Long-term effects of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: systematic review and single-arm meta-analyses
Introduction
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is one of the most common urologic problems among men younger than 50 years old (1-4). It is characterized by a diverse range of pain and inflammatory symptoms that involve the region of the pelvis, perineum, scrotum, rectum, testes, and penis, in the absence of positive urine culture (5). In addition to the principal diagnostic pelvic pain or discomfort, CP/CPPS is often associated with negative cognitive, sexual, and emotional consequences (6).
To date, the pathophysiological mechanisms underlying CP/CPPS are still poorly understood, and the appropriate and effective therapies are lacked (7). The mainstream oral drugs such as antibiotics, alpha-blockers or combinations of these drugs for CP/CPPS treatment are empirical and directed toward improving a hypothetical condition that may be associated with relevant symptoms including pelvic pain and lower urinary tract symptoms (8). Although aforementioned therapies have moderate effect regarding NIH-CPSI score reductions (9), their sustained effects were unclear (10).
Cumulative evidences obtained from RCTs and meta-analyses indicate that acupuncture could ameliorate the symptoms of CP/CPPS, particularly in relieving pain (11-14). However, the long-term effects of acupuncture on CP/CPPS has not been fully studied because few RCTs assessed the sustained effects of acupuncture specially, and the published meta-analyses did not clearly define ‘long-term’ as well (9). According to the study of Carlsson, the long-term effects that clinically relevant of acupuncture for pain relieving should be assessed more than 6 months (15).
Thus, we performed this study to assess the long-term effects of acupuncture for CP/CPPS through eligible RCTs and observational studies which set the follow-up outcome at 6-month. This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (16).
Methods
Sources and search strategy
Two authors (Z Qin and J Wu) independently searched PubMed, EMBASE, and Cochrane CENTRAL Register for Clinical Trials for English-language publications from their inception through December 8, 2017 and updated at May 20, 2018 with following subject headings and text words: “chronic prostatitis” OR “chronic pelvic pain syndrome” OR “CP/CPPS” AND “acupuncture” (see Table S1, which describe the search terms and strategies). In addition, a manual search was performed for relevant systematic reviews and guidelines. Both two authors have over 3 years’ experience in evidence-based practice.

Full table
Eligibility criteria
The following eligibility criteria were specified as followed: (I) the interested population should be patients who have been diagnosed with CP/CPPS; (II) the intervention of acupuncture group should be invasive manual acupuncture or electroacupuncture on the acupoint; (III) both RCTs and observational studies of acupuncture for CP/CPPS were selected for meta-analyses. Observational studies were included because there are few acupuncture related RCTs set long-term follow-up periods; (IV) for those studies to be included should report the outcomes at 6-month or after 6-month. Abstracts, study protocols, commentaries, editorials, and case reports were excluded.
Clinical outcomes
Studies with one of the following outcomes were included. The NIH-CPSI [range from 0 (best) –43 (worst)] measures 3 most important symptom domains of CP/CPPS: pain (location, frequency, and severity; range from 0–21), urinary symptoms (irritating and obstructive symptoms; range from 0–10), and negative effects on quality of life (range from 0–12) (17). The primary outcome was the response rate of acupuncture at the end of follow-up. The responder of long-lasting acupuncture treatment was defined as the person who has at least 50% decreases in the NIH-CPSI score from baseline at the end of follow-up. The secondary outcomes were the changes in NIH-CPSI total score and NIH-CPSI subscale scores referring to pain, urinary symptoms, and impact on quality of life at the end of follow-up.
Study selection
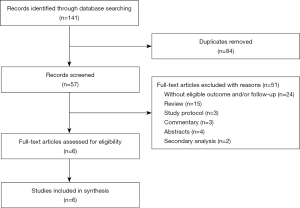
The flow chart for study selection is shown in Figure 1. Two authors (Z Qin and J Wu) screened the literature independently. At the first step, title and abstract were viewed by one author (Z Qin) exclude studies obviously out of the scope. Another author (C Xu) checked the excluded records to ensure there was no mis-operation. Then, the two authors read the full-text of the remaining studies to make the final judgement.
