Stress-induced thrombus: prevalence of thromboembolic events and the role of anticoagulation in Takotsubo cardiomyopathy
Introduction
Takotsubo cardiomyopathy (TCM) or stress-induced cardiomyopathy was first described by Sato et al. in 1990 and accounts for 1.7% to 2.2% of all suspected cases of acute coronary syndrome (ACS) (1-5). It is predominantly associated with reversible apical ballooning during systole causing a reduction in ejection fraction. Initial presentation can easily mimic ACS with symptoms that include chest pain and shortness of breath.
Overall, TCM is felt to be a benign process, with a similar in hospital mortality of patients with ACS (6). However, it is associated with several significant complications such as heart failure, arrhythmias, left ventricular (LV) outflow obstruction, thromboembolic events and rarely cardiac rupture.
The aim of our study was to determine the prevalence of thromboembolic events and LV thrombus in patients with TCM.
Methods
We performed a comprehensive literature search to identify studies that reported prevalence of LV thrombus in patients diagnosed with TCM. We performed our search through Scopus, PubMed and using the search terms “thrombus”, “takotsubo”, “embolus”. Additional manual search of the bibliographies of selected studies was performed. We included studies that reported the rate of thromboembolic events as well as LV thrombus. Data on patient’s age, gender, presence of LV thrombus, and occurrence of a thromboembolic event were collected. Two authors screened, reviewed and excluded irrelevant studies. Single case reports were also excluded.
Data analysis was performed using descriptive statistics such as mean and standard deviations (SD), frequencies and percentage frequency distributions using SPSS software package, version 23 (SPSS Inc., Chicago, Illinois, USA).
Results
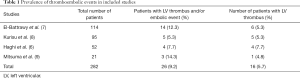
In our literature search, we identified four studies, which resulted in a total of 282 patients. Of the selected 282, 26 (9.2%) patients (mean age ± SD =70.5±11.7 years) were found to have a thromboembolic event. The percent of thromboembolic events per study ranged from 5.3% to 14.3% (Table 1). All patients with a thromboembolic event were females with the exception of one male. In 16 patients a confirmed LV thrombus was identified by echocardiogram, the remaining had no evidence of LV thrombus. The overall prevalence of LV thrombus was found to be 5.7%, with a range of 4.8% to 7.7% among the four studies (Table 1). The most common site of embolization was found to be in the cerebrovascular system. Acute cerebrovascular accident was diagnosed in 6 (23.1%) of the 26 patients.
Full table
Discussion
TCM was first described over 25 years ago and has since then been labeled as a relatively benign pathology. There are several complications associated with TCM. Of which, thrombus formation complicating TCM was first described in the literature in 2003, and has been associated with a higher long-term mortality rate (7,10). Andò et al. (11) reported the first direct visualization of a systemic cardiogenic embolism in a patient with Takotsubo in 2009. Lately, there has been a rising interest in thromboembolic events in Takotsubo, but the true prevalence of thrombus formation and its clinical significance in these patients still remains unknown.
In our review of the literature, the prevalence of thromboembolic events in patients with TCM was found to be 9.2%. This is significantly higher then what is reported in the International Takotsubo Registry, 1.3% (6). It is important to point out that the International Takotsubo Registry identified patients with a follow-up diagnosis of stroke and/or transient ischemic attack. This might lead to an underestimation of the true prevalence of thromboembolic events in these patients.
The prevention and management of thrombus formation complicating TCM also remains undetermined. In a recent literature review by Herath et al., the majority of thrombi were detected during the first 2 weeks (12). In addition of the 50 patients included in their study, most were started on heparin and warfarin with resolution of the thrombus within 2 weeks. Thus, highlighting the importance of follow-up echocardiography in patients diagnosed with TCM.
Should we anticoagulate?
Little is known about the role of prophylactic anticoagulation in patients diagnosed with TCM. Several retrospective studies documented in the literature recommend the use of anticoagulation until resolution of systolic dysfunction on follow-up echocardiogram. To help determine the appropriateness of anticoagulation in these patients, we contrasted our results to the adjusted stroke risk in patients with atrial fibrillation using the CHA2DS2-VASc score. When compared to the CHA2DS2-VASc scoring system, an event rate of 9.2% is equivalent to a score of at least 5. In patients with atrial fibrillation, we routinely anticoagulate with a CHA2DS2-VASc score >2 if there are no contraindications in order to reduce the risk of thromboembolic events (13). Furthermore, in the 2013 STEMI guidelines, there is a IIb recommendation to prophylactically anticoagulate patients with a large anterior wall myocardial infraction (14). The rate of LV thrombus in patients with large anterior myocardial infarction has been reported to be between 5.4% and 7.1% percent. So, applying this approach, it might be reasonable to consider prophylactic anticoagulation in patients with TCM until the myocardium has recovered.
