Surveillance or resection after chemoradiation in esophageal cancer
Introduction
Esophageal cancer is the sixth leading cause of cancer-related mortality worldwide due to its overall poor prognosis (1). The global age-standardized incidence rate of esophageal squamous cell carcinoma (ESCC) is 1.4–13.6 per 100,000 people (2). Esophageal cancer is estimated to be responsible for 15,690 deaths and 16,940 new cases in the United States in 2016 (3). The majority of patients present with locally advanced or systemic disease and outcomes remain poor despite advances in treatment (4,5). Although esophagectomy has traditionally been the mainstay of curative treatment for esophageal cancer, the role of surgery has been evolving. Fewer and fewer patients are being treated with esophagectomy alone. Endoscopic mucosal resection and ablation have achieved excellent results in patients with very early stage disease such as high grade dysplasia or intramucosal tumors. Esophagectomy as monotherapy remains the treatment of choice only for that small subset of patient with local disease not amenable to endoscopic therapy, but not yet considered locally advanced—multifocal T1a tumors, T1b tumors, and some T2 tumors (6-8).
Trimodality therapy with neoadjuvant chemoradiation (nCRT) followed by surgery has become the standard of care for many patients with locally advanced esophageal cancer. Multiple randomized studies have demonstrated the advantages of nCRT including tumor down staging, enhanced resectability (R0 resection), better local control, and most importantly, improved overall survival (OS). While trimodality therapy has become increasingly common in the treatment of locally advanced esophageal cancer, evidence has also emerged supporting the use of definitive CRT for some patients. Retrospective studies of definitive CRT for esophageal cancer have reported survival rates comparable to those for trimodality therapy (9). Randomized controlled trials, with predominantly squamous cell patients, have not found a survival benefit for the addition of surgery after CRT, calling into question the necessity of surgery (10,11). Based on the available data, there appears to be only a group of patients who actually derive a survival benefit from esophagectomy after CRT, but identifying that group of patients is problematic (12). Thus, for patients who have a good response to CRT, the decision of whether to undergo surveillance or resection is difficult.
Emergence of nCRT
In the first randomized study investigating nCRT for esophageal carcinoma, performed by Walsh et al., trimodality therapy was associated with a longer median survival (16 vs. 11 months, P=0.01) and a higher 3-year survival rate (32% vs. 6%, P=0.01), when compared to surgery alone (13). Since then, additional studies and meta-analyses have demonstrated the superiority of treatment with nCRT plus surgery as compared to surgery alone for locally advanced esophageal cancer (14-17). Over the past 20 years, the use of nCRT has become much more common. As experience with trimodality therapy has increased, there has been greater recognition that some patients have pathologic complete response (pCR) after nCRT with no evidence of residual tumor on final pathology. This appears to be a true reflection of treatment response, rather than a sampling error (18). As opposed to nCRT which rarely leads to pCR, nCRT may lead to pCR in a significant percentage of patients (19).
Importance of pathologic response
Multiple studies have demonstrated the importance of pCR for prognosis. In many studies, the pathologic response to nCRT was the most important factor for OS (20-24). Due to the heterogeneity of patient characteristics and treatment regimens, studies have reported a wide range of pCR rates. In randomized trials of nCRT, pCR rates of 16–43% have been reported (Table 1). In a prospective study, Lee et al. showed that pCR was achieved in 43% [95% confidence interval (CI), 27–59%] of patients who underwent surgery after CRT (24). Samson et al. reported that a pCR rate of 17.2% (30). There is a myriad of factors that likely influence the probability of achieving pCR. Squamous cell histology has generally been thought to be more responsive to radiotherapy than adenocarcinoma (AC). Burmeister et al. reported that the pCR of squamous cell carcinoma (SCC) is higher than AC (27). However, in a review of multiple, heterogeneous studies, Bollschweiler et al. reported that SCC was not consistently associated with improved rates of pCR (31). More recent studies have reported greater response rates in SCC than for AC. In the CROSS trial, patients with squamous histology had more than double the rate of pCR (49%) compared to AC (23%, P=0.008) (16). One study found that patient age, smoking history, and tumor diameter were predictors of pCR (32).
