Severe sepsis and cardiac arrhythmias
Introduction
The diagnosis of systemic inflammatory response to infection has been found to highly correlate with the presentation of cardiac arrhythmias in critically ill patients (1-4). As previous studies have shown, patients with moderate to severe sepsis have a greater likelihood of exhibiting various cardiac arrhythmias (5,6). The majority of these clinical studies were focused on the diagnosis, management, predictors and outcomes of new onset AF in the general intensive care patient population (7). However, studies performed to provide a comprehensive assessment of both atrial and ventricular arrhythmias in severe sepsis patients are lacking.
Age, gender, and the progression of sepsis are known risk factors for the development of cardiac arrhythmias (4,6). Patients with severe sepsis are more likely to suffer from new-onset AF, ischemic stroke, or mortality (4). Current treatment for atrial and ventricular arrhythmias in severe sepsis patients consists primarily of the utilization of calcium channel and beta-blockers (8). Although guidelines have been developed to manage severe sepsis in order to reduce morbidity and mortality in critical care patients, these have yet to significantly affect outcomes in patients who develop cardiac arrhythmias (8,9).
While antibiotic therapies treat the cause of sepsis, there is a lack of preventative measures for arresting the development of cardiac arrhythmias in sepsis patients (10). This study focuses on the outcomes of this patient population to identify whether there is sufficient evidence to necessitate preventative guidelines for atrial and ventricular arrhythmias in patients with diagnosed severe sepsis.
The aim of this study is to evaluate the risk of atrial and ventricular arrhythmias in patients with severe sepsis, identify predictors and assess the impact of arrhythmias on outcome in this clinical setting.
Methods
Data source and objectives
National Inpatient Sample (NIS) database from 2012 was used for obtaining data. The NIS is sponsored by the Agency for Healthcare Research and Quality as a part of Healthcare Cost and Utilization Project (HCUP) and is the largest publicly available all-payer database in the United States. The database contains discharge-level data from about 1,000 hospitals designed to approximate a 20% stratified sample of all community hospitals in the United States. Currently 46 U.S. states contribute data to NIS. The database contains more than 100 clinical and non-clinical elements for each hospital stay, including primary and secondary diagnoses and procedures, admission and discharge status, patient demographics, hospital characteristics, payer source, comorbidity measures, length of stay (LOS), and discharge status (15 from AMIs paper). Discharge weights are provided in each patient discharge record and are then used to obtain national estimates. As the data are based on an administrative dataset and are de-identified, no informed consent was needed. Our objectives were to identify prevalence and independent risk factors of cardiac arrhythmias in patients diagnosed with severe sepsis.
Study population and outcomes
We used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (provided in supplementary appendix) to identify all patients over the age of 18 years with a discharge diagnosis of severe sepsis, atrial fibrillation (A Fib), atrial flutter (AFL), ventricular fibrillation (VF) arrest and non-ventricular fibrillation (non-VF) arrest. The sepsis group (n=1,756,965) was compared to those without sepsis (n=28,955,559). Our primary outcome of interest was to assess prevalence of atrial and ventricular arrhythmias. Secondary outcomes of interest were mortality and LOS.
Statistical analysis
We used baseline patient characteristics including demographics (age, gender, and race), primary expected payer, median household income for patient’s ZIP code, Elixhauser co-morbidities as defined by the Agency for Healthcare Research and Quality, and other clinically relevant co-morbidities (dyslipidemia, hypertension, congestive heart failure (CHF), chronic lung disease, diabetes mellitus (DM), liver disorders, neurological disorders, obesity, renal failure, peripheral vascular disease (PVD), valvular heart disease and mechanical ventilation) (11,12). A list of ICD-9-CM and Clinical Classifications Software codes used to identify co-morbidities is provided in Table S1.

