Thoracic perforations—surgical techniques
Introduction
Since the esophageal wall is thin, it is not only an organ that may get easily injured, but also it is unlikely to have end-to-end anastomosis due to the fact that its blood build up is poor. Traumatic defects of esophagus still have more than 20% mortality despite advanced intensive care (1). In the event of multiple organ failure and sepsis development, that rate may easily exceed 50%. A close relationship has been found as a result of critical clinical studies between the period between the beginning of the symptoms and the treatment and mortality (2).
Since esophageal perforation is a rare condition and its occurrence varies, there is difference of opinion about its diagnosis and treatment. According to minor retrospective series and to views of specialists, treatment firstly consists of surgical attempts.
Incidence and classification
It is quite difficult to calculate the true incidence of esophageal injuries. While the most frequent cause of esophageal injuries was spontaneous in the past, iatrogenic injuries have gained the first place today due to the fact that diagnostic and treatment-purpose endoscopical attempts have become common. While risk of esophageal injury is 0.018-0.003% for the flexible endoscopies, that rate is 0.11% for the rigid esophagoscopies, and that rate may go up to 10–15% with the addition of the treatment-purpose attempts (3,4).
In the event of cases such as Boerhaave syndrome where no instrumentation or intubation is available for esophagus, the spontaneously-occurring defects in the esophagus are generally called a rupture. On the other hand, esophageal perforation occurs due to an object entering into the esophageal lumen. Those lesions are traumatic, and for most of the cases, it occurs as a result of diagnostic or therapeutic interventions (5).
Penetrating injuries of esophagus most frequently occur in the neck, and thoracic injuries are seen approximately in one third of the cases (6). Traumatic esophageal injuries do not cause a complication leading to death in the early hours. Considering that heart and major vein injuries cause death at the scene of event or on the way to hospital, rates of the traumatic esophageal injuries in which autopsy studies are not included may be misleading.
Etiology
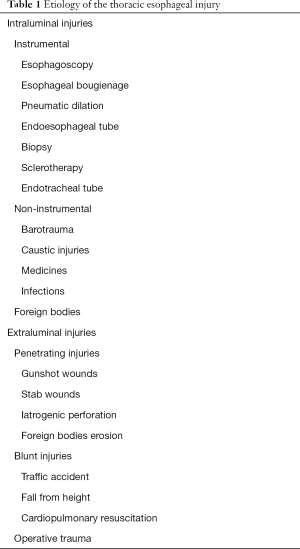
Esophageal injuries may be examined according to their etiology in two groups as intraluminal and extraluminal. The table shows the main headings of the factors found in etiology of the thoracic esophageal injury (Table 1).
Full table
Clinical findings
Even minimal nonspecific symptoms should not be ignored in the event of penetrating and blunt traumas of neck and thorax, drinking caustic substances, swallowing foreign bodies or removing foreign bodies from esophagus, attempts in or beyond esophagus, and the patients who have lately undergone a surgery. Even if the surgical attempt experienced is not for esophagus and the neighbouring structures, it should be kept in mind that a perforation may have developed in connection with esophageal intubation (7).
Clinical findings in esophageal injuries are soft at first, and they generally become evident after 24 h. In the event that there are not any accompanying complications during the early hours of the perforation such as pneumothorax or subcutaneous emphysema, there may not be any pathologies detected as a result of the physical examination. That condition is more frequently seen especially in the patients who have iatrogenical perforation and who have not oral intake. The patient may come with signs of sepsis following oral nutrition hours, days after the perforation.
The symptoms and the findings of the physical examination depend on the cause, localization and time of occurrence of the perforation. The most frequently seen symptoms are pain, fever, swallowing difficulties, dyspnea and subcutaneous emphysema. Mediastinal emphysema is in the first place in the thoracic perforation, and subcutaneous emphysema is detected by 30% (8,9). Despite the fact that pain is the most frequent finding, it is completely nonspecific. Despite the fact that fever is the indicator of a systemic inflammatory response and beginning of a possible infection, it is not specific. Quick and high fever is an indicator of toxic progression, and it is seen following the mediastinal perforation (5,9).
Pleural and mediastinal findings are frequent in the esophageal perforation, and they may help detect the region of injury. While a rupture found in the middle of the esophagus is generally likely to lead to right–sided pneumothorax/hydrothorax because of its neighbourhood with the right pleura, a distal thoracic rupture is likely to lead to mediastinal and left-sided findings.