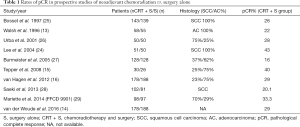
Full table
Definitive CRT
Definitive CRT has long been the standard treatment for unresectable disease and has been an option for patients with poor physical status or patients who refuse esophagectomy (33,34). The JCOG 9906 trial, reported by Kato et al., reported survival rates after definitive CRT for stage II and III esophageal SCC that were similar to trimodality therapy (median survival of 29 months, 3- and 5-year survival rates of 44.7% and 36.8%, respectively) (35). Two European randomized trials of CRT vs. trimodality therapy have also provided evidence to support the use of definitive CRT even for patients who are surgical candidates. Bedenne et al. (FFCD 9102) and Stahl et al. randomized patients to either surgical resection after CRT or definitive CRT. Neither of these studies found a survival benefit for surgery. However, postoperative mortality after esophagectomy was relatively high in both studies and locoregional control was significantly better with surgery in both studies (10,11). These studies were largely performed before more modern staging with positron emission tomography/computed tomography (PET/CT) and endoscopic ultrasound, which probably would have identified additional patients with metastatic disease. Retrospective studies have reported improved survival for treatment that includes surgery, but these studies are obviously limited by selection bias (36). Even if esophagectomy offers some survival benefit, that benefit must be weighed against the potential short-term and long-term harms, including perioperative mortality and morbidity, and adverse effects on long-term quality of life (37).
One important consideration for definitive CRT is the dose of radiation. Evidence from the intergroup (INT) 0123 trial (RTOG 94-05) indicates that the optimal dose for nCRT and definitive CRT are equivalent, and that higher doses beyond 50 Gy of radiation are unwarranted even for definitive CRT (38). In some ways, this eliminates the need to decide on definitive or nCRT prior to therapy. The decision to perform surgery may be made after completion of CRT without compromising the chemotherapy or radiation plan.
Clinical tools to predict pCR after CRT
The recognition that many patients have no viable tumor in the resected specimen has naturally led to the question of whether surgery is beneficial for patients with pCR. There has been increased interest in ways to identify which patients have pCR prior to surgery. At present, imaging modalities have suboptimal accuracy in differentiating residual carcinoma from inflammation or fibrotic change after CRT. PET continues to be integrated into treatment decision-making, as well as the prediction of response and survival after CRT. Arnett et al. demonstrated that the rates of pCR in patients with and without radiographic complete response after preoperative CRT were 42% and 31% (P=0.17), respectively. In addition, no predictive correlation was found between pCR and the change in maximum standardized uptake value (SUV) (P=0.25) (39). Likewise, endoscopic ultrasound has limited accuracy in determining pCR after CRT (40).
Recently, there has been some interest in potentially increasing the rate of pCR by increasing the interval between CRT and surgery. The results of a recent meta-analysis indicate that a longer interval (more than the standard 7–8 weeks) between nCRT and surgery likely does increase the mortality or major complication rate (41). However, the longer interval does not appear to significantly improve pCR rates and may be associated with worse OS. Interpretation of these results should be done with caution, given the retrospective nature of the studies included in the analysis and the significant selection bias.