Data extraction
Two authors (Z Qin and J Wu) extracted data from selected studies using an electronic standardized data extraction form. Any disagreements were solved by consensus. Study characteristics, patient characteristics, acupuncture types, acupoints selection, and various efficacy outcomes were summarized. If the study did not provide the change value of the estimators (from baseline to the end of follow-up), we calculated it using the formula provided in Cochrane Handbook (18). For studies only provide graphs without the exact numerical data, we estimated the missing data using GetData Graph Digitizer version 2.26 (19). For studies compared different types of acupuncture, we extracted the data from both groups.
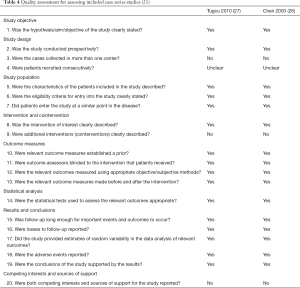
Quality assessment
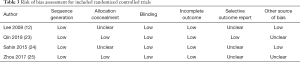
Quality assessment of RCTs and case series studies were conducted according to the tools for RCTs and case series, respectively (18,20). We used the Cochrane Collaboration tool to evaluate the risk of bias for the RCTs included. In addition, a tool developed by Moga and his colleagues was used for assessing case series studies, which consists of 20 items and can systematically evaluate the case series studies (21). Two reviewers (Z Qin and J Wu) evaluated the adequacy of random sequence generation and allocation concealment, blinding of participants, outcomes assessors, incomplete outcome data, selective reporting, and other biases.
Statistical analysis
Statistical analyses were conducted using Stata version 13.0 (StataCorp LP). We pooled the categorical variables as proportion, and the continuous variables as mean difference (MD), both with 95% confidence intervals (CIs). Random-effect model was used for analysis, with the underlying assumption that data comes from varied populations with different distributions, given the potential heterogeneous response rate across studies. The magnitude of heterogeneity was measure by I2 statistic, that is, the ratio of between-study variance to the total variance. A larger I2 means higher heterogeneity and I2>50% indicates there is substantial heterogeneity. For the primary outcome, sensitivity analysis was conducted to identify the source of heterogeneity, this was followed by classified different types of studies, low quality studies (if exist), as well as studies with small sample size (less than 15 participants per group). For studies having proportion of events more than 80% or less than 20%, we transferred the data using double arcsine method to avoid the anomalous values of 95% CI (22). A two-tailed t-test with alpha of 0.05 was used for the statistical inference.
Results
Description of included studies
After removal of duplicates, 141 citations for eligibility with 57 full-texts were used. A total of 6 studies [four RCTs (12,23-25) and two case series studies (26,27)] were included in qualitative review and meta-analysis (12,23-27). The most common reason for exclusion was that studies without eligible outcome or follow-up. The included trials were from China, Malaysia, Turkey, and Canada. All studies were published in English. Tables 1 and 2 summarize the parameters of included trials. Amongst the include studies, the mean age of the population ranges from 31.4 to 42.4 years; the follow-up ranges from 24 to 34 weeks; and the sample size ranges from 12 to 93 participants.
Full table
Full table
Quality assessment
In general, the quality items of included four RCTs and two case series studies were well reported. For included RCTs, two studies did not report the allocation concealment condition; three studies did not attach research protocol so that we cannot evaluate whether they selectively reported the outcomes; two studies were assessed as unclear risk of bias regarding other possible source of bias owing to the small sample size (Table 3). For case series studies, more than a half items have been checked as positive results (Table 4).