Full table
Data were analyzed using SAS statistical software package version 9.4, (SAS Institute Inc., Cary, North Carolina, USA). Continuous variables were summarized using means with 95% confidence intervals (CI). Similarly, categorical variables were summarized with the use of proportions and percentages. The Chi-square test was used to compare categorical variables and the t-test for continuous variables. Appropriate Survey Discharge Weights were applied for NIS data and Survey Procedure Commands were applied for the analysis. A 2-sided P value of <0.05 was used to assess for statistical significance. Multivariate logistic regression was used to compare outcomes between the two groups. The regression model adjusted for demographics, primary expected payer, median household income and all Elixhauser co-morbidities.
Results
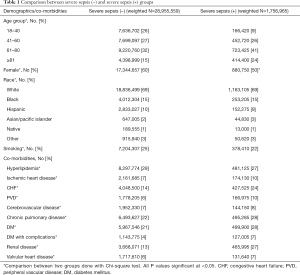
Baseline characteristics of patients diagnosed with severe sepsis during 2012 are described in Table 1. In general, patients with severe sepsis were more likely to be older in age, to have CHF, PVD, chronic obstructive pulmonary disease (COPD), DM and renal disease.
Full table
Predictors and outcomes of arrhythmias in patients with severe sepsis
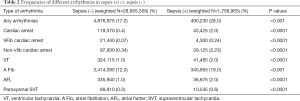
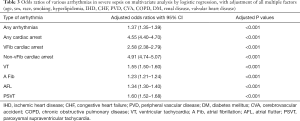
Severe sepsis was associated with a higher prevalence of atrial and ventricular arrhythmias (28% vs. 17%, P<0.001, Table 2). A Fib was the most prevalent arrhythmia overall, although it was more prevalent in the sepsis group (12% vs. 19%, P<0.001). Severe sepsis increased the risk of arrhythmias across the board (Table 3). On multivariate analysis, after adjusting for potential confounders, severe sepsis was associated with higher risk of A Fib (OR, 1.23; 95% CI, 1.21–1.24), AFL (OR, 1.34; 95% CI, 1.30–1.40) and paroxysmal supraventricular tachycardia (SVT) (OR, 1.60; 95% CI, 1.52–1.68). Among ventricular arrhythmias, the risk was higher for VF (OR, 2.58; 95% CI, 2.38–2.79) compared to ventricular tachycardia (VT) (OR, 1.55; 95% CI, 1.50–1.60). Risk of non-VF arrest was nearly twice as high as VF arrest (OR, 4.91; 95% CI, 4.74–5.07).
Full table
Full table
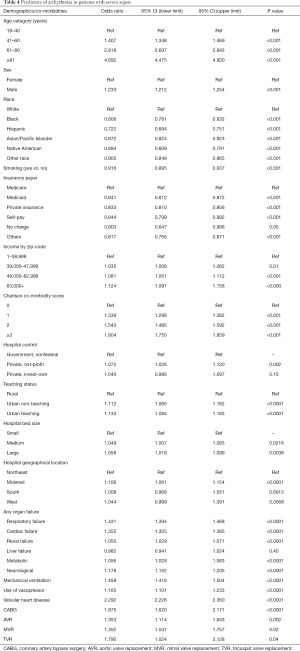
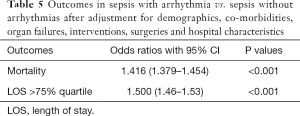
Advanced age, male sex, ischemic heart disease, DM, CHF, valvular heart disease, respiratory failure, mechanical ventilation and use of vasopressors were independently associated with cardiac arrhythmias (Table 4). Patients with severe sepsis and a co-diagnosis of any cardiac arrhythmia was associated with a higher in-hospital mortality (OR, 1.416; 95% CI, 1.379–1.454) and LOS >75% quartile (OR, 1.500; 95% CI, 1.46–1.53, Table 5).