The role of salvage esophagectomy
Some patients that choose to have surveillance rather than resection after CRT will have local recurrence. Local recurrence rates following definitive CRT have been reported in up to 40–75% of patients (42,43). If the recurrence is only local, the question then becomes whether salvage resection should be attempted. Recent studies have demonstrated that the postoperative morbidity, mortality, and OS of patients after salvage esophagectomy are comparable to matched patients after planned resection in cases of esophageal AC. One study found that both salvage esophagectomy and planned esophagectomy after nCRT showed good 3-year survival results (63% vs. 71%, respectively), with low postoperative morbidity and mortality (44). In addition, Marks et al. found no difference in the OS between salvage resection and planned resection after CRT (48% at 3-year and 32% at 5-year vs. 55% at 3-year and 45% at 5-year, respectively) (45) These studies suggest that patients with esophageal AC who fail definitive CRT and have locoregional recurrence should be considered for salvage esophagectomy at experienced surgical centers (45,46). However, in a meta-analysis study by Markar et al., which closely examined esophageal SCC, salvage esophagectomy was shown to have poor short-term outcomes when compared with planned esophagectomy following nCRT. Salvage esophagectomy was associated with a significantly increased incidence of post-operative mortality (9.50% vs. 4.07%; P<0.001), anastomotic site leakage (23.97% vs. 14.47%; P=0.005), pulmonary complications (29.75% vs. 16.99%; P<0.001), and an increased duration of hospital stay (P<0.001) (47).
Selective surgery
Given the combination of the above data (a lack of survival benefit for the addition of surgery after CRT, the equivalent radiation dose for definitive and nCRT, and emerging studies demonstrating the safety of salvage esophagectomy), a compelling argument can be made for a selective approach to surgery after CRT. For patients with complete clinical response after CRT, close observation could be performed. Salvage esophagectomy could be used for recurrent locoregional disease. On the other hand, patients who have clear residual disease after CRT could be offered esophagectomy within the same time frame as traditional trimodality therapy. This type of treatment strategy was investigated in the RTOG-0246 prospective trial of selective surgery for esophageal cancer (48). Patients were treated with induction chemotherapy followed by CRT. Patients were then recommended surgery based on clinical suspicion of residual disease. Nearly half the patients (20/41) avoided esophagectomy. Overall 5-year survival was 37% for the group as a whole and 53% among those with clinical complete response.
Future directions in esophageal cancer treatment
Improved systemic therapies may improve the efficacy of nonoperative treatment. Trastuzumab has been studied in combination with nCRT for HER2-expressing esophageal cancer (49). Immunotherapy, such as pembrolizumab the anti-PD-1 antibody, is also being investigated in combination with CRT (50). Aside from increasing cures for esophageal cancer, improving technology will allow us to determine with confidence who will truly benefit from surgery. Newer imaging technologies have shown promise in detecting response to treatment in pilot studies. Some researchers have found diffusion weighted magnetic resonance imaging (MRI) to be predictive of pCR (51). There has been an explosion of interest in biomarkers to predict and assess response to CRT. In particular, miRNA profiling has the potential to predict response to therapy and detect cancer in the serum (52,53).