Full table
Clinical outcomes
One RCT reported response rate after 2-week treatment instead of follow-up periods, in addition, its definition of response rate (30% decrease from baseline) was inconsistent with our predefined requirement (50% decrease from baseline) (25). Finally, we selected 5 studies (3 RCTs and 2 case series) including 226 patients into the single-arm meta-analysis in a random-effect model (12,23,24,26,27). The response rates of two studies were higher than 80% (26,27). Therefore, the data was transferred by the double arcsine transformation methods, so as the upper limit of 95% CI will not surpass 1. The pooled response rate was 68.4% (95% CI: 42.1% to 89.5%) after 5 studies were synthesized (12,22,23,25,26). Significant heterogeneity was observed among response rates with an I2 statistic of 93.5%. Sub-groups analyses were conducted to identify the source of heterogeneity among the primary outcome. After classified case series studies from the data combining, the heterogeneity changed from 93.5% to 87.5% with the response rate of 53.9% (95% CI: 29.4% to 77.4%) in the RCTs subgroup (12,23,24); and the heterogeneity decreased to 20.4% with the results of 90.1% (95% CI: 81.2% to 96.5%) in the case series studies subgroup.
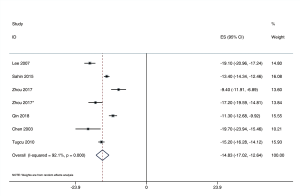
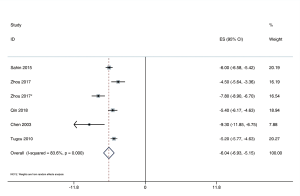
In terms of NIH-CPSI total score, meta-analysis of 6 studies (4 RCTs and 2 case series) enrolled 310 patients were performed (12,23-27), yielding a clinical change in NIH-CPSI score of −14.8 (95% CI: −17.0 to −12.6). Methodologically, the studies were highly heterogeneous with an I2 statistic of 92.1% (Figure 2). Other NIH-CPSI relevant outcomes were reported by 5 studies (3 RCTs and 2 case series studies) with 266 patients (23-27). The changes across all groups was −6.0 (95% CI: −6.9 to −5.2), −2.6 (95% CI: −3.3 to −2.0), and −4.4 (95% CI: −6.2 to −2.6) in NIH-CPSI pain, urinary, and quality of life, respectively. The studies were highly heterogeneous with I2 statistic range from 83.6% to 98.7% (Figures 3-5).
Discussion
Summary of results
The most important finding of our analyses was that the response rate of CP/CPPS to acupuncture treatment was 68.4% (95% CI: 42.1% to 89.5%) after follow-up periods. We also observed clinically significant improvement in the NIH-CPSI total score. The acupuncture group got a clinically meaningful decrease (14.8-point) at the end of follow-up, which is twofold greater than the 6-point threshold (28), illustrating that the long-lasting effects could be a potential advantage of acupuncture in the treatment of CP/CPPS. In terms of NIH-CPSI related sub-scales scores, the changes of pain, urinary symptoms, and quality of life were −6.0, −2.6, and −4.4 at the end of follow-up, respectively. The decrease trends of pain and urinary symptoms after acupuncture in this study were similar to one trial in which acupuncture was demonstrated to alleviate pain symptoms of CP/CPPS better then to relieve urinary symptoms (11). However, owing to the insufficient studies included, the source of heterogeneity cannot be explored. As a result, the evidence of combing data has been limited. The source of heterogeneity may relate to various acupoints selection, treatment sessions, and follow-up periods.
Mechanistic explanations
Similar to other chronic pain, CP/CPPS patients have shown specific patterns of functional and pain-related brain activation and anatomical reorganization, which is correlated with clinical pain intensity (29). Pain-reliving effects of acupuncture on CP/CPPS may involve events in the tissue, spinal cord, and supraspinal levels, encompassing the gate control therapy, regulation of the endogenous opioid system and the purinergic signaling system. Additionally, autoimmunity may be one of the possible explanations for CP/CPPS, characterized by self-recognition by the immune system resulting in immune response destroying or damaging of normal cells and tissues (30,31). Acupuncture may also improve the CP/CPPS symptoms via modulating the activities of immunocytes and the secretion of immune molecules. In 2014, Lee and colleagues hypothesized acupuncture may affect the immune system in CP/CPPS patients and assayed immunological parameters from the patients (n=12 in two arms, with 1:1 ratio) who have been enrolled in a RCT (12,32). The results showed that after 20 weeks treatment, acupuncture decreased leukocytes, neutrophil, lymphocyte, and monocyte; improved the ratio of CD3+, CD4+, CD8+, CD19+, and NK cells compared with baseline, indicating that acupuncture may relief the symptoms via modulating immune system in CP/CPPS (32).