In the spontaneous rupture of esophagus, the episode of vomiting is followed by severe chest pain, dyspnea, hematemesis, nausea, and sweating with chills. The pain may be substernal, epigastric, left lateral, or interscapular. At first, clinic signs of the patient lead to considering myocardial infarction, aorta dissectaneurysm or perforated peptic ulcer. Beginning of the pain with or following vomiting is important for diagnosis. Subcutaneous emphysema is not frequent in those patient at first, and it never develops in 2/3 of the patients. Epigastric sensitivity, defence and rebound may be taken in the patients. A septic shock table generally develops following the first 12 h (10).
Serohemorrhagic or serious hemorrhagic bloody fluid or eaten food residuals may be seen in thoracentesis or tube thoracostomy. In the event that oral methylene blue is drunk, it can be seen that it comes very rapidly from the chest tube (11).
Diagnosis
Early diagnosis of esophageal perforation is made through occurrence and radiological confirmation of the clinical findings. Direct graphy provides important clues for 70–90% of the cases for the diagnosis of esophageal perforations (7,12). Findings such as hydrothorax, pneumothorax, hydropneumothorax, pneumomediastinum, subcutaneous emphysema, mediastinal extension, subdiaphragmatic air, foreign bodies, retrotracheal extension may be detected. Mediastinal emphysema is found in approximately half of the esophageal perforations. Hyrdopneumothorax is detected in one fourth of the cases (13,14).
Esophagography is required in order to confirm the diagnosis, localize the perforation and determine the treatment for all of the cases with esophageal perforation. In the cases where perforation is found in the subesophageal section secondary to the instrumentation, it is frequently seen that the contrast agent overflows into the pleural space or into the mediastinum. In the event that it is still doubtful after the water soluble contrast esophagography or that it is not possible to make a certain localization anatomically, then the operation may be repeated with barium. However, most surgeons is worried about the extravasation of the barium into the thorax. Use of water soluble agents can detect 75% of thoracic perforations (15).
Tomographical evaluation with the contrast agent is another option for diagnosis. In computerized tomography (CT), pneumothorax, pneumomediastinum, subcutaneous emphysema, mediastinal extension, apse cavities, the lesion level, and foreign bodies, if any, can be seen. In some cases, CT can detect the very small extravasations of the contrast agent that cannot be seen in the standard graphies. CT can clearly show the emphysematous tissue plans and the developing apses. In addition, it helps detect the vertical spread of the infectious process in the mediastinum (7,16).
Final diagnosis of a rupture is seeing it endoscopically. Esophagoscopy both detects the diseases found together with the level of rupture and helps determine the method of treatment. On the other hand, use of endoscopy for diagnosis of esophageal perforation is controversial. Small perforations may even escape the notice of experienced endoscopists. In addition, entering into the laceration field with endoscope may make the perforation bigger, and create more contaminations (14).
Treatment
The fundamental principles in the primary and emergency treatment of esophageal perforation are early diagnosis, stabilization of the patient, and determining whether to use operative or nonoperative treatment. Variability of the clinical findings and difficulty of diagnosis often lead to delay in treatment. That situation is especially seen in the spontaneous ruptures where suspicion of esophageal perforation is clinically low. The fact that a delay of more than 24 h for diagnosis after a perforation leads to approximately a 2 times increase in mortality from 14% emphasizes the importance of early diagnosis and treatment (17).
Selection of the method of treatment depends on the cause and localization of the perforation, the underlying esophageal disease, time of diagnosis, condition of the esophagus, injury of the neighbouring organs, performance status and age of the patient. Even if indication of survival depends on the period of time passing between the perforation and the treatment, severity of the injury and experience of the surgeon are also important (18).
Pretreatment
In the event of suspicion of a perforation, treatment should be immediately started. First of all, oral intake is stopped. A wide intravenous vascular access is established, and a fluid replacement is applied with 0.9% isotonic sodium chloride solution and lactate ringer solution. Effective broad-spectrum antibiotic treatment is started for the aerob and anaerob microorganisms. The patient may be monitorized at the intensive care unit for hemodynamic monitarization, stabilization and volume replacement. A central venous catheter, a ureter catheter and an arterial catheter should be placed into those cases. Those preparations should not cause to postpone surgical evaluation and the treatment, on the contrary, they should accelerate the process in order to carry out the surgical treatment at the most appropriate time. The patient should be prepared for the surgical treatment with the laboratory tests (complete blood count, coagulation tests, electrolytes) and the chest radiographies (14,17,18).
