;469:476-82. [Crossref] [PubMed]
- Collet T, Atanasiu JP, de Cussac JB, et al. Midterm outcomes of titanium modular femoral necks in total hip arthroplasty. Ann Transl Med 2017;5:395. [Crossref] [PubMed]
- Mertl P, Philippot R, Rosset P, et al. Distal locking stem for revision femoral loosening and peri-prosthetic fractures. Int Orthop 2011;35:275-82. [Crossref] [PubMed]
- Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res 2004.55-62. [Crossref] [PubMed]
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737-55. [Crossref] [PubMed]
- d'Aubigne RM, Postel M. The classic: functional results of hip arthroplasty with acrylic prosthesis. 1954. Clin Orthop Relat Res 2009;467:7-27. [Crossref] [PubMed]
- Lecerf G, Fessy MH, Philippot R, et al. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res 2009;95:210-9. [Crossref] [PubMed]
- Meermans G, Malik A, Witt J, et al. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clin Orthop Relat Res 2011;469:1677-82. [Crossref] [PubMed]
- Pierchon F, Migaud H, Duquennoy A, et al. Radiologic evaluation of the rotation center of the hip. Rev Chir Orthop Reparatrice Appar Mot 1993;79:281-4. [PubMed]
- Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 1979.17-27. [PubMed]
- Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res 2004.80-95. [Crossref] [PubMed]
- Smith MA, Deakin AH, Allen D, et al. Midterm Outcomes of Revision Total Hip Arthroplasty Using a Modular Revision Hip System. J Arthroplasty 2016;31:446-50. [Crossref] [PubMed]
- Wronka KS, Cnudde PH. Midterm results following uncemented, modular, fully porous coated stem used in revision total hip arthroplasty: Comparison of two stem systems. J Orthop 2016;13:298-300. [Crossref] [PubMed]
- Huddleston JI 3rd, Tetreault MW, Yu M, et al. Is There a Benefit to Modularity in 'Simpler' Femoral Revisions? Clin Orthop Relat Res 2016;474:415-20. [Crossref] [PubMed]
- Tangsataporn S, Safir OA, Vincent AD, et al. Risk Factors for Subsidence of a Modular Tapered Femoral Stem Used for Revision Total Hip Arthroplasty. J Arthroplasty 2015;30:1030-4. [Crossref] [PubMed]
- Menciere ML, Wissocq N, Krief E, et al. Mid-term outcomes after distally locked-to-standard primary stem exchange in 29 hip-prosthesis patients. Orthop Traumatol Surg Res 2014;100:135-40. [Crossref] [PubMed]
- Stimac JD, Boles J, Parkes N, et al. Revision total hip arthroplasty with modular femoral stems. J Arthroplasty 2014;29:2167-70. [Crossref] [PubMed]
- Jibodh SR, Schwarzkopf R, Anthony SG, et al. Revision hip arthroplasty with a modular cementless stem: mid-term follow up. J Arthroplasty 2013;28:1167-72. [Crossref] [PubMed]
- Klauser W, Bangert Y, Lubinus P, et al. Medium-term follow-up of a modular tapered noncemented titanium stem in revision total hip arthroplasty: a single-surgeon experience. J Arthroplasty 2013;28:84-9. [Crossref] [PubMed]
- Skytta ET, Eskelinen A, Remes V. Successful femoral reconstruction with a fluted and tapered modular distal fixation stem in revision total hip arthroplasty. Scand J Surg 2012;101:222-6. [Crossref] [PubMed]
- Weiss RJ, Beckman MO, Enocson A, et al. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty 2011;26:16-23. [Crossref] [PubMed]
- Canella RP, de Alencar PG, Ganev GG, et al. Revision Total Hip Arthroplasty Using a Modular Cementless Distal Fixation Prosthesis: The Zmr(®) Hip System. Clinical and Radiographic Analysis of 30 Cases. Rev Bras Ortop 2015;45:279-85. [Crossref] [PubMed]
- Lakstein D, Backstein D, Safir O, et al. Revision total hip arthroplasty with a porous-coated modular stem: 5 to 10 years follow-up. Clin Orthop Relat Res 2010;468:1310-5. [Crossref] [PubMed]