Full table
Full table
Discussion
Several reports and studies have demonstrated an association between sepsis and various cardiac arrhythmias (1-5,13). The vast majority of studies assessing risk and outcomes of arrhythmias in sepsis have focused on supra ventricular arrhythmias, A Fib in particular (14-17). To our knowledge, the present study is the largest to use discharge diagnoses from the NIS database to validate prevalence, trends, predictors and outcomes of different arrhythmias in the septic population. The majority of studies in the literature have analyzed data from single and multi-center cohorts. Our study measures prevalence, risk factors and outcomes through discharge diagnoses of NIS database; therefore employing data sourced from multiple centers nationwide, and thus has a fair degree of generalizability.
Among more than thirty million hospital discharges analyzed, around 6% had a discharge diagnosis of severe sepsis. There was an increased risk of atrial and ventricular arrhythmias, as well as a fivefold higher incidence of cardiac arrest in patients with severe sepsis. Even though AF was the most prevalent arrhythmia in both septic and non-septic populations, odds of developing paroxysmal SVT were highest followed by AFL and AF in the severe sepsis group. Among ventricular arrhythmias VF was significantly more frequent than VT. Furthermore, a co- diagnosis of cardiac arrhythmia in patients with severe sepsis was associated with a higher mortality and longer length of hospital stay. As expected, advanced age, male sex, ischemic heart disease, DM, CHF, valvular heart disease, respiratory failure, mechanical ventilation, high comorbidity burden measured using CCI and use of vasopressors were associated with cardiac arrhythmias.
Association of cardiac arrhythmias with sepsis has been reported since the 1970s (18). Although A fib is the most frequently reported arrhythmia (14,15,17,19), large epidemiologic studies designed to assess incidence of different arrhythmias in the septic population are lacking. Consistent with our findings, previous studies have found advanced age, male gender and comorbidities such as heart failure, HTN and valvular heart disease to predict new onset A Fib in critically ill patients (5,14,16,20,21). Similarly new onset A fib has consistently been associated with a higher mortality in septic patients (2,4,14). Compared to patients with preexisting A Fib, new onset A Fib has been associated with higher mortality rates (4). Furthermore, both atrial and ventricular arrhythmias have been associated with a higher incidence of neurologic compromise (22) and prolonged need for vasopressors (23).
The mechanisms behind higher incidence of cardiac arrhythmias in severe sepsis have not been completely elucidated but could involve several pathophysiologic pathways impacting the arrhythmogenic substrate, the trigger factors and the modulation factors.
Imbalance in autonomic tone has been suggested as a potential pro-arrhythmic factor in severe sepsis (24,25), which may induce arrhythmias by altering triggered activity (26). In addition to high catecholamine levels, systemic inflammatory component of severe sepsis may further contribute to the pro-arrhythmic milieu. This hypothesis is supported by a strong correlation between systemic inflammatory markers such as elevated C-reactive protein, IL-6 and TNF-α, and new onset A Fib (27). Furthermore, abnormalities in calcium handling have been demonstrated in animal models in response to endotoxin application (28-31). Increased intracellular calcium is associated with shortening of atrial refractory period and elicited triggered activity by the way of delayed afterdepolarizations therefore putting patients at high risk of cardiac arrhythmias (26,32).
Reemphasized by the present study, even though arrhythmias may be an early sign of sepsis (1) and are associated with adverse outcomes, there is lack of data regarding evidence based treatment strategies. Moreover, present data mainly focuses on treatment and prevention of A fib (3). Although beta blockers and calcium channel blockers have proven successful in management of atrial arrhythmias (8), their use outside of atrial arrhythmias has not been tested and it may be a challenge to use them in setting of hypotension, which is a frequent occurrence in severe sepsis. Antibiotics and hemodynamic support, which includes volume resuscitation and use of vasopressors in severe cases are the mainstay therapy (9). Current sepsis treatment guidelines recommend norepinephrine, dopamine and dobutamine as first line vasopressor agents, they may not be the ideal choice in the setting of active or recurrent arrhythmias (9) in view of their pro-arrhythmic properties (33). Despite lack of data to support this, in view of their virtual lack of affinity for beta receptors it appears intuitive to use vasopressors such as phenylephrine and vasopressin in the setting of recurrent or active arrhythmias in septic patients requiring vasopressor support. By the same token, electrolytes should be closely monitored and replaced as needed, as potassium and magnesium in particular are established risk factors for cardiac arrhythmias irrespective of the clinical setting (33).