Compared with long-term effects of drugs
Previous network meta-analysis illustrated that mean NIH-CPSI total scores at follow-up changed −11.0 (95% CI: −13.9 to −8.1) for alpha-blockers, −9.8 (95% CI: −15.1 to −4.6) for antibiotics, and −13.8 (95% CI: −17.5 to −10.2) for the combination of alpha-blockers plus antibiotics compared with placebo (33). However, this network meta-analysis did not report the exact follow-up period. Owing to the lack of placebo/sham-controlled group, the results of this study could not exclude placebo effect of acupuncture. Our finding of NIH-CPSI total score at the end of follow-up was similar to the results of the combination therapy.
Limitation
This study has several limitations. Only six studies were included in this single-arm meta-analyses, the insufficient quantity of studies and small sample size limited to conduct the robust evidence; the significant heterogeneity was obvious after data synthesis, the source of heterogeneity was failed to be identified owing to insufficient studies; the missing data was estimated by assuming the correlation coefficient R was 0.5, a conservative value that may lead to the potential higher variance; the mixture of various types of acupuncture, frequency of administration, different acupuncturists, duration of each session, and location of acupoints should have potential impacts on the effects of acupuncture.
Conclusions
In conclusion, the synthesized data showed that clinically significant long-term effects of acupuncture on CP/CPPS patients. However, current evidence is limited by insufficient studies and high heterogeneity. Further studies with large sample size and long-term follow-up periods are warranted.
Acknowledgements
The authors thanks Prof. Joey S. W. Kwong (JC School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong) for her help in improving the methodology and the quality of the manuscript.
Funding: This study has been supported by China Academy of Chinese Medical Sciences (Grant No. ZZ10-012) and the National Natural Science Foundation of China (Grant No. 81430099).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This is a systematic review and meta-analyses, the study did not use any private patient data.
References
- Bartoletti R, Cai T, Mondaini N, et al. Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multicenter case-control observational study. J Urol 2007;178:2411-5; discussion 2415. [Crossref] [PubMed]
- Ejike CE, Ezeanyika LU. Prevalence of chronic prostatitis symptoms in a randomly surveyed adult population of urban-community-dwelling Nigerian males. Int J Urol 2008;15:340-3. [Crossref] [PubMed]
- Ferris JA, Pitts MK, Richters J, et al. National prevalence of urogenital pain and prostatitis-like symptoms in Australian men using the National Institutes of Health Chronic Prostatitis Symptoms Index. BJU Int 2010;105:373-9. [Crossref] [PubMed]
- Liang CZ, Li HJ, Wang ZP, et al. The prevalence of prostatitis-like symptoms in China. J Urol 2009;182:558-63. [Crossref] [PubMed]
- Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA 1999;282:236-7. [Crossref] [PubMed]
- Murphy AB, Macejko A, Taylor A, et al. Chronic prostatitis: management strategies. Drugs 2009;69:71-84. [Crossref] [PubMed]
- Breser ML, Salazar FC, Rivero VE, et al. Immunological Mechanisms Underlying Chronic Pelvic Pain and Prostate Inflammation in Chronic Pelvic Pain Syndrome. Front Immunol 2017;8:898. [Crossref] [PubMed]
- Rees J, Abrahams M, Doble A, et al. Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU Int 2015;116:509-25. [Crossref] [PubMed]
- Engeler. D, Baranowski. AP, Borovicka. J, et al. EAU Guidelines on Chronic Pelvic Pain. Available online: http://uroweborg/guideline/chronic-pelvic-pain/
- Zhao Y, Zhao W, Lang G, et al. Circumcision plus antibiotic, anti-inflammatory, and alpha-blocker therapy for the treatment for chronic prostatitis/chronic pelvic pain syndrome: a prospective, randomized, multicenter trial. World J Urol 2015;33:617-22. [Crossref] [PubMed]
- Lee SH, Lee BC. Use of acupuncture as a treatment method for chronic prostatitis/chronic pelvic pain syndromes. Curr Urol Rep 2011;12:288-96. [Crossref] [PubMed]
- Lee SW, Liong ML, Yuen KH, et al. Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. Am J Med 2008;121:79.e1-7. [Crossref] [PubMed]
- Qin Z, Wu J, Tian J, et al. Network Meta-Analysis of the Efficacy of Acupuncture, Alpha-blockers and Antibiotics on Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Sci Rep 2016;6:35737. [Crossref] [PubMed]
- Qin Z, Wu J, Zhou J, et al. Systematic Review of Acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Medicine (Baltimore) 2016;95:e3095. [Crossref] [PubMed]
- Carlsson C. Acupuncture mechanisms for clinically relevant long-term effects--reconsideration and a hypothesis. Acupunct Med 2002;20:82-99. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1-34. [Crossref] [PubMed]
- Litwin MS, McNaughton-Collins M, Fowler FJ Jr, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol 1999;162:369-75. [Crossref] [PubMed]
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration 2011.