Conclusions
The current treatment of esophageal cancer involves multidisciplinary therapies including esophagectomy, CRT, chemotherapy, and endoscopic resection. However, esophagectomy remains a complex surgical procedure with associated high mortality and morbidity rates and has the potential to adversely impact long-term quality of life (54). Much like other areas of cancer care, the treatment of locally advanced esophageal cancer needs to move towards personalized medicine. Treatment plans should be based on the underlying biology of the tumor as well as the preferences of the patient. Such an individualized treatment strategy should also take into account the surgical risk of the particular patient and potential impact on quality of life. An organ preservation strategy will likely be more common as methods to assess response to CRT improve. However, given the limitations of current diagnostic technology, we contend resection should remain the standard of care after nCRT for AC. On the other hand, surgery should be approached more judiciously in patients with esophageal SCC who have had a complete response to nCRT, and it should only be done at centers with low operative mortality. Given the poor long-term survival in patients with significant residual nodal disease after CRT, caution should also be exercised in performing surgery in this cohort (55).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- Vizcaino AP, Moreno V, Lambert R, et al. Time trends incidence of both major histologic types of esophageal carcinomas in selected countries, 1973-1995. Int J Cancer 2002;99:860-8. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin 2017;67:7-30. [Crossref] [PubMed]
- Pöttgen C, Stuschke M. Radiotherapy versus surgery within multimodality protocols for esophageal cancer--a meta-analysis of the randomized trials. Cancer Treat Rev 2012;38:599-604. [Crossref] [PubMed]
- Courrech Staal EF, Aleman BM, Boot H, et al. Systematic review of the benefits and risks of neoadjuvant chemoradiation for oesophageal cancer. Br J Surg 2010;97:1482-96. [Crossref] [PubMed]
- Mariette C, Piessen G, Triboulet JP. Therapeutic strategies in oesophageal carcinoma: role of surgery and other modalities. Lancet Oncol 2007;8:545-53. [Crossref] [PubMed]
- Pech O, Manner H, Ell C. Endoscopic resection. Gastrointest Endosc Clin N Am 2011;21:81-94. [Crossref] [PubMed]
- Yamamoto H. Technology insight: endoscopic submucosal dissection of gastrointestinal neoplasms. Nat Clin Pract Gastroenterol Hepatol 2007;4:511-20. [Crossref] [PubMed]
- Wakui R, Yamashita H, Okuma K, et al. Esophageal cancer: definitive chemoradiotherapy for elderly patients. Dis Esophagus 2010;23:572-9. [Crossref] [PubMed]
- Bedenne L, Michel P, Bouche O, et al. Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 2007;25:1160-8. [Crossref] [PubMed]
- Stahl M, Stuschke M, Lehmann N, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 2005;23:2310-7. [Crossref] [PubMed]
- Vallböhmer D, Brabender J, Metzger R, et al. Genetics in the pathogenesis of esophageal cancer: possible predictive and prognostic factors. J Gastrointest Surg 2010;14 Suppl 1:S75-80. [Crossref] [PubMed]
- Walsh TN, Noonan N, Hollywood D, et al. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 1996;335:462-7. [Crossref] [PubMed]
- van der Woude SO, Hulshof MC, van Laarhoven HW. CROSS and beyond: a clinical perspective on the results of the randomized ChemoRadiotherapy for Oesophageal cancer followed by Surgery Study. Chin Clin Oncol 2016;5:13. [PubMed]
- Tepper J, Krasna MJ, Niedzwiecki D, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 2008;26:1086-92. [Crossref] [PubMed]
- van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012;366:2074-84. [Crossref] [PubMed]
- Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol 2011;12:681-92. [Crossref] [PubMed]