Limitations
The main limitation of the study is that it is a retrospective analysis of an administrative hospital-originated database. Large population based studies utilizing databases and registries are prone to bias inherent to such studies (34), as the investigators are highly dependent on the accuracy and completeness of initial data entry by non-medical professionals. Furthermore, the database did not allow us access to laboratory values, imaging studies, medications and certain clinical variables, which would have allowed us to assess severity of critical illness and further stratify the arrhythmia risk. Multivariate analysis was performed to account for baseline differences; however, the impact of undocumented confounding factors could not be completely dissected in this retrospective analysis. Despite these limitations, the study, one of the largest assessing the relationship between cardiac arrhythmias and severe sepsis, identifies incidence of and outcomes of cardiac arrhythmias in patients with severe sepsis.
Conclusions
Patients with severe sepsis are at high risk of atrial and ventricular arrhythmias. Presence of arrhythmias in this critically ill population is associated with adverse outcomes. Even though their presence could be a marker of increasing severity of the pre-existing illness, arrhythmias may independently increase mortality in septic patients. Every effort should be made to prevent arrhythmias in this clinical setting. Further studies identifying predictors and mechanisms of arrhythmias in severe sepsis will help with defining preventive and treatment strategies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Since the study was based on de identified publicly available database and IRB exempt, IRB review was not required hence not sought.
References
- Goodman S, Weiss Y, Weissman C. Update on cardiac arrhythmias in the ICU. Curr Opin Crit Care 2008;14:549-54. [Crossref] [PubMed]
- Christian SA, Schorr C, Ferchau L, et al. Clinical characteristics and outcomes of septic patients with new-onset atrial fibrillation. J Crit Care 2008;23:532-6. [Crossref] [PubMed]
- Meierhenrich R, Steinhilber E, Eggermann C, et al. Incidence and prognostic impact of new-onset atrial fibrillation in patients with septic shock: a prospective observational study. Crit Care 2010;14:R108. [Crossref] [PubMed]
- Walkey AJ, Wiener RS, Ghobrial JM, et al. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA 2011;306:2248-54. [Crossref] [PubMed]
- Aderka D, Sclarovsky S, Lewin RF, et al. Life-threatening ventricular arrhythmias in septicemia. Isr J Med Sci 1984;20:535-7. [PubMed]
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5. [Crossref] [PubMed]
- Schwartz A, Brotfain E, Koyfman L, et al. Cardiac Arrhythmias in a Septic ICU Population: A Review. J Crit Care Med 2015;1:140-6.