Conservative treatment
Due to the fact that incidence of iatrogenical injuries has increased over the last several decades and that they have had quicker diagnoses and less extraluminal contamination, it is seen that conservative treatment applications have increased, too (19,20). Due to the fact that control of contaminated tissues is difficult in the event of perforation in the pleural or peritoneal cavities, conservative approaches are accepted as relatively contraindicated.
Medical treatment should only be applied for selected patients. Available option of surgical treatment should not be ignored while applying medical treatment. Endoscopy should definitely be used for such cases, and as a result, the perforation should be seen. Medical treatment is recommended in literature in the event of the following conditions for treatment of the thoracic esophageal perforation (19,21-25):
- A perforation with or without minimal extravasation limited with the involvement of mediastinum and in the absence of involvement in the pleural space in the contrast esophagogram;
- A perforation well-drained into the esophagus;
- In absence of sepsis findings;
- A small perforation;
- An old and weak patient;
- Iatrogenical minimal perforations;
- Absence of pleural effusion;
- A perforation that is detected and treated very late, and with a very bad prognosis;
- Observing clinical recovery 24 h after a conservative treatment;
- A perforation that is diagnosed late and well-surrounded;
- In the absence of an obstruction or a stricture in the region of the perforation.
The patients should be frequently evaluated, and be prepared for surgery if they need an operation. Imaging should be repeated for the patients who have symptoms of worsening clinical status or an infection. Well-localizable fluid collection may be drained in a percutaneous way in guidance of CT. Medically-treated patients should be followed without any oral intake for at least 7-10 days. In the event that the patients are stable during that period, integration of the esophagus is controlled by drinking gastrografin. In the event that a transition of contrast is found from the esophagus into the other spaces, parenteral nutrition is continued. When it is shown that there is no leakage in the esophagus, the patient can start oral intake. Liquid food starts to be taken, and proceed to the extent of toleration of the patient. In the event that there is no recovery and worsening is observed for clinical status of the patient 24 h after the beginning of the conservative treatment, then surgical intervention is compulsory.
Conservative treatment is less frequently used for the non-iatrogenical perforations. Therefore, almost all of the studies focused on treatment are surgical. Width of the injury is determined with surgical exploration, and the appropriate method of treatment is selected.
Operative treatment
The options involving the surgical treatment are simple drainage of the contaminated space, debridement with primary repair of the perforation, esophageal diversion and delayed repair or esophagectomy. A rarely-used and almost-abandoned option is placing a T-tube into the perforation in a percutaneous way. On the other hand, treatment should be determined according to individual criteria for each patient.
The purposes of the surgery are the debridement of the necrotic tissues, the repair of the perforation, the correction of the distal obstruction, the drainage of the contaminated and infected area, and nutrition jejunostomy (13,14,26).
Principles of surgical treatment
Even if the time of diagnosis is more than 24 h, the optimal treatment for the perforation of an esophagus is the primary repair of the region of the perforation. In the event of a diffuse mediastinal necrosis, a very large perforation in the esophagus that prevents approximating the mucosa again, or the patient being clinically unstable, primary repair cannot be considered as an option (13,14,26).
Primary surgical repair
It is the most frequently preferred type of a surgical attempt. The earlier the primary repair is applied, the bigger the success of the operation is. The repairs that are applied in the first 24 h have better results. In the event that a delay of more than 24 h is there for diagnosis or in the event of serious extraluminal contamination that is caused by a leakage of fluid and debris, effectiveness of the primary repair can be increased by using a vascularized tissue flap. For this purpose, intercostal muscle flaps are the most frequently used ones. Other options of flaps are the serratus muscle, the latissimus dorsi muscle, the diaphragm, the parietal pleura and the stomach fundus (27).
In the event that the surgical approach is being planned for the thoracic esophageal perforation, the relationship of the neighbouring vital structures with the esophagus should exactly be known. While approximating a perforation in the middle section of the esophagus from the sixth or seventh intercostal space by way of the right thoracotomy, it is required to approximate a perforation in the distal esophagus from the seventh or eighth intercostal space by way of left thoracotomy.
