The emerging role of sST2 blocking in the therapy of graft-versus-host disease
Suppression of tumorigenicity 2 (ST2) is an interleukin-1 (IL-1) receptor family member with transmembrane (mST2) and soluble isoforms (sST2) (1).
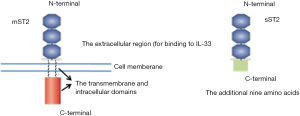
The mST2 is expressed on many types of cells including group 2 innate lymphoid cells (ILC2s), natural killer (NK) cells, Th1 cells, Th2 cells, regulatory T (Treg) cells and CD8+ T cells (2,3). While sST2, a soluble truncated form of mST2 without the transmembrane and intracellular domains, is secreted into the circulation.
Until now, the only known ligand of ST2 is IL-33, a member of the IL-1 family and mainly expressed in the nucleus of tissue lining cells, stromal cells, and activated myeloid cells (3). In the latest research we also found that IL-33 is highly expressed in the central nervous system (CNS) (4), in which IL-33 is over 10 fold more than in liver, spleen and lung (unpublished data from our lab). IL-33 is mostly released as a damage-associated molecular pattern (DAMP) molecule from damaged cells (2,3,5) or be processed and released from activated cells (2,4,6) to the extracellular milieu and plays an important role in many indicated diseases such as inflammatory bowel disease, allergy, autoimmune disease, transplantation rejection, graft-versus-host disease (GVHD), infectious disease, and cancers (3,5,7).
IL-33 exerts its cellular functions by binding a receptor complex composed of mST2 and IL-1R accessory protein to induce MyD88-dependent signaling. On the other hand, IL-33/mST2 signaling will be inhibited by sST2 which always functions as a “decoy” receptor to sequester free IL-33 (1,8). In multiple clinical trials, sST2 has emerged as a clinically useful prognostic biomarker in patients with cardiac diseases (1,9) and allergic and nonallergic pulmonary disease (10).
Zhang et al. are to be congratulated for revealing a potential therapeutic target of sST2 in GVHD, a devastating complication after allogeneic hematopoietic stem-cell transplantation (HSCT) (11). Allogeneic HSCT can cure haematological malignancies and inherited or acquired non-malignant disorders of blood cells, such as sickle-cell anaemia and aplastic anaemia. After chemotherapy, patients are transplanted with the bone marrow or peripheral-blood stem cells (PBSCs) from donors. Whereas bone-marrow cells and granulocyte colony-stimulating factor (G-CSF)-mobilized PBSCs are enriched for haematopoietic progenitors, and contain mature CD4+ and CD8+ αβ T cells. These T cells promote haematopoietic engraftment, reconstitute T-cell immunity (particularly in adults with reduced thymic function) and mediate a potent beneficial antitumour effect, known as graft versus leukaemia (GVL).Unfortunately, both of these donor T-cell subsets also cause graft-versus-host disease (GVHD), the broad attack against host tissues by donor T cells (12).
Clinical GVHD has two forms: acute GVHD is characterized by damage to the skin, liver and the gastrointestinal tract; whereas chronic GVHD has more diverse manifestations. Zhang et al. demonstrated that in the development of GVHD, as the main target organ, the intestine CD45–EpCAM–stromal cells and CD45-EpCAM–CD146+ endothelial cells, as well as donor T cells circulated in the intestine produced a large number of sST2 into plasma. When the full-length anti-ST2 mAb was applied, the severity and mortality of GVHD were reduced significantly (11). As for the probable pathway, there were four main points as follows: (I) ST2 blockade decreased the percentages of pathogenic TH1 cells and TH17 cells, so as the inflammatory cytokines IFN-γ, IL-17, and IL-23 were decreased; (II) the anti-ST2 mAb neutralized the sST2 and more free IL-33 bond to mST2-expressing T cells to drive the production of type 2 cytokines, which was responsible for protective type 2 inflammatory responses and promoted the expansion of regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), so as the release of anti-inflammatory cytokine IL-10 was increased; (III) the anti-ST2 mAb restrained sST2-producing T cells (such as TH17 and Tc17) to produce sST2; (IV) the anti-ST2 mAb inhibited the expansion of immunogenic CD103+ dendritic cells and the expression of MHC class II and costimulatory molecules (CD40, CD80, and CD86) on CD11c+ dendritic cells. In the meanwhile, sST2 blockade preserved substantial antitumoral cytotoxicity and GVL activity. Above all, it suggests that sST2 is a therapeutic target for severe GVHD in clinical trials.
The main promoter used for the expression of the ST2 gene is distinct among different cells or species (13,14). sST2 and mST2 mRNA in rats were generated by use of the proximal and distal promoters, respectively. In mice, differential mRNA processing within the ST2 gene generates two mRNAs of 2.7 and 5 kb, corresponding to shorter secreted sST2 and longer, membrane-anchored mST2 respectively. Hence, sST2 is identical with the extracellular region (for binding to IL-33) of mST2 except for an additional nine amino acids presented at the C terminus of the molecule (15,16) (Figure 1). Seemingly, it is difficult to develop a specific anti-ST2 mAb only against sST2 but not mST2.
