
Initial treatment combined with Prunella vulgaris reduced prednisolone consumption for patients with subacute thyroiditis
Introduction
Subacute thyroiditis (SAT) is a transient inflammatory and nonsuppurative thyroid disease, also known as painful SAT, subacute granulomatous thyroiditis, or de Quervain’s thyroiditis, and is likely related to viral infection or autoimmune response. Patients with SAT usually have a history of a proceeding systemic illness with a moderate enlargement of their thyroid which has been associated with parenchymal destruction in large phagocytic cells (1,2). A few patients with SAT might show mild symptoms which can be treated with nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin. For others who suffer severe pain in the thyroid region and have a high fever, a high dose of oral glucocorticoids (prednisolone, PSL) can be considered necessary (2). PSL at 40 mg/d has been recommended for the treatment of SAT. Although the application of a high dose of PSL previously provided dramatic relief for both pain and fever, the recurrence rate remained high after treatment, and the continuing side effects resulting from the high dosage were disturbing.
In traditional Chinese medicine, SAT was mainly treated by dispelling wind, clearing away heat, resolving phlegm, and removing mass (3). Selfheal® (Xianhe Pharmacy, Prunella vulgaris, Dongying, Shandong, China), commonly known as Prunella vulgaris (PV), has a long history of application in traditional Chinese and Western medicine as a remedy for sore throat, swelling of the thyroid gland, fever, and general wounds. Studies have confirmed that PV could suppress inflammation via several signal transduction pathways (4). Therefore, PV was adopted at our center to achieve a better prognosis of SAT patients and reduce the dosage of PSL to avoid side effects. Promising results were noted, thus, in the present study, we retrospectively analyzed the effectiveness and safety of the new treatment protocols for SAT, consisting of PV extract and low-dosage PSL.
Methods
Patients and methods
Data regarding the untreated patients with SAT who visited our thyroid clinic at the First Affiliated Hospital, School of Medicine, Zhejiang University, between September 2013 and May 2016 were retrospectively analyzed. Patient characteristics including age, sex, body weight, C-reactive protein (CRP), serum thyrotropin (TSH), serum-free thyroxine, B ultrasound (BUS) data, and pain score were collected. The patients were followed up at 4, 8 weeks and 6 months after treatment. If the patient’s pain score decreased to less than 3 points, and a reduction in the level of C-reactive protein and area of the hypoechoic lesion in thyroid were also noted, then the patient would be considered as being in clinical remission.
Diagnosis of SAT
SAT was diagnosed on the basis of pain and tenderness in the thyroid gland or radiating pain, and laboratory findings of abnormity of CRP, serum-free triiodothyronine (FT3) and tetraiodothyronine (FT4), serum thyrotropin (TSH), anti-thyroid peroxidase antibodies (TPOAb) and hypoechoic lesion in thyroid gland on BUS. The diagnosis was made according to the criteria established by the Society of Endocrine of Chinese Medical Association (5).
Treatment protocols
The patients treated with PSL alone or combined with PV were divided into two groups. Patients treated with PSL alone were divided into the control group. Others received 10 mg/day of PSL combined with 1.4 g/day of PV® (Xianhe Pharmacy, Prunella vulgaris, Dongying, Shandong, China). The PSL was reduced 5 mg/day every 3 weeks and withdrawn at 6 weeks after treatment. Patients found to have tachycardia were treated with propranolol.
Ethical statement
Written informed consent was obtained from all participants. Ethical approval was obtained from the Ethics Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University (Reference Number. 2018-723), and the study was performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. All of the data were analyzed anonymously and identified before analysis.
Statistics
Statistical analysis was performed using the Statistical Package for the Social Sciences 19.0® (SPSS Inc., Chicago, Il, USA). Data are presented as the mean ± the standard deviation (SD) or counts. Categorical variables were determined by the Fisher’s exact test or Chi-square test. Continuous variables were compared by Student’s t-tests or Wilcoxon rank-sum test. A P value of <0.05 was considered statistically significant.