A posterior-based intercostal muscle flap is prepared in order to strengthen the primary repair before entering into the thoracic cavity. By applying a thoracotomy, with mobilization of the pleural fold and the inferior pulmonary ligament, mobilization of the lung toward the front is facilitated. The pleural space is cleaned, and the infarcts in the mediastinum are debrided. The esophagus is turned from the proximal and hanged with a penrose drain in order to help the dissection. Then, in order to completely evaluate the size of the mucosal injury, the muscle fibres both up and down the perforation are cut longitudinally. Expanding of the mucosal injury to the distal and poor visibility of the proximal section are the most common cause of the persistent leakages. Finally, the mucosa and the layer of muscles are closed in double one by one with absorbable sutures. Care must be taken not to lead to narrowness in the esophageal lumen by appropriate approximation. In the event that intercostal muscle flap cannot be obtained or that blood supply is poor, then the parietal pleura flap may be used alternatively instead of the intercostal muscle flap. The pleural space and the defect are irrigated well, and two chest tubes are placed. One of the chest tubes is placed into the posterior bazal. And the other chest tube is left near the region of injury in order to ensure sufficient drainage in the event that any problems arise in the primary repair. In the event that there are exudates and debris, pulmonary decortication should be applied in order to ensure sufficient lung expansion. A nasogastric tube is sent into the stomach in a way not to give any damage to the region of the repair. During the primary repair of the esophagus, a jejunostomy tube may be placed with mini laparotomy (28-31).
Postoperative treatment
Nutritional support is required until the patient starts and continues oral nutrition effectively. The patient does not have oral intake for approximately one week following the operation. The patient is provided with nutrition support two or three times a day with the jejunal food tube. The intravenous wide-spectrum antibiotic treatment is continued for 7–10 days depending on the clinical status of the patient. In the event that the patient is clinically stable, they are evaluated with a contrasted esophagogram on the seventh postoperative day. In the event that there are not any findings of an esophageal leakage or a postoperative ileus, then the nasogastric tube is removed, and nutrition is started with an oral liquid diet. After the patient tolerates the oral intake and any finding of leakage is eliminated clinically, the drains are removed (30,32).
Alternative approaches for primary surgical repair
In the cases where primary surgical repair is not technically possible, where the patient is hemodynamically unstable, or where a perforation is diagnosed immediately after an attempt, several different approaches have been defined. For instance, in the event of fragility of the extraesophageal tissues resulting from a delay in diagnosis and a serious mediastinitis in relation with necrosis, primary repair cannot be applied (28,30).
Drainage only
Drainage alone as an operative treatment is a valid application for the cervical esophageal perforations where the region of the perforation cannot be displayed completely and where it has no obstruction in the distal. Drainage alone is contraindicated for the thoracic and intraabdominal esophageal perforations due to the fact that the leakage cannot be controlled and that the neighbouring structures such as pleura and periton have contamination.
Authors recommend the use of the hybrid technique for the cases that have a large thoracic esophageal perforation, where the patient has an important comorbid disease and where there are findings of clinically mediastinal sepsis. That technique involves the aggressive debridement, the drainage, closing the defect with the muscle flap, and the placement of an endoscopic stent. The purposes of that approach are the septic contamination of the neighbouring structures and controlling of the leakage with reconstruction of the esophageal lumen for the cases that cannot tolerate a second operative approach with the aim of ensuring the continuity of the esophagus. Alternatively, a T-tube may be placed into the perforation for the cases that cannot tolerate a larger surgical operation (22,33,34).
Drainage of the thoracic perforation may not only be carried out with the placement of a closed tube thoracostomy, but also with an operative debridement or VATS by opening the thoracotomy. For all of the cases, the mediastinum should be left wide open, and the necrosed tissues should be debrided. The perforated region is debrided, and the drainage is carried out with the chest tube. The serum is given orally or with a naso-gastric catheter, and the region of the perforation can be washed in this way (35).
T-tube drainage
Placement of a T-tube, which is a controversial technique of diversion, is in fact forming an esophagocutaneous fistule. During the thoracotomy and debridement, the tube is placed away from the diaphragm and the aorta, to the region of the perforation. Supporters of that technique believe that it may be an alternative for a major surgery such as esophagectomy in the event of a serious level of damage. A gastrostomy and jejunostomy tube may also be placed for the purpose of nutrition and drainage. After recovery of the patient, the T-tube is removed, and recovery of the perforation is allowed. Recovery and closure of the perforation is followed with esophagography (36).
Diversion
Diversion is an operation where the esophageal content is directed rather than the primary repair of the perforation. In cases where the repair is not possible due to the fact that the patient is unstable, that there is a story of an esophageal disease, that the neighbouring tissues are fragile, and that the defect is large, it can be applied. Diversion ensures the control and the drainage of the extraluminal contamination. Esophagus is directed in the proximal with cervical esophagostomy, and the remaining esophagus is resected.
