Adhering to quality medical care: a case report of upper gastrointestinal bleeding due to self-expandable metal stent placed for benign duodenal obstruction
Introduction
Treatment options for benign pyloric obstruction—a common complication of peptic ulcer disease—include medical, endoscopic and surgical approach. Surgery is associated with a significant risk of postoperative comorbidity; thus, remains suitable for a minority of patients. On the other hand, endoscopic balloon dilation with concurrent use of anti-secretory therapy has been proven a useful alternative particularly in high surgical risk candidates. Self-expandable metal stent (SEMS)—designated originally for the treatment of malignant obstructive lesions—represent a sophisticated therapeutic option (1). To date, several reports of SEMS placement for benign pyloric stenosis have been published; however, data regarding their long term efficacy and safety in particular, remain limited (2-6). Herein, we present the management of a late onset stent induced iatrogenic complication in a patient suffering from peptic ulcer disease consequence, aiming to underline that innovation does not necessarily correlate with quality of care.
Case presentation
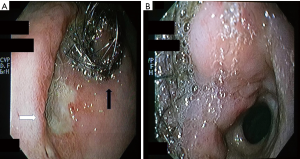
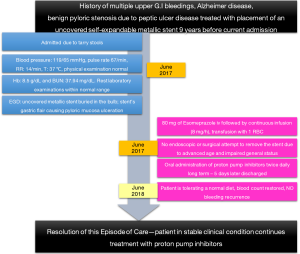
A 100-year-old Caucasian female patient was transferred to our Emergency Department due to tarry stool. Her past medical history involved seventeen upper gastrointestinal (GI) bleeding episodes—no proper investigation during previous admissions has been performed due to patient’s clinical status, Alzheimer disease and benign pyloric stenosis treated with placement of an uncovered self-expandable metallic stent 9 years before. On current admission, the patient was hemodynamically stable and under no medication. Clinical evaluation was unremarkable, while laboratory examinations demonstrated only anemia (Hb: 8.5 g/dL); all other routine biochemical and hematological profiles were within normal ranges. After initial resuscitation, the patient was transferred to the Endoscopy Unit where esophagogastroduodenoscopy revealed the presence of an uncovered SEMS, buried and epithelialized in the duodenal bulb. The distorted gastric flair of the stent caused ulceration of the surrounding pyloric mucosa (Figure 1). At that time, no attempt to remove the stent was performed, while surgical treatment was ruled out due to patient’s advanced age and impaired performance status (Grade 3). Instead, we favored conservative approach and treatment only with proton pump inhibitors twice daily was advocated. Gradually, the patient presented significant clinical improvement and was discharged 5 days post-admission, instructed to continue the same medication. Twelve months later, the patient is tolerating a normal diet, blood count has been fully restored and has not experienced bleeding recurrence, as shown in the case report time line (Figure 2).
Discussion
Although technical and clinical success rates of SEMS for treating benign gastro duodenal obstruction have been well established, their long-term consequences remain to be elucidated. Severe complications i.e., bleeding and perforation are rare and mainly present in the early post-procedural period (4,7). To the best of our knowledge, this is the first case of a late onset complication due to a self-expandable stent placed for benign gastro duodenal obstruction, occurring over than 9 years after the index procedure.
Case series have shown that SEMSs deployment not only results in immediate symptom improvement, but more importantly this effect is sustained on the long term (after 11 months of follow-up) (5). Similarly, partially covered SEMS were found to improve obstructive symptoms for more than 1 year, even after multiple unsuccessful balloon dilatation procedures (8). In another study, patients who had previously failed balloon dilatation reported sustained symptom improvement after SEMS implementation (3). Taken together, these data suggest that SEMS represent an effective alternative with safe and favorable outcome, particularly as salvage treatment after balloon dilatation failure.
Nonetheless, the process is not complication free. Among them, stent occlusion, migration and perforation are the most common (1). Minor post-procedural bleeding can be also seen frequently; however, massive bleeding requiring an intervention, occurs seldom (0.8%) and in most cases in the early post-procedural period (4). Previous reports have concluded that the radial force generated by stenting might be the cause of GI bleeding (7). Although no clear explanation can be provided, we postulate that in our case recurrent bleeding was the result of local mucosal ischemia due to constant stent pressure.
The rationale that led to stent placement in the first place, instead of managing the benign stricture via another efficient method (e.g., balloon dilation) can be hardly addressed, as the patient’s medical record was not available. It is possible that the patient’s neurological deficit prevented performance of other balloon dilation sessions for palliation of the obstruction, since they usually need to be repeated for a durable response to be achieved. In addition, even in expert hands a well-established perforation risk (3–7%) is imminent (1).
This case suggests that one should be cautious with innovative devices, particularly in cases where long term prospective data on their efficacy and safety are lacking. Fancy adjunct tools are attractive and endoscopists are always eager to use them; however, evidence to support their widespread use is not always sufficiently robust. Therefore, established guidelines should govern our everyday clinical practice and guide therapeutic decisions on a case by case basis, taking each time into account all patient-related parameters and potential outcomes. Fortunately, long term proton pump inhibitor treatment resulted in cessation of hemorrhages and improved the patient’s quality of life.
In conclusion, late onset bleeding after SEMS placement is a rare post-procedural complication and endoscopists should be aware of it. Prior to using innovative treatment modalities, they should carefully assess all the unique aspects of each patient’s disease and bear the ultimate goal in mind: to provide the optimal medical care.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Committee ASoP, Fukami N, Anderson MA, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc 2011;74:13-21. [Crossref] [PubMed]
- Choi WJ, Park JJ, Park J, et al. Effects of the temporary placement of a self-expandable metallic stent in benign pyloric stenosis. Gut Liver 2013;7:417-22. [Crossref] [PubMed]
- Dormann AJ, Deppe H, Wigginghaus B. Self-expanding metallic stents for continuous dilatation of benign stenoses in gastrointestinal tract - first results of long-term follow-up in interim stent application in pyloric and colonic obstructions. Z Gastroenterol 2001;39:957-60. [Crossref] [PubMed]
- Saleem A, Bakken J, Baron TH. Early massive bleeding after duodenal self-expandable metal stent placement for palliation of malignant gastric outlet obstruction (with video). Gastrointest Endosc 2011;74:1426-7. [Crossref] [PubMed]
- Heo J, Jung MK. Safety and efficacy of a partially covered self-expandable metal stent in benign pyloric obstruction. World J Gastroenterol 2014;20:16721-5. [Crossref] [PubMed]
- Joo MK, Park JJ, Lee BJ, et al. A case of stenotic change from gastric candidiasis managed with temporary stent insertion. Gut Liver 2011;5:238-41. [Crossref] [PubMed]
- Matsumoto K, Hayashi A, Yashima K, et al. Late complications of self-expandable metallic stent placement for malignant gastric outlet obstruction. Intern Med 2014;53:2773-5. [Crossref] [PubMed]
- Park S, Chun HJ, Keum B, et al. Successful salvage treatment of peptic duodenal stenosis with repeat insertion of self-expanding stent after failed balloon dilation. Endoscopy 2011;43 Suppl 2 UCTN:E187-8.


