Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction
Atrial fibrillation (AF) is the commonest cardiac arrhythmia and is an independent risk factor for stroke and mortality. Oral anticoagulation is the cornerstone of management for primary and secondary stroke prophylaxis in patients with AF and known additional risk factors (1). Whilst oral vitamin K antagonists (VKA) such as warfarin were the mainstay of treatment for decades, they have been superseded by the newer non-vitamin K antagonist oral anticoagulants (NOACs), which offer relative efficacy, safety and convenience compared to VKAs (2,3). The NOACs include direct thrombin inhibitor, dabigatran and direct factor Xa inhibitors such as rivaroxaban, apixaban and edoxaban.
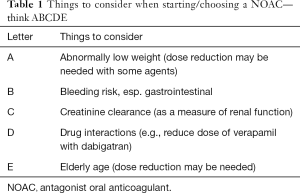
Compared with warfarin, NOACs are generally more convenient to use and are usually given in fixed doses with no routine coagulation monitoring. However, NOACs are prescribed based on strict criteria considering age, weight (in the setting of apixaban), co-morbidities and renal function. When prescribing a NOAC, clinical factors that should be considered are shown in Table 1 (4). Of note, all NOACs are cleared through the renal system to varying degrees (5). Thus, there is a real and understandable risk of under- or over dosing of NOACs in the setting of renal dysfunction which can translate clinically to increased risk of stroke/systemic embolism and/or bleeding.
Full table
Whilst conducting a clinical trial in assessing the direct effects of under- or over dosing of NOACs in real world population is not a viable option for ethical reasons, retrospective analysis of observational “real world” datasets may offer some options.
In a recent issue of JACC, Yao et al. (6) analysed a large U.S. administrative database of 14,865 patients with AF initiating NOACs and examined use of a standard dose in AF patients with a renal indication for dose reduction (i.e., potential overdosing) and the use of a reduced dose when the renal indication is not present (i.e., potential underdosing). Of 1,473 patients with a renal indication for dose reduction, 43.0% were potentially overdosed, which led to more major bleeding (hazard ratio: 2.19; 95% CI: 1.07–4.46) but no significant difference in stroke rates. Among the other 13,392 patients with no renal indication for dose reduction, 13.3% were potentially underdosed, which was associated with a higher stroke risk (hazard ratio: 4.87; 95% CI: 1.30–18.26) with no difference in major bleeding amongst apixaban-treated patients. There were no statistically significant relationships in dabigatran- or rivaroxaban-treated patients without a renal indication. Hence, the presumption that underdoing leads to gains in safety are not borne out, but instead puts patients at risk of thromboembolism. This has been highlighted in other recent publications (7,8).
The study by Yao et al. (6) has many positive aspects, including a large sample size from a ‘real world’ claims dataset, as well as clear study endpoints and consideration of drug interactions. Nevertheless, the limitations should be recognised, as with any “real world” observational study based on claims or administrative data (9,10). Apixaban dosing criteria as per the approved product label requires two of the following three criteria: age ≥80 years, weight <60 kg, and SCr level >1.5 mg/dL (11). As with claims data, they were not able to check weights for apixaban, hence their main analyses relied on SCr level as the apixaban dose indication. Follow up times varied from 1 to 9.6 months, and thus, the absolute numbers of events and event rates were generally low, so longer term information would be needed especially for thromboembolism and mortality outcomes. Limited follow up may partly explain the lack of a statistically significant relationship between dose reduction and risk of stroke or bleeding in the dabigatran- or rivaroxaban-treated patients. Also, the CKD-EPI equation was used to calculate renal function rather than the Cockcroft-Gault method as information on patients’ weight was not available. As with claims data, we do not know if patient had additional risk factors and were prescribed the NOAC appropriately in the first instance, including information on laboratory values, proteinuria, etc.
What are the future considerations from this work? Potential overdosing (i.e., use of standard dose NOACs in patients with severe renal impairment) was associated with a doubled risk of bleeding with no attendant reduction in the risk of stroke. One might expect that increased NOAC exposure would further reduce stroke risk, but this observation suggested that the stroke reduction effect plateaued with escalating drug exposure. Perhaps the remaining stroke risk is attributable to athero-embolic disease or other non-cardio-embolic stroke sources not readily addressed with systemic anticoagulation therapy. This observation may illustrate the inflection point at which increased bleeding risk no longer justifies intensified anticoagulation therapy. Indeed, the residual risk of death and cardiovascular events in patients with AF despite adequate anticoagulation is well recognised (12,13), which is perhaps unsurprising given the multiple cardiovascular risk factors present in AF patients (14,15). More studies and better clinical decision support tools are needed to guide NOAC dosing, particularly in patients with renal impairment. This can be in the form of simple clinical pathways that align primary and secondary care management [“the Birmingham 3-step” approach to stroke prevention (16)], as well as the use of novel approaches to integrated care with mobile health technologies. The latter would suit certain healthcare settings, as recently shown in the mAFA trial (17), where the mAF App on smartphones, integrating clinical decision support, education, and patient-involvement strategies, significantly improved knowledge, drug adherence, quality of life, and anticoagulation satisfaction. Attention to long-term adherence, persistence and compliance with anticoagulation improves outcomes (18-20). Things can only get better if appropriate and responsible prescribing and treatment uptake prevails, balancing risk appropriately (21).