Cervical esophagostomy is approximated with left neck incision. In order to facilitate the esophagostomy process and the placement of the ostomy device on the anterior chest wall, the proximal length of the esophagus must be as much as possible. A subcutaneous tunnel is formed that reaches the chest wall from over the sternocleidomastoid muscle, the clavicle muscle and the pectoral muscle. The esophagostomy process must be carried out in literal position in order to avoid any complication that might require tracheostomy. The skin is excised for 1–2 cm as round in order to prevent any development of narrowness on the distal point of the tunnel. The proximal end of the esophagus is withdrawn from the tunnel, and the skin is identified strongly with absorbable sutures one by one. The neck incision is irrigated with serum physiological, and then closed. A drain is placed that reaches the superior mediastinum from the neck in order to help the drainage of the mediastinal contamination (37-40).
A flexible fiberoptic laryngoscopy must necessarily be conducted for those cases in order to evaluate the postoperative vocal cord functions; the esophagostomy must be dilated with the help of a finger in order to prevent the formation of a stricture and reduce the risk of aspiration pneumony, and a full nutritional support must be provided. Reconstruction of the esophagus must be typically carried out 6 months or 1 year after the perforation in order to ensure full recovery. Retrosternal colon interposition is generally required in order to ensure the continuity of the digestive system (41).
Minimally invasive techniques
A trend has developed in the principles of treatment towards the endoscopic operations such as the fibrin glue injection, the use of clips, and drug eluting self-expansable stents. Endoscopic repair is easy with hemoclip, in addition, it is considered safe and effective. It has additional advantages such as less pain in connection with the endoscopic operation, and a shorter period of hospitalization and a reduction in costs (42,43).
The endoscopic submucosal fibrin glue injection results in re-filling of the region of the perforation and in the stimulation of the granulation formation. The potential disadvantage of that operation is that it delays starting oral intake and that it requires multiple endoscopic sessions for the large perforations (44-46). For this reason, the endoscopic fibrin glue injection should be only used for the small esophageal perforations as in the endoscopic clip (less than 30%). Schubert et al. (47) have reported that they successfully treated endoscopically 25 of 27 patients who have mediastinal anastomotic leakage. Endoscopic lavage and leakage debridement must be carried out before closing the perforation.
Endoscopical stent placement
Today endoscopic drug eluting stents are used more and more frequently for the treatment of the thoracic esophageal perforations. Despite the fact that there is no general rule on that, a stent may be appropriate in the event of a serious comorbidity, an advanced stage mediastinal sepsis, a large esophageal defect or that patient being at a stage where they cannot tolerate a major surgical intervention (48,49).
Placement of a stent has been found to be ineffective in the event of an injury on the proximal of the cervical esophagus or on the gastroesophageal junction, segment injuries longer than 6 cm, and an anastomotic leakage found in the more distal conduit section (50,51).
Placement of an endoscopic stent for the esophageal perforation must be carried out fluoroscopy-guided. First of all, a diagnostic endoscopy is carried out in order to determine the exact location of the perforation and measure the size of the injury. The drug eluting stent must be at least 4 cm longer than the size of the damage. The stent must be able to cover an area of at least 2 cm from the proximal and the distal of the perforation. Placement of a stent into the distal esophagus might cause the distal section of the drug eluting stent to be found in the stomach lumen. In this case, tension of the stent, which is formed by radial pressure, is reduced, and frequency of migration increases. However, it is critically important that the distal end of the stent be at that localization in order to completely close and control the distal esophageal perforation (52,53).
Placement of an effective stent can restore the integrity of the lumen, and prevent further extraluminal leakage. In addition to that, the extraluminal contamination must be drained for an effective treatment of the esophageal perforations. A contrasted esophagogram-guided evaluation is carried out in order to evaluate the stent postoperatively placed and completely eliminate the perforation. In the event that the perforation is under control and that the patient is clinically stable, oral nutrition is started. Especially the stents that are placed in the distal esophagus might be followed with plain radiographies in terms of malposition (52,53).
Resection
Esophagectomy, which is very rarely used today, is the most appropriate approach both for primary and delayed reconstruction in some cases. That method is used for the patients who have a severe sepsis or an underlying esophageal disease. The indications of the esophagectomy involves distal obstruction occurring because of a peptic stricture, neuromotor dysfunction (achalasia containing megaesophagus), multiple esophageal strictures, corrosive esophageal burns, intrinsic diseases such as esophageal reflux or esophagitis, massive necrosis, serious mediastinal contamination and inflammatory reaction, or early-tried surgical drainage, or poor closure. Resection helps both eliminate the underlying disease and ensure the continuity of the gastrointestinal system (54-56).