- Walkey AJ, Evans SR, Winter MR, et al. Practice Patterns and Outcomes of Treatments for Atrial Fibrillation During Sepsis: A Propensity-Matched Cohort Study. Chest 2016;149:74-83. [Crossref] [PubMed]
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med 2017;43:304-77. [Crossref] [PubMed]
- Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care 2009;15:392-7. [Crossref] [PubMed]
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8-27. [Crossref] [PubMed]
- Healthcare Cost and Utilization Project (HCUP). Comorbidity Software. Available online: https://www.ahrq.gov/research/data/hcup/index.html
- Reinelt P, Karth GD, Geppert A, et al. Incidence and type of cardiac arrhythmias in critically ill patients: a single center experience in a medical-cardiological ICU. Intensive Care Med 2001;27:1466-73. [Crossref] [PubMed]
- Salman S, Bajwa A, Gajic O, et al. Paroxysmal atrial fibrillation in critically ill patients with sepsis. J Intensive Care Med 2008;23:178-83. [Crossref] [PubMed]
- Goodman S, Shirov T, Weissman C. Supraventricular arrhythmias in intensive care unit patients: short and long-term consequences. Anesth Analg 2007;104:880-6. [Crossref] [PubMed]
- Seguin P, Signouret T, Laviolle B, et al. Incidence and risk factors of atrial fibrillation in a surgical intensive care unit. Crit Care Med 2004;32:722-6. [Crossref] [PubMed]
- Makrygiannis SS, Margariti A, Rizikou D, et al. Incidence and predictors of new-onset atrial fibrillation in noncardiac intensive care unit patients. J Crit Care 2014;29:697.e1-5. [Crossref] [PubMed]
- Kirkpatrick JR, Heilbrunn A, Sankaran S. Cardiac arrhythmias: an early sign of sepsis. Am Surg 1973;39:380-2. [PubMed]
- Bender JS. Supraventricular tachyarrhythmias in the surgical intensive care unit: an under-recognized event. Am Surg 1996;62:73-5. [PubMed]
- Brathwaite D, Weissman C. The new onset of atrial arrhythmias following major noncardiothoracic surgery is associated with increased mortality. Chest 1998;114:462-8. [Crossref] [PubMed]
- Knotzer H, Mayr A, Ulmer H, et al. Tachyarrhythmias in a surgical intensive care unit: a case-controlled epidemiologic study. Intensive Care Med 2000;26:908-14. [Crossref] [PubMed]
- Annane D, Sebille V, Duboc D, et al. Incidence and prognosis of sustained arrhythmias in critically ill patients. Am J Respir Crit Care Med 2008;178:20-5. [Crossref] [PubMed]
- Seemann A, Boissier F, Razazi K, et al. New-onset supraventricular arrhythmia during septic shock: prevalence, risk factors and prognosis. Ann Intensive Care 2015;5:27. [Crossref] [PubMed]
- Muller-Werdan U, Buerke M, Ebelt H, et al. Septic cardiomyopathy - A not yet discovered cardiomyopathy? Exp Clin Cardiol 2006;11:226-36. [PubMed]
- Werdan K, Schmidt H, Ebelt H, et al. Impaired regulation of cardiac function in sepsis, SIRS, and MODS. Can J Physiol Pharmacol 2009;87:266-74. [Crossref] [PubMed]
- Aldhoon B, Melenovsky V, Peichl P, et al. New insights into mechanisms of atrial fibrillation. Physiol Res 2010;59:1-12. [PubMed]
- Engelmann MD, Svendsen JH. Inflammation in the genesis and perpetuation of atrial fibrillation. Eur Heart J 2005;26:2083-92. [Crossref] [PubMed]
- Sulakhe PV, Sandirasegarane L, Davis JP, et al. Alterations in inotropy, nitric oxide and cyclic GMP synthesis, protein phosphorylation and ADP-ribosylation in the endotoxin-treated rat myocardium and cardiomyocytes. Mol Cell Biochem 1996;163-4:305-18. [Crossref] [PubMed]
- Hung J, Lew WY. Cellular mechanisms of endotoxin-induced myocardial depression in rabbits. Circ Res 1993;73:125-34. [Crossref] [PubMed]
- Wu SN, Lue SI, Yang SL, et al. Electrophysiologic properties of isolated adult cardiomyocytes from septic rats. Circ Shock 1993;41:239-47. [PubMed]
- Abi-Gerges N, Tavernier B, Mebazaa A, et al. Sequential changes in autonomic regulation of cardiac myocytes after in vivo endotoxin injection in rat. Am J Respir Crit Care Med 1999;160:1196-204. [Crossref] [PubMed]
- Maesen B, Nijs J, Maessen J, et al. Post-operative atrial fibrillation: a maze of mechanisms. Europace 2012;14:159-74. [Crossref] [PubMed]
- Overgaard CB, Dzavik V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation 2008;118:1047-56. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D. Understanding the statistics and limitations of large database analyses. Spine (Phila Pa 1976) 2014;39:1311-2. [Crossref] [PubMed]