It is important to point out that TCM secondary to catecholamine surges can also be seen after neurologic injuries, such as acute intracranial bleeding (15). In this specific patient population, follow-up echocardiography is particularly important and caution should always be taken when considering anticoagulation.
Conclusions
In our literature review, we found the prevalence of thromboembolic events in patients diagnosed with TCM to be 9.2%, which is significantly higher than what is currently reported in the International Takotsubo Registry, 1.3% (16). We conclude that this feared complication is underappreciated and thus emphasize the importance of follow-up echocardiography in these patients. Prophylactic anticoagulation might be a sensible strategy to prevent thromboembolic events in patients with TCM. Further studies will be needed in order to help select patients with TCM who are at high risk for thromboembolic events.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Dote K, Sato H, Tateishi H, et al. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol 1991;21:203-14. [PubMed]
- Bybee KA, Prasad A, Barsness GW, et al. Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am J Cardiol 2004;94:343-6. [Crossref] [PubMed]
- Ito K, Sugihara H, Katoh S, et al. Assessment of Takotsubo (ampulla) cardiomyopathy using 99mTc-tetrofosmin myocardial SPECT--comparison with acute coronary syndrome. Ann Nucl Med 2003;17:115-22. [Crossref] [PubMed]
- Akashi YJ, Nakazawa K, Sakakibara M, et al. 123I-MIBG myocardial scintigraphy in patients with "takotsubo" cardiomyopathy. J Nucl Med 2004;45:1121-7. [PubMed]
- Matsuoka K, Okubo S, Fujii E, et al. Evaluation of the arrhythmogenecity of stress-induced "Takotsubo cardiomyopathy" from the time course of the 12-lead surface electrocardiogram. Am J Cardiol 2003;92:230-3. [Crossref] [PubMed]
- Haghi D, Papavassiliu T, Heggemann F, et al. Incidence and clinical significance of left ventricular thrombus in tako-tsubo cardiomyopathy assessed with echocardiography. QJM 2008;101:381-6. [Crossref] [PubMed]
- El-Battrawy I, Behnes M, Hillenbrand D, et al. Prevalence, Clinical Characteristics, and Predictors of Patients with Thromboembolic Events in Takotsubo Cardiomyopathy. Clin Med Insights Cardiol 2016;10:117-22. [Crossref] [PubMed]
- Kurisu S, Inoue I, Kawagoe T, et al. Incidence and treatment of left ventricular apical thrombosis in Tako-tsubo cardiomyopathy. Int J Cardiol 2011;146:e58-60. [Crossref] [PubMed]
- Mitsuma W, Kodama M, Ito M, et al. Thromboembolism in Takotsubo cardiomyopathy. Int J Cardiol 2010;139:98-100. [Crossref] [PubMed]
- Kurisu S, Inoue I, Kawagoe T, et al. Left ventricular apical thrombus formation in a patient with suspected tako-tsubo-like left ventricular dysfunction. Circ J 2003;67:556-8. [Crossref] [PubMed]
- Andò G, Saporito F, Trio O, et al. Systemic embolism in takotsubo syndrome. Int J Cardiol 2009;134:e42-3. [Crossref] [PubMed]
- Herath HMMTB, Pahalagamage SP, Lindsay LC, et al. Takotsubo cardiomyopathy complicated with apical thrombus formation on first day of the illness: a case report and literature review. BMC Cardiovasc Disord 2017;17:176. [Crossref] [PubMed]
- Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010;137:263-72. [Crossref] [PubMed]
- American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions, O'Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78-140. [Crossref] [PubMed]
- Trio O, de Gregorio C, Andò G. Myocardial dysfunction after subarachnoid haemorrhage and tako-tsubo cardiomyopathy: a differential diagnosis? Ther Adv Cardiovasc Dis 2010;4:105-7. [Crossref] [PubMed]
- Templin C, Ghadri JR, Diekmann J, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 2015;373:929-38. [Crossref] [PubMed]