In the event of a minimal pleural contamination or mediastinal restriction, irrigation and debridement of the contaminated space with the transhiatal esophagectomy might bring success. For the patients with chronic perforation who resist the other methods of treatment, the transthoracic approach might be required for the sufficient debridement of the mediastinum and the pleural cavity, or in order to carry out the dissection safely. Whatever the technique is, restoration for the continuity of the intestines must be carried out at the time of the first operation provided that the status of the patient is not critical. Otherwise, gastrostomy and jejunostomy are carried out along with the first proximal esophagostomy and esophagectomy. Reconstruction is carried out with a gastric tube or a colon placement in a substernal position where the natural esophageal support does not exist anymore 6 months or 1 year later (57,58).
Conclusions
Rate of mortality of the perforations in the thoracic region is higher than in the other regions. Early diagnosis and treatment are important for minimizing the rate of mortality of the thoracic esophageal perforation. In the event that a delay more than 24 h occurs in diagnosis and treatment, the rate of mortality significantly increases. In the cases where the pleura with no systemic symptom is intact, conservative treatment may be implemented. However, primary repair is the golden selection of a standard treatment for the thoracic esophageal perforations. Drainage operation alone is not appropriate for the perforations in that region.
Diversion is indicated for the cases that are not clinically stable, that are not acceptable for larger surgical operations, or where a large esophageal injury prevents primary repair. Esophagectomy is an operation that should be considered in the event of an end-stage benign esophageal disease and of a large esophageal damage that prevents primary repair. Despite the fact that there is no guideline for the esophageal stents, they might be appropriate in the event of a serious comorbidity, an advanced mediastinal sepsis or a large esophageal defect, and when the patient cannot tolerate a major surgical attempt. Today frequency of use of minimally invasive attempts for treatment of the esophageal perforation is increasing more and more.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Huber-Lang M, Henne-Bruns D, Schmitz B, et al. Esophageal perforation: principles of diagnosis and surgical management. Surg Today 2006;36:332-40. [Crossref] [PubMed]
- Wu JT, Mattox KL, Wall MJ Jr. Esophageal perforations: new perspectives and treatment paradigms. J Trauma 2007;63:1173-84. [Crossref] [PubMed]
- Eisen GM, Baron TH, Dominitz JA, et al. Complicasions of upper GI endoscopy Gastrointestinal Endoscopy 2002;55:784-93. [Crossref] [PubMed]
- Tullavardhana T. Iatrogenic Esophageal Perforation. J Med Assoc Thai 2015;98 Suppl 9:S177-83. [PubMed]
- Weber T. Esophageal rupture and perforation. In: Grosfeld J, O’neill J, Foncalsrud E, Coran A. editors. Pediatric surgery. Philadelphia, PA: Elsevier Mosby; 2012:889-92.
- Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma 2001;50:289-96. [Crossref] [PubMed]
- Faggian A, Berritto D, Iacobellis F, et al. Imaging Patients With Alimentary Tract Perforation: Literature Review. Semin Ultrasound CT MR 2016;37:66-9. [Crossref] [PubMed]
- Younes Z, Johnson D. The spectrum of spontaneous and iatrogenic esophageal injury: perforations, mallory-weiss tears, and hematomas. J Clin Gastroenterol 1999;29:306-17. [Crossref] [PubMed]
- Pasricha PJ, Fleischer DE, Kalloo AN. Endoscopic perforations of the upper digestive tract: a review of their pathogenesis, prevention, and mangagement. Gastroenterology 1994;106:787-802. [Crossref] [PubMed]
- Szeliga J, Jackowski M. Boerhaave syndrome. Pol Przegl Chir 2011;83:523-6. [Crossref] [PubMed]
- Wei L, Wang F, Chen S. A late diagnosed case of Spontaneous esophageal perforation in an elderly patient. Int J Clin Exp Med 2015;8:11594-7. [PubMed]