Results
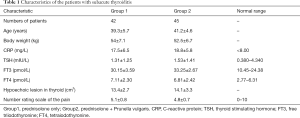
In total, data from 126 patients were collected. Thirty-one patients who were only treated with NSAIDs and 8 patients who were intolerable of PSL because of gastric ulcers or diabetes mellitus, were excluded. Consequently, 87 patients were included in our study and divided into two groups depending on whether or not they received PV to treat the SAT. No significant difference regarding the patient characteristics before treatment, including serum CRP, sex, body weight, age, and lesion area, were noted between the two groups (Table 1). Thyroid hormone (FT4 and FT3) and CRP levels measured at the initial visit were above normal range (Table 1).
Full table
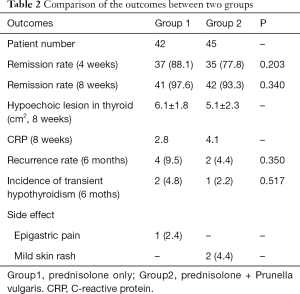
In total, thyroiditis in 72 patients had improved within 4 weeks, and 83 improved within 6–8 weeks after treatment. No difference regarding the remission rate between the two groups was noted (P=0.203 and P=0.340, respectively, Table 2). The hypoechoic lesions in thyroid gland were all downsized more than 1/2 (Tables 1,2). The CRP levels significantly decreased in both groups. The longest treatment duration was 31 weeks. Five patients in group 2 needed an increased dose of PSL: 30 mg was required in 2 patients, and 20 mg was required in 3. Five patients took PSL for more than 7 weeks. Four patients (9.5%) in group 1 and 2 (4.4%) in group 2 recurred within 6 months (P=0.350, Table 2). Two patients (4.8%) in group 1 and 1 (2.2%) in group 2 underwent transient hypothyroidism within 6 months (P=0.517, Table 2).
Full table
One patient receiving only PSL complained of epigastric pain, which was considered to be caused by a high dose of PSL, and two patients complained of mild skin rash caused by PV. They were treated accordingly and completely recovered soon after. The overall incidences of the side effects in the two groups were 2.4% and 4.4%, respectively, and no significant difference was found (P=0.673) (Table 2).
Discussion
SAT often occurs along with a viral infection; however, no specific virus has been identified. Although SAT is a self-limited disease, it can still last 6–12 months and often cause intolerable pain. The recurrence rate of SAT after treatment was found to be about 20%, and 10–15% of patients suffered from permanent hypothyroidism even with treatment (2,3,6). No consensus regarding the treatment of SAT has been reached thus far. For severe and protracted cases, the American Thyroid Association and American Association of Clinical Endocrinologists recommended 40 mg/day of PSL as the initial dosage for the treatment (7). In China, 20–40 mg/day was recommended (5). A dosage of between 20–65 mg/day of PSL was the most commonly encountered in the initial treatment of SAT (8-10).
Adoption of PSL may be able to effectively relieve pain and other systematic symptoms. However, in a few patients initially treated with a long duration and a large dosage of PSL, once the SAT has recurred, the patients must receive a higher dosage to once again control the symptoms. These patients were reported to be constantly troubled by hypertrichiasis and acne caused by PSL. Thus, it was crucial to take strict control of the application of PSL and find alternative substances for glucocorticoids to reduce the dosage, or even replace the PSL.
In traditional Chinese medicine, SAT was considered to be caused by wind-heat, internal emotional injuries, stagnation of liver-Qi, and thus should be treated by dispelling wind, clearing away heat, resolving phlegm, and removing mass. Luo H showed that Chinese herbal medicine alone or combined with Western medicine improved the therapeutic efficacy of SAT, and reduced the incidence of hypothyroidism, the side effects of glucocorticoids and recurrence rate of SAT (11). PV, or so-called “selfheal”, is a traditional herb which has the potential to cure photophobia, ocular pain, mastitis, mastocarcinoma, lymphoid tuberculosis, parotitis, hepatitis, etc. It has been reported to have anti-inflammatory, antiviral, and antibacterial effects (12,13).
