Implications of obesity in exceptional longevity
Except for the world’s poorest regions, it is estimated that global obesity [body mass index (BMI) >30 kg/m2] prevalence will reach 18% (men) and >21% (women) by 2025 (1). Recent nationally representative surveys in the US for the 2013–2014 period indicate age-adjusted obesity prevalence of 35.0% and 40.4% among adult men and women, respectively (2) and of 17.0% for children and adolescents aged 2–19 years (3). On the other hand, because healthy life expectancy also shows global improvement, the world is becoming apparently heavier and healthier (4). This finding is paradoxical given the association of obesity, and especially severe/morbid obesity, and/or its metabolic consequences with all-cause mortality as well as with a broad range of diseases and health complaints (5). In fact, recent data suggest that life expectancy will start to decline in the US over this century. Accordingly, we could be approaching a tipping point where technological and medical care advances might no longer compensate for our poor lifestyle habits (6).
Centenarians show exceptional longevity (~20+ years more than the average Westerner) and most have postponed, and some even escaped major diseases despite their advanced age. The latter represents the paradigm of extended healthy life expectancy that any individual would dream of reaching.
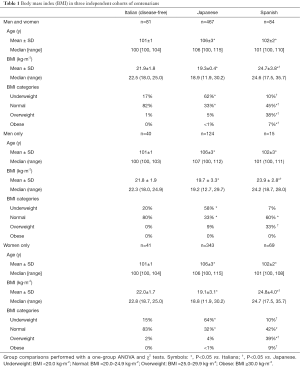
We assessed BMI in three independent centenarians’ cohorts of both sexes that we have studied extensively (7): n=81 from Northern Italy (Lombardy, Piedmont); n=84 from Spain (central area); and n=467 from Japan [participants in the Tokyo Centenarians and semi-supercentenarians (SS) study] (7). The Italian centenarians were free of major age-related diseases (cancer, CVD, dementia). BMI assessment was done during 2009–2013 (Spain), 2011–2014 (Italy), 2000–2004 (Japanese centenarians) and 2002–2016 (Japanese SS) (7). We compared BMI mean values and categories across cohorts with one-group ANOVA and χ2 tests, respectively. We obtained approval from the local ethics committees [European University of Madrid (Spain), 2E Science (Italy), and Keio University (Japan)]. The study followed the tenets of the Declaration of Helsinki for Human Research.
Results are shown in Table 1. Aside from some geographic-specific differences (Japanese centenarians had the lowest BMI and a high prevalence of underweight–which is concurrent with the typical profile of this country compared with most Western societies), a main result is that the percentage of obese centenarians was well below the estimated current values for adults [age-standardized obesity of 10.8% (95% CI: 9.7–12.0) in men and 14.9% (95% CI: 13.6–16.1) in women] (1). Notably, we found no obese male centenarians in any of the cohorts. Italy has one of the world’s highest percentages of obese people [ranked number 9 (men) and 14 (women) in 2014] (1). And yet there were no obese disease-free centenarians in the Italian cohort.
Full table
According to our results, obese people do not show healthy life expectancy. Compared to other hominoids, humans show an evolved predisposition to deposit fat. Such adaptation maintains energetic homeostasis in times of energy shortfalls and might contribute to explain the energetic paradox that, despite having a higher reproduction output with larger neonates as well as a higher metabolic rate than any other hominoid, humans live longer (8). However, the evolutionary trade-off between the competitive needs of reproduction and growth on the one hand, and maintenance, on the other hand, has been recently disrupted in modern societies living in obesogenic environments. We are becoming progressively inactive (with 1/3 of adults worldwide engaging in <150 min/week of exercise) while eating poor-quality diets at the cost of increasing adiposity to pathogenic levels and making obesity becoming virtually a pandemic.
Obesity prevention is one of the interventions to be kept in mind to promote successful aging. This is even more urgent when considering the potential health- and economic-related effects of the 21th century obesity pandemic. Our data support recent initiatives, e.g., using mobile technology for preventing obesity-related behaviors in at-risk children (9) or pilot research indicating the cost-effectiveness of childhood interventions to combat obesity (10).
Acknowledgements
Funding: Research in the field by A. Lucia is supported by grants from the Spanish Ministry of Economy and Competitiveness [Fondo de Investigaciones Sanitarias (FIS), grant number PI15/00558] and Fondos Feder. A. Lucia and H. Pareja-Galeano are supported by grants from Cátedra Real Madrid-Universidad Europea (#2015/02RM and 2016/RM02, respectively). F. Sanchis-Gomar is supported by a post-doctoral contract granted by Conselleria de Educación, Investigación, Cultura y Deporte de la Generalitat Valenciana (APOSTD/2016/140).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387:1377-96. [Crossref] [PubMed]
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 2016;315:2284-91. [Crossref] [PubMed]
- Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014. JAMA 2016;315:2292-9. [Crossref] [PubMed]
- Smith GD. A fatter, healthier but more unequal world. Lancet 2016;387:1349-50. [Crossref] [PubMed]
- Patterson RE, Frank LL, Kristal AR, et al. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med 2004;27:385-90. [Crossref] [PubMed]
- Ludwig DS. Lifespan Weighed Down by Diet. JAMA 2016;315:2269-70. [Crossref] [PubMed]
- Garatachea N, Emanuele E, Calero M, et al. ApoE gene and exceptional longevity: Insights from three independent cohorts. Exp Gerontol 2014;53:16-23. [Crossref] [PubMed]
- Pontzer H, Brown MH, Raichlen DA, et al. Metabolic acceleration and the evolution of human brain size and life history. Nature 2016;533:390-2. [Crossref] [PubMed]
- Nollen NL, Mayo MS, Carlson SE, et al. Mobile technology for obesity prevention: a randomized pilot study in racial- and ethnic-minority girls. Am J Prev Med 2014;46:404-8. [Crossref] [PubMed]
- Gortmaker SL, Long MW, Resch SC, et al. Cost Effectiveness of Childhood Obesity Interventions: Evidence and Methods for CHOICES. Am J Prev Med 2015;49:102-11. [Crossref] [PubMed]