- Ghahremani G. Esophageal trauma. Semin Roentgenol 1994;29:387-400. [Crossref] [PubMed]
- Eroglu A, Kurkcuoglu IC, Karaoganoglu N, et al. Esophageal perforation: the importance of early diagnosis and primary repair. Dis Esophagus 2004;17:91-4. [Crossref] [PubMed]
- Eroglu A, Turkyilmaz A, Aydin Y, et al. Current management of esophageal perforation: 20 years experience. Dis Esophagus 2009;22:374-80. [Crossref] [PubMed]
- Foley MJ, Ghahremani GG, Rogers LF. Reappraisal of contrast media use to detect upper gastrointestinal perforations: comparison of ionic water-soluble media with barium sulfate. Radiology 1982;144:231-7. [Crossref] [PubMed]
- Fadoo F, Ruiz DE, Dawn SK, et al. Helical CT esophagography for the evaluation of suspected esophageal perforation or rupture. AJR Am J Roentgenol 2004;182:1177-9. [Crossref] [PubMed]
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [Crossref] [PubMed]
- Gupta NM, Kaman L. Personal management of 57 consecutive patients with esophageal perforation. Am J Surg 2004;187:58-63. [Crossref] [PubMed]
- Altorjay A, Kiss J, Vörös A, et al. Nonoperative management of esophageal perforations. Is it justified? Ann Surg 1997;225:415-21. [Crossref] [PubMed]
- Vogel SB, Rout WR, Martin TD, et al. Esophageal perforation in adults: aggressive, conservative treatment lowers morbidity and mortality. Ann Surg 2005;241:1016-21. [Crossref] [PubMed]
- Shaffer HA, Valenzuela G, Mittal RK. Esophageal perforation: a reassessment of the criteria for choosing medical or surgical therapy. Arch Intern Med 1992;152:757-61. [Crossref] [PubMed]
- Onwuka EA, Saadai P, Boomer LA, et al. Nonoperative management of esophageal perforations in the newborn. J Surg Res 2016;205:102-7. [Crossref] [PubMed]
- Pezzetta E, Kokudo T, Uldry E, et al. The surgical management of spontaneous esophageal perforation (Boerhaave's syndrome) – 20 years of experience. Biosci Trends 2016;10:120-4. [Crossref] [PubMed]
- Markar SR, Mackenzie H, Wiggins T, et al. Management and Outcomes of Esophageal Perforation: A National Study of 2,564 Patients in England. Am J Gastroenterol 2015;110:1559-66. [Crossref] [PubMed]
- Liu HC, Chen CH, Chan ML, et al. Management of Esophageal Perforations in Elderly Patients. Int J Gerontol 2015;9:107-10. [Crossref]
- Wright CD, Mathisen DJ, Wain JC, et al. Reinforced primary repair of thoracic esophageal perforation. Ann Thorac Surg 1995;60:245-8. [Crossref] [PubMed]
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- Chirica M, Champault A, Dray X, et al. Esophageal perforations. J Visc Surg 2010;147:e117-28. [Crossref] [PubMed]
- Jougon J, Mc Bride T, Delcambre F, et al. Primary esophageal repair for Boerhaave's syndrome whatever the free interval between perforation and treatment. Eur J Cardiothorac Surg 2004;25:475-9. [Crossref] [PubMed]
- Sung SW, Park JJ, Kim YT, et al. Surgery in thoracic esophageal perforation: primary repair is feasible. Dis Esophagus 2002;15:204-9. [Crossref] [PubMed]
- Sudarshan M, Elharram M, Spicer J, et al. Management of esophageal perforation in the endoscopic era: Is operative repair still relevant? Surgery 2016;160:1104-10. [Crossref] [PubMed]
- Nirula R. Esophageal perforation. Surg Clin North Am 2014;94:35-41. [Crossref] [PubMed]
- Santos GH, Frater RW. Transesophageal irrigation for the treatment of mediastinitis produced by esophageal rupture. J Thorac Cardiovasc Surg 1986;91:57-62. [PubMed]
- Chang CH, Lin PJ, Chang JP, et al. One-stage operation for treatment after delayed diagnosis of thoracic esophageal perforation. Ann Thorac Surg 1992;53:617-20. [Crossref] [PubMed]
- Cho JS, Kim YD. Treatment of mediastinitis using video-assisted thoracoscopic surgery. Eur J Cardiothorac Surg 2008;34:520-4. [Crossref] [PubMed]
- Nakabayashi T, Kudo M, Hirasawa T, et al. Successful late management of esophageal perforation with T-tube drainage. Case Rep Gastroenterol 2008;2:67-70. [Crossref] [PubMed]