Aiming at finding a new therapeutic scheme for SAT with a better outcome and less adverse effects, the PV extract was adopted in our center. In the present study, we employed a dosage of 20 mg/day of PSL alone as the initial dosage for the treatment of SAT. The patients were also provided the alternative of 10 mg/day of PSL combined with 1.4 g/day PV which would only be adopted if consent were obtained. The results showed that the new combination of PSL and PV alleviated the fever, pain, thyroid swelling more efficiently, and had a lower recurrence rate. This improvement might owe to the immunosuppression and antiviral function of PV.
SAT is triggered by an autoimmune response with the release of colloids. After the virus injures the thyroid follicles, the immune response initiates and causes SAT. The active components of the extract of PV consists of four triterpenes, including betulinic acid, ursolic acid, 2α, 3α-dihydroxyurs-12-en-28-oic acid, and 2α-hydroxyursolic acid. These compounds exhibit strong anti-allergic and anti-inflammatory activities (13). Also, it has been shown that PV up-regulated T-lymphocyte subsets in peripheral blood to inhibit the replication of the virus and suppress innate and adaptive immunity (14).
Conclusions
In summary, the combination of 10 mg/day of PSL and 1.4 g/d PV as the initial dosage for the treatment of SAT with a degression of 5 mg every 3 weeks was effective and safe. These results thus indicate that combining a low dose of PSL and PV together can be viable as a treatment for SAT.
Acknowledgements
Funding: The research study was supported by the Health Department of Zhejiang Province (#2013KYA075) and the Zhejiang Provincial Natural Science Foundation of China (LY19H070004).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from the Ethics Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University (Reference Number. 2018-723), and the study was performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from all participants.
References
- Volpé R. The management of subacute (Dequervain) thyroiditis. Thyroid 1993;3:253-5. [Crossref] [PubMed]
- Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003;348:2646-55. [Crossref] [PubMed]
- China Association of Traditional Chinese Medicine. Guide for diagnosing and treating common diseases in surgical department of Traditional Chinese Medicine. Beijing: China Press of Traditional Chinese Medicine 2012:43-5.
- Hwang YJ, Lee EJ, Kim HR, et al. NF-κB-targeted anti-inflammatory activity of Prunella vulgaris var. lilacina in macrophages RAW 264.7. Int J Mol Sci 2013;14:21489-503. [Crossref] [PubMed]
- Chinese Society of Endocrinology. Chinese guideline for thyroid disease- thyroiditis. Chin J Intern Med 2008;47:784-8.
- Kujat C, Dyck R, Brederhoff J, et al. Diagnosis and treatment of (Dequervain) subacute thyroiditis. Dtsch Med Wochenschr 1991;116:1439-43. [Crossref] [PubMed]
- Bahn Chair RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid 2011;21:593-646. [Crossref] [PubMed]
- Mizukoshi T, Noguchi S, Murakami T, et al. Evaluation of recurrence in 36 subacute thyroiditis patients managed with prednisolone. Intern Med 2001;40:292-5. [Crossref] [PubMed]
- Vagenakis AG, Abreau CM, Braverman LE. Prevention of recurrence in acute thyoiditis following corticosteroid withdrawal. J Clin Endocrinol Metab 1970;31:705-8. [Crossref] [PubMed]
- Fatourechi V, Aniszewski JP, Fatourechi GZE, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab 2003;88:2100-5. [Crossref] [PubMed]
- Luo H, Lü M, Pei X, et al. Chinese herbal medicine for subacute thyroiditis: a systematic review of randomized controlled trials. J Tradit Chin Med 2014;34:243-53. [Crossref] [PubMed]
- Psotová J, Kolár M, Sousek J, et al. Biological activities of Prunella vulgaris extract. Phytother Res 2003;17:1082-7. [Crossref] [PubMed]
- Ryu SY, Oak MH, Yoon SK, et al. Anti-allergic and anti-inflammatory triterpenes from the herb of Prunella vulgaris. Planta Med 2000;66:358-60. [Crossref] [PubMed]
- Zheng Y, Qiao C, Yuan W. Influnce of Selfheal Capsule on the Expression of Subsets of T Lymphocyte in Peripheral Blood of Rats with Ulcerative Colitis. Chin J Integr Trad West Med Dig 2004;12:10-2.