Commendably, Zhang et al. demonstrated that the anti-ST2 mAb they used specifically inhibited sST2 by forming a stable complex with sST2 in circulating blood and also verified that the inhibitory effect was limited to the soluble form by measuring the frequency of ST2+ Tregs after treatment (11). The methods account for the effects of anti-ST2 antibody on distinct ST2 forms, but they remain far from enough. And administration of sST2 to ST2-knockout mice or selectively expressing either sST2 or mST2 in transgenic mice may be a feasible approach to disentangle the involvement of distinct ST2 forms in GVHD. It also accords with what Trajkovic et al. speculated in infection and autoimmune diseases (15). Thus, it seems that sST2 might present an important role in GVHD and more direct evidences for such hypothesis are urgent need.
In the research from Zhang et al., ex vivo systemic injections of IL-33 did not lead to improvement in the treated animals though anti-ST2 mAb did reduce the severity and mortality of GVHD (11). Despite of different disease model, we also observed the similar phenomenon in experimental autoimmune encephalomyelitis (EAE). Although IL-33 alone cannot relieve the progress of EAE, anti-IL-33 polyclonal antibody aggravated the disease apparently (unpublished data from our lab). Zhang et al. explained that endogenously produced IL-33 and exogenously administered IL-33 have different (I) circulating doses, (II) pharmacokinetics, and (III) binding properties in vivo. We consider another possibility that the mST2 in vivo is limited, so as the endogenous IL-33 is excessive that the exogenous IL-33 have no chance to exerts its cellular functions at all. While the endogenous IL-33 is blocked largely by anti-IL-33 antibody, its’ protective role emerges in the reverse direction.
In summary, Zhang et al. found that sST2 was an effective target to relieve GVHD in a minor histocompatibility antigen (miHA)–mismatched model of allo-HCT and a human-to-mouse xenogeneic model. It highlights the unique antagonistic action of anti-ST2 antibody to sST2 which also needs more to prove. sST2 blocking overcomes the difficulty that there is no effective strategy to control GVHD without decreasing GVL activity and the risk of leukemia relapse .
Acknowledgements
This work is supported by National Natural Science Foundation of China (Grant Number: 31470852).
Footnote
Provenance: This is a Guest Commentary commissioned by Section Editor Tingting Wu, MD (Department of Cardiology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mueller T, Jaffe AS. Soluble ST2--analytical considerations. Am J Cardiol 2015;115:8B-21B. [Crossref] [PubMed]
- Molofsky AB, Savage AK, Locksley RM. Interleukin-33 in Tissue Homeostasis, Injury, and Inflammation. Immunity 2015;42:1005-19. [Crossref] [PubMed]
- Lu B, Yang M, Wang Q. Interleukin-33 in tumorigenesis, tumor immune evasion, and cancer immunotherapy. J Mol Med (Berl) 2016;94:535-43. [Crossref] [PubMed]
- Chen H, Sun Y, Lai L, et al. Interleukin-33 is released in spinal cord and suppresses experimental autoimmune encephalomyelitis in mice. Neuroscience 2015;308:157-68. [Crossref] [PubMed]
- Garlanda C, Dinarello CA, Mantovani A. The interleukin-1 family: back to the future. Immunity 2013;39:1003-18. [Crossref] [PubMed]
- Peine M, Marek RM, Löhning M. IL-33 in T Cell Differentiation, Function, and Immune Homeostasis. Trends Immunol 2016;37:321-33. [Crossref] [PubMed]
- Reichenbach DK, Schwarze V, Matta BM, et al. The IL-33/ST2 axis augments effector T-cell responses during acute GVHD. Blood 2015;125:3183-92. [Crossref] [PubMed]
- Oshikawa K, Yanagisawa K, Tominaga S, et al. Expression and function of the ST2 gene in a murine model of allergic airway inflammation. Clin Exp Allergy 2002;32:1520-6. [Crossref] [PubMed]
- Bayes-Genis A, Zhang Y, Ky B. ST2 and patient prognosis in chronic heart failure. Am J Cardiol 2015;115:64B-9B. [Crossref] [PubMed]
- Bajwa EK, Mebazaa A, Januzzi JL. ST2 in Pulmonary Disease. Am J Cardiol 2015;115:44B-7B. [Crossref] [PubMed]
- Zhang J, Ramadan AM, Griesenauer B, et al. ST2 blockade reduces sST2-producing T cells while maintaining protective mST2-expressing T cells during graft-versus-host disease. Sci Transl Med 2015;7:308ra160. [Crossref] [PubMed]
- Shlomchik WD. Graft-versus-host disease. Nat Rev Immunol 2007;7:340-52. [Crossref] [PubMed]
- Iwahana H, Yanagisawa K, Ito-Kosaka A, et al. Different promoter usage and multiple transcription initiation sites of the interleukin-1 receptor-related human ST2 gene in UT-7 and TM12 cells. Eur J Biochem 1999;264:397-406. [Crossref] [PubMed]
- Gächter T, Werenskiold AK, Klemenz R. Transcription of the interleukin-1 receptor-related T1 gene is initiated at different promoters in mast cells and fibroblasts. J Biol Chem 1996;271:124-9. [Crossref] [PubMed]
- Trajkovic V, Sweet MJ, Xu D. T1/ST2--an IL-1 receptor-like modulator of immune responses. Cytokine Growth Factor Rev 2004;15:87-95. [Crossref] [PubMed]
- Bergers G, Reikerstorfer A, Braselmann S, et al. Alternative promoter usage of the Fos-responsive gene Fit-1 generates mRNA isoforms coding for either secreted or membrane-bound proteins related to the IL-1 receptor. EMBO J 1994;13:1176-88. [PubMed]