- Philippot R, Delangle F, Verdot FX, et al. Femoral deficiency reconstruction using a hydroxyapatite-coated locked modular stem. A series of 43 total hip revisions. Orthop Traumatol Surg Res 2009;95:119-26. [Crossref] [PubMed]
- Rodriguez JA, Fada R, Murphy SB, et al. Two-year to five-year follow-up of femoral defects in femoral revision treated with the link MP modular stem. J Arthroplasty 2009;24:751-8. [Crossref] [PubMed]
- Kang MN, Huddleston JI, Hwang K, et al. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty 2008;23:220-5. [Crossref] [PubMed]
- Koster G, Walde TA, Willert HG. Five- to 10-year results using a noncemented modular revision stem without bone grafting. J Arthroplasty 2008;23:964-70. [Crossref] [PubMed]
- Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty 2007;22:993-9. [Crossref] [PubMed]
- McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty 2006;21:372-80. [Crossref] [PubMed]
- Schuh A, Werber S, Holzwarth U, et al. Cementless modular hip revision arthroplasty using the MRP Titan Revision Stem: outcome of 79 hips after an average of 4 years' follow-up. Arch Orthop Trauma Surg 2004;124:306-9. [Crossref] [PubMed]
- Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty 2003;18:94-7. [Crossref] [PubMed]
- Badarudeen S, Shu AC, Ong KL, et al. Complications After Revision Total Hip Arthroplasty in the Medicare Population. J Arthroplasty 2017;32:1954-8. [Crossref] [PubMed]
- Springer BD, Fehring TK, Griffin WL, et al. Why revision total hip arthroplasty fails. Clin Orthop Relat Res 2009;467:166-73. [Crossref] [PubMed]
- Wirtz DC, Heller KD, Holzwarth U, et al. A modular femoral implant for uncemented stem revision in THR. Int Orthop 2000;24:134-8. [Crossref] [PubMed]
- Regis D, Sandri A, Bartolozzi P. Stem modularity alone is not effective in reducing dislocation rate in hip revision surgery. J Orthop Traumatol 2009;10:167-71. [Crossref] [PubMed]
- Romagnoli M, Grassi A, Costa GG, et al. The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: a systematic review and meta-analysis of comparative studies. Int Orthop 2018. [Epub ahead of print]. [Crossref] [PubMed]
- de Boer FA, Sariali E. Comparison of anatomic vs. straight femoral stem design in total hip replacement - femoral canal fill in vivo. Hip Int 2017;27:241-4. [Crossref] [PubMed]
- Su SL, Koch CN, Nguyen TM, et al. Retrieval Analysis of Neck-Stem Coupling in Modular Hip Prostheses. J Arthroplasty 2017;32:2301-6. [Crossref] [PubMed]
- Blakey CM, Eswaramoorthy VK, Hamilton LC, et al. Mid-term results of the modular ANCA-Fit femoral component in total hip replacement. J Bone Joint Surg Br 2009;91:1561-5. [Crossref] [PubMed]
- Ollivier M, Parratte S, Galland A, et al. Titanium-titanium modular neck for primary THA. Result of a prospective series of 170 cemented THA with a minimum follow-up of 5 years. Orthop Traumatol Surg Res 2015;101:137-42. [Crossref] [PubMed]
- Traina F, De Fine M, Tassinari E, et al. Modular neck prostheses in DDH patients: 11-year results. J Orthop Sci 2011;16:14-20. [Crossref] [PubMed]
- Earll MD, Fehring TK, Griffin WL, et al. Success rate of modular component exchange for the treatment of an unstable total hip arthroplasty. J Arthroplasty 2002;17:864-9. [Crossref] [PubMed]
- Jang HG, Lee KJ, Min BW, et al. Mid-term Results of Revision Total Hip Arthroplasty Using Modular Cementless Femoral Stems. Hip Pelvis 2015;27:135-40. [Crossref] [PubMed]
- Toomey SD, Hopper RH Jr, McAuley JP, et al. Modular component exchange for treatment of recurrent dislocation of a total hip replacement in selected patients. J Bone Joint Surg Am 2001;83-A:1529-33. [Crossref] [PubMed]
- Cavagnaro L, Formica M, Basso M, et al. Femoral revision with primary cementless stems: a systematic review of the literature. Musculoskelet Surg 2018;102:1-9. [PubMed]