- Urschel HC, Razzuk MA, Wood RE, et al. Improved management of esophageal perforation: exclusion and diversion in continuity. Ann Surg 1974;179:587-91. [Crossref] [PubMed]
- Lee YC, Lee ST, Chu SH. New technique of esophageal exclusion for chronic esophageal perforation. Ann Thorac Surg 1991;51:1020-2. [Crossref] [PubMed]
- Zumbro GL, Anstadt MP, Mawulawde K, et al. Surgical management of esophageal perforation: Role of esophageal conservation in delayed perforation. The American Surgeon 2002;68:36-40. [PubMed]
- Salo JA, Isolauri JO, Heikkila LJ, et al. Management of delayed esophageal perforation with mediastinal sepsis. Esophagectomy or primary repair? J Thorac Cardiovasc Surg 1993;106:1088-91. [PubMed]
- Thomas P, Fuentes P, Giudicelli R, et al. Colon interposition for esophageal replacement: current indications and long-term function. Ann Thorac Surg 1997;64:757-64. [Crossref] [PubMed]
- Blocksom JM, Sugawa C, Tokioka S, et al. The Hemoclip: a novel approach to endoscopic therapy for esophageal perforation. Dig Dis Sci 2004;49:1136-8. [Crossref] [PubMed]
- Shimamoto C, Hirata I, Umegaki E, et al. Closure of an esophageal perforation due to fishbone ingestion by endoscopic clip application. Gastrointest Endosc 2000;51:736-9. [Crossref] [PubMed]
- Pross M, Manger T, Reinheckel T, et al. Endoscopic treatment of clinically symptomatic leaks of thoracic esophageal anastomoses. Gastrointest Endosc 2000;51:73-6. [Crossref] [PubMed]
- Kimura T, Takemoto T, Fujiwara Y, et al. Esophageal perforation caused by a fish bone treated with surgically indwelling drainage and fibrin glue injection for fistula formation. Ann Thorac Cardiovasc Surg 2013;19:289-92. [Crossref] [PubMed]
- Fernandez FF, Richter A, Freudenberg S, et al. Treatment of endoscopic esophageal perforation. Surg Endosc 1999;13:962-6. [Crossref] [PubMed]
- Schubert D, Pross M, Nestler G, et al. Endoscopic treatment of mediastinal anastomotic leaks. Zentralbl Chir 2006;131:369-75. [Crossref] [PubMed]
- Lange B, Kubiak R, Wessel LM, et al. Use of fully covered self-expandable metal stents for benign esophageal disorders in children. J Laparoendosc Adv Surg Tech A 2015;25:335-41. [Crossref] [PubMed]
- Rollins MD, Barnhart DC. Treatment of persistent esophageal leaks in children with removable, covered stents. J Pediatr Surg. 2012;47:1843-7. [Crossref] [PubMed]
- Herrera A, Freeman RK. The Evolution and Current Utility of Esophageal Stent Placement for the Treatment of Acute Esophageal Perforation. Thorac Surg Clin 2016;26:305-14. [Crossref] [PubMed]
- Fischer A, Thomusch O, Benz S, et al. Nonoperative treatment of 15 benign esophageal perforations with self-expandable covered metal stents. Ann Thorac Surg 2006;81:467-72. [Crossref] [PubMed]
- Turkyilmaz A, Eroglu A, Aydin Y, et al. The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus 2009;22:119-26. [Crossref] [PubMed]
- Turkyilmaz A, Eroglu A, Aydin Y, et al. Complications of metallic stent placement in malignant esophageal stricture and their management. Surg Laparosc Endosc Percutan Tech 2010;20:10-5. [Crossref] [PubMed]
- Thyoka M, Barnacle A, Chippington S, et al. Fluoroscopic balloon dilation of esophageal atresia anastomotic strictures in children and young adults: single-center study of 103 consecutive patients from 1999 to 2011. Radiology 2014;271:596-601. [Crossref] [PubMed]
- Kroepil F, Schauer M, Raffel AM, et al. Treatment of early and delayed esophageal perforation. Indian J Surg 2013;75:469-72. [Crossref] [PubMed]
- Seo YD, Lin J, Chang AC, et al. Emergent Esophagectomy for Esophageal Perforations: A Safe Option. Ann Thorac Surg 2015;100:905-9. [Crossref] [PubMed]
- Orringer MB, Stirling MC. Esophagectomy for esophageal disruption. Ann Thorac Surg 1990;49:35-42. [Crossref] [PubMed]
- de Aquino JL, de Camargo JG, Cecchino GN, et al. Evaluation of urgent esophagectomy in esophageal perforation. Arq Bras Cir Dig 2014;27:247-50. [Crossref] [PubMed]