- Fedorov S. GetData Graph Digitizer version 2.26. Available online: http://getdata-graph-digitizer.com/
- Moga C GB, Schopflocher D, Harstall C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique. Edmonton AB: Institute of Health Economics 2012.
- Guo B, Moga C, Harstall C, et al. A principal component analysis is conducted for a case series quality appraisal checklist. J Clin Epidemiol 2016;69:199-207.e2. [Crossref] [PubMed]
- Miller J. The inverse of the Freeman-Tukey double arscine transformation. Am Statistician 1978;32:138.
- Qin Z, Zang Z, Zhou K, et al. Acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized, sham acupuncture-controlled trial. J Urol 2018;200:815-22. [Crossref] [PubMed]
- Sahin S, Bicer M, Eren GA, et al. Acupuncture relieves symptoms in chronic prostatitis/chronic pelvic pain syndrome: a randomized, sham-controlled trial. Prostate Cancer Prostatic Dis 2015;18:249-54. [Crossref] [PubMed]
- Zhou M, Yang M, Chen L, et al. The effectiveness of long-needle acupuncture at acupoints BL30 and BL35 for CP/CPPS: a randomized controlled pilot study. BMC Complement Altern Med 2017;17:263. [Crossref] [PubMed]
- Chen R, Nickel JC. Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome. Urology 2003;61:1156-9; discussion 1159. [Crossref] [PubMed]
- Tugcu V, Tas S, Eren G, et al. Effectiveness of acupuncture in patients with category IIIB chronic pelvic pain syndrome: a report of 97 patients. Pain Med 2010;11:518-23. [Crossref] [PubMed]
- Propert KJ, Litwin MS, Wang Y, et al. Responsiveness of the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI). Qual Life Res 2006;15:299-305. [Crossref] [PubMed]
- Farmer MA, Chanda ML, Parks EL, et al. Brain functional and anatomical changes in chronic prostatitis/chronic pelvic pain syndrome. J Urol 2011;186:117-24. [Crossref] [PubMed]
- Motrich RD, Maccioni M, Riera CM, et al. Autoimmune prostatitis: state of the art. Scand J Immunol 2007;66:217-27. [Crossref] [PubMed]
- Rivero VE, Motrich RD, Maccioni M, et al. Autoimmune etiology in chronic prostatitis syndrome: an advance in the understanding of this pathology. Crit Rev Immunol 2007;27:33-46. [Crossref] [PubMed]
- Lee SW, Liong ML, Yuen KH, et al. Acupuncture and immune function in chronic prostatitis/chronic pelvic pain syndrome: a randomized, controlled study. Complement Ther Med 2014;22:965-9. [Crossref] [PubMed]
- Anothaisintawee T, Attia J, Nickel JC, et al. Management of chronic prostatitis/chronic pelvic pain syndrome: a systematic review and network meta-analysis. JAMA 2011;305:78-86. [Crossref] [PubMed]