- Chang EY, Smith CA, Corless CL, et al. Accuracy of pathologic examination in detection of complete response after chemoradiation for esophageal cancer. Am J Surg 2007;193:614-7; discussion 617. [Crossref] [PubMed]
- Rohatgi PR, Swisher SG, Correa AM, et al. Failure patterns correlate with the proportion of residual carcinoma after preoperative chemoradiotherapy for carcinoma of the esophagus. Cancer 2005;104:1349-55. [Crossref] [PubMed]
- Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 1994;73:2680-6. [Crossref] [PubMed]
- Swisher SG, Hofstetter W, Wu TT, et al. Proposed revision of the esophageal cancer staging system to accommodate pathologic response (pP) following preoperative chemoradiation (CRT). Ann Surg 2005;241:810-7; discussion 817-20. [Crossref] [PubMed]
- Berger AC, Farma J, Scott WJ, et al. Complete response to neoadjuvant chemoradiotherapy in esophageal carcinoma is associated with significantly improved survival. J Clin Oncol 2005;23:4330-7. [Crossref] [PubMed]
- Tsou YK, Liang KH, Lin WR, et al. GALNT14 genotype as a response predictor for concurrent chemoradiotherapy in advanced esophageal squamous cell carcinoma. Oncotarget 2017;8:29151-60. [Crossref] [PubMed]
- Lee JL, Park SI, Kim SB, et al. A single institutional phase III trial of preoperative chemotherapy with hyperfractionation radiotherapy plus surgery versus surgery alone for resectable esophageal squamous cell carcinoma. Ann Oncol 2004;15:947-54. [Crossref] [PubMed]
- Bosset JF, Gignoux M, Triboulet JP, et al. Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 1997;337:161-7. [Crossref] [PubMed]
- Urba SG, Orringer MB, Turrisi A, et al. Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 2001;19:305-13. [Crossref] [PubMed]
- Burmeister BH, Smithers BM, Gebski V, et al. Surgery alone versus chemoradiotherapy followed by surgery for resectable cancer of the oesophagus: a randomised controlled phase III trial. Lancet Oncol 2005;6:659-68. [Crossref] [PubMed]
- Saeki H, Morita M, Nakashima Y, et al. Neoadjuvant chemoradiotherapy for clinical stage II-III esophageal squamous cell carcinoma. Anticancer Res 2011;31:3073-7. [PubMed]
- Mariette C, Dahan L, Mornex F, et al. Surgery alone versus chemoradiotherapy followed by surgery for stage I and II esophageal cancer: final analysis of randomized controlled phase III trial FFCD 9901. J Clin Oncol 2014;32:2416-22. [Crossref] [PubMed]
- Samson P, Robinson C, Bradley J, et al. Neoadjuvant Chemotherapy versus Chemoradiation Prior to Esophagectomy: Impact on Rate of Complete Pathologic Response and Survival in Esophageal Cancer Patients. J Thorac Oncol 2016;11:2227-37. [Crossref] [PubMed]
- Bollschweiler E, Holscher AH, Metzger R. Histologic tumor type and the rate of complete response after neoadjuvant therapy for esophageal cancer. Future Oncol 2010;6:25-35. [Crossref] [PubMed]
- Saeki H, Nakashima Y, Zaitsu Y, et al. Current status of and perspectives regarding neoadjuvant chemoradiotherapy for locally advanced esophageal squamous cell carcinoma. Surg Today 2016;46:261-7. [Crossref] [PubMed]
- Crosby TD, Brewster AE, Borley A, et al. Definitive chemoradiation in patients with inoperable oesophageal carcinoma. Br J Cancer 2004;90:70-5. [Crossref] [PubMed]
- Kaneko K, Ito H, Konishi K, et al. Definitive chemoradiotherapy for patients with malignant stricture due to T3 or T4 squamous cell carcinoma of the oesophagus. Br J Cancer 2003;88:18-24. [Crossref] [PubMed]
- Kato K, Muro K, Minashi K, et al. Phase II study of chemoradiotherapy with 5-fluorouracil and cisplatin for Stage II-III esophageal squamous cell carcinoma: JCOG trial (JCOG 9906). Int J Radiat Oncol Biol Phys 2011;81:684-90. [Crossref] [PubMed]
- Chen MF, Chen PT, Lu MS, et al. Survival benefit of surgery to patients with esophageal squamous cell carcinoma. Sci Rep 2017;7:46139. [Crossref] [PubMed]