Acknowledgements
None.
Footnote
Conflicts of Interest: Professor Lip has served as a consultant for Bayer/Janssen, BMS/Pfizer, Biotronik, Medtronic, Boehringer Ingelheim, Microlife and Daiichi-Sankyo; and a speaker for Bayer, BMS/Pfizer, Medtronic, Boehringer Ingelheim, Microlife, Roche and Daiichi-Sankyo. No personal fees received. AA Khan has no conflicts of interest to declare.
References
- Lip G, Freedman B, De Caterina R, et al. Stroke prevention in atrial fibrillation: Past, present and future. Comparing the guidelines and practical decision-making. Thromb Haemost 2017;117:1230-9. [Crossref] [PubMed]
- Skjøth F, Larsen TB, Rasmussen LH, et al. Efficacy and safety of edoxaban in comparison with dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation. An indirect comparison analysis. Thromb Haemost 2014;111:981-8. [Crossref] [PubMed]
- Blann AD, Skjoth F, Rasmussen LH, et al. Edoxaban versus placebo, aspirin, or aspirin plus clopidogrel for stroke prevention in atrial fibrillation. An indirect comparison analysis. Thromb Haemost 2015;114:403-9. [Crossref] [PubMed]
- Lip GY, Fauchier L, Freedman SB, et al. Atrial fibrillation. Nat Rev Dis Primers 2016;2:16016. [Crossref] [PubMed]
- Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015;17:1467-507. [Crossref] [PubMed]
- Yao X, Shah ND, Sangaralingham LR, et al. Non-Vitamin K Antagonist Oral Anticoagulant Dosing in Patients With Atrial Fibrillation and Renal Dysfunction. J Am Coll Cardiol 2017;69:2779-90. [Crossref] [PubMed]
- Nielsen PB, Skjoth F, Sogaard M, et al. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ 2017;356:j510. [Crossref] [PubMed]
- Steinberg BA, Shrader P, Thomas L, et al. Off-Label Dosing of Non-Vitamin K Antagonist Oral Anticoagulants and Adverse Outcomes: The ORBIT-AF II Registry. J Am Coll Cardiol 2016;68:2597-604. [Crossref] [PubMed]
- Freedman B, Lip GY. "Unreal world" or "real world" data in oral anticoagulant treatment of atrial fibrillation. Thromb Haemost 2016;116:587-9. [Crossref] [PubMed]
- Potpara TS, Lip GY. Postapproval Observational Studies of Non-Vitamin K Antagonist Oral Anticoagulants in Atrial Fibrillation. JAMA 2017;317:1115-6. [Crossref] [PubMed]
- Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015;17:1467-507. [Crossref] [PubMed]
- Fauchier L, Villejoubert O, Clementy N, et al. Causes of Death and Influencing Factors in Patients with Atrial Fibrillation. Am J Med 2016;129:1278-87. [Crossref] [PubMed]
- Lip GY, Laroche C, Ioachim PM, et al. Prognosis and treatment of atrial fibrillation patients by European cardiologists: one year follow-up of the EURObservational Research Programme-Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur Heart J 2014;35:3365-76. [Crossref] [PubMed]
- Guo Y, Wang H, Tian Y, et al. Multiple risk factors and ischaemic stroke in the elderly Asian population with and without atrial fibrillation. An analysis of 425,600 Chinese individuals without prior stroke. Thromb Haemost 2016;115:184-92. [Crossref] [PubMed]
- Darwiche W, Bejan-Angoulvant T, Angoulvant D, et al. Risk of myocardial infarction and death in patients with atrial fibrillation treated with dabigatran or vitamin K antagonists. Meta-analysis of observational analyses. Thromb Haemost 2016;116:1150-8. [Crossref] [PubMed]
- Lip GY. Stroke prevention in Atrial Fibrillation. Eur Heart J 2017;38:4-5. [Crossref] [PubMed]
- Guo Y, Chen Y, Lane DA, et al. Mobile Health Technology for Atrial Fibrillation Management Integrating Decision Support, Education, and Patient Involvement: mAF App Trial. Am J Med 2017;130:1388-96.e6. [Crossref] [PubMed]
- Martinez C, Katholing A, Wallenhorst C, et al. Therapy persistence in newly diagnosed non-valvular atrial fibrillation treated with warfarin or NOAC. A cohort study. Thromb Haemost 2016;115:31-9. [Crossref] [PubMed]
- Rivera-Caravaca JM, Roldan V, Esteve-Pastor MA, et al. Cessation of oral anticoagulation is an important risk factor for stroke and mortality in atrial fibrillation patients. Thromb Haemost 2017;117:1448-54. [Crossref] [PubMed]
- Mazurek M, Shantsila E, Lane DA, et al. Guideline-Adherent Antithrombotic Treatment Improves Outcomes in Patients With Atrial Fibrillation: Insights From the Community-Based Darlington Atrial Fibrillation Registry. Mayo Clin Proc 2017;92:1203-13. [Crossref] [PubMed]
- Kittelson JM, Steg PG, Halperin JL, et al. Bivariate evaluation of thromboembolism and bleeding in clinical trials of anticoagulants in patients with atrial fibrillation. Thromb Haemost 2016;116:544-53. [Crossref] [PubMed]