- Scarpa M, Saadeh LM, Fasolo A, et al. Health-related quality of life in patients with oesophageal cancer: analysis at different steps of the treatment pathway. J Gastrointest Surg 2013;17:421-33. [Crossref] [PubMed]
- Minsky BD, Pajak TF, Ginsberg RJ, et al. INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 2002;20:1167-74. [Crossref] [PubMed]
- Arnett AL, Merrell KW, Macintosh EM, et al. Utility of 18F-FDG PET for Predicting Histopathologic Response in Esophageal Carcinoma following Chemoradiation. J Thorac Oncol 2017;12:121-8. [Crossref] [PubMed]
- Zuccaro G Jr, Rice TW, Goldblum J, et al. Endoscopic ultrasound cannot determine suitability for esophagectomy after aggressive chemoradiotherapy for esophageal cancer. Am J Gastroenterol 1999;94:906-12. [Crossref] [PubMed]
- Lin G, Han SY, Xu YP, et al. Increasing the interval between neoadjuvant chemoradiotherapy and surgery in esophageal cancer: a meta-analysis of published studies. Dis Esophagus 2016;29:1107-14. [Crossref] [PubMed]
- Cooper JS, Guo MD, Herskovic A, et al. Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group. JAMA 1999;281:1623-7. [Crossref] [PubMed]
- Kranzfelder M, Schuster T, Geinitz H, et al. Meta-analysis of neoadjuvant treatment modalities and definitive non-surgical therapy for oesophageal squamous cell cancer. Br J Surg 2011;98:768-83. [Crossref] [PubMed]
- Farinella E, Safar A, Nasser HA, et al. Salvage esophagectomy after failure of definitive radiochemotherapy for esophageal cancer. J Surg Oncol 2016;114:833-7. [Crossref] [PubMed]
- Marks JL, Hofstetter W, Correa AM, et al. Salvage esophagectomy after failed definitive chemoradiation for esophageal adenocarcinoma. Ann Thorac Surg 2012;94:1126-32; discussion 1132-3. [Crossref] [PubMed]
- Smithers BM, Cullinan M, Thomas JM, et al. Outcomes from salvage esophagectomy post definitive chemoradiotherapy compared with resection following preoperative neoadjuvant chemoradiotherapy. Dis Esophagus 2007;20:471-7. [Crossref] [PubMed]
- Markar SR, Karthikesalingam A, Penna M, et al. Assessment of short-term clinical outcomes following salvage esophagectomy for the treatment of esophageal malignancy: systematic review and pooled analysis. Ann Surg Oncol 2014;21:922-31. [Crossref] [PubMed]
- Swisher SG, Moughan J, Komaki RU, et al. Final Results of NRG Oncology RTOG 0246: An Organ-Preserving Selective Resection Strategy in Esophageal Cancer Patients Treated with Definitive Chemoradiation. J Thorac Oncol 2017;12:368-74. [Crossref] [PubMed]
- Kataoka K, Tokunaga M, Mizusawa J, et al. A randomized Phase II trial of systemic chemotherapy with and without trastuzumab followed by surgery in HER2-positive advanced gastric or esophagogastric junction adenocarcinoma with extensive lymph node metastasis: Japan Clinical Oncology Group study JCOG1301 (Trigger Study). Jpn J Clin Oncol 2015;45:1082-6. [Crossref] [PubMed]
- Iams WT, Villaflor VM. Neoadjuvant Treatment for Locally Invasive Esophageal Cancer. World J Surg 2017;41:1719-25. [Crossref] [PubMed]
- van Rossum PS, van Lier AL, van Vulpen M, et al. Diffusion-weighted magnetic resonance imaging for the prediction of pathologic response to neoadjuvant chemoradiotherapy in esophageal cancer. Radiother Oncol 2015;115:163-70. [Crossref] [PubMed]
- Skinner HD, Lee JH, Bhutani MS, et al. A validated miRNA profile predicts response to therapy in esophageal adenocarcinoma. Cancer 2014;120:3635-41. [Crossref] [PubMed]
- Zhang K, Wu X, Wang J, et al. Circulating miRNA profile in esophageal adenocarcinoma. Am J Cancer Res 2016;6:2713-21. [PubMed]
- Sanghera SS, Nurkin SJ, Demmy TL. Quality of life after an esophagectomy. Surg Clin North Am 2012;92:1315-35. [Crossref] [PubMed]
- Kim JY, Nelson RA, Kim J, et al. How well does pathologic stage predict survival for esophageal adenocarcinoma after neoadjuvant therapy? J Thorac Dis 2015;7:734-9. [PubMed]


