The immunocompromised oncohematological critically ill patient: considerations in severe infections
Introduction
Despite therapeutic progress made in the field of infections, sepsis and septic shock remain a major cause of mortality among critically ill patients. This is particularly relevant among cancer patients as highlighted by different series, showing that up to one in five patients admitted to intensive care units (ICU) with sepsis have cancer, and also, sepsis is one of the leading reasons for ICU admission in patients with cancer (1,2). This specific type of patient differs from the general population, when those presents these complications are often accompanied with higher risk of death, even 10-fold greater according to some series (3). In recent years the controversy for admission to these patients to an ICU, the risk factors for mortality, and the prognosis afterwards has been retaken due to relatively few data assessing this matter.
The severity of the inflammatory response in an already fragile economy makes this subset of patients prone to rapid decompensation. This condition is in addition to the higher susceptibility of these group for life threatening infectious complications; that might be explained by: the improvements in cancer care that have led to patients to live much longer and thus they may be exposed to the immunosuppression caused by the underlying disease for a longer period of time (in which severe infections may occur). On the other hand, some newer treatment strategies have become more aggressive or more prolonged, or develop new treatment-related complications once again increasing the immunosuppression time, accompanying the susceptibility for opportunistic and severe infections to take place. Third, in a specific group of these patients the source of infection becomes a clinical challenge, due to the difficulty for the prompt identification in patients with abnormal immune function, and symptoms of infection are often diminished. (4) Finally, in the last decade’s mortality has dropped among patients with malignancies, in consequence, the number of these patients admitted to an ICU with cancer has increased (5).
The increase survival rate in these patients have an possible explanation; first the utilization and development of targeted anti-tumor therapies, the advances in prompt identification of cancer patients, the better and current understanding of the pathophysiological mechanisms of organ dysfunction and the continuous improvement in supportive organ techniques and all the variables that critical care involves (mechanical ventilation, nutrition support, sedation, analgesia, hemodynamic monitoring, etc.) may play a role.
Here the authors present a review on particular issues regarding general management of severe infections in oncohematological critically ill patient as common immunosuppressed patient admitted to an ICU, in order to give a current scenario and future directions where clinical trials should be advised. The analysis of human immunodeficiency virus and organ transplant recipient are beyond this review.
Immune system impairment and infections in the oncohematological critically ill
The type of infection in the critically ill immunocompromised patient depends on the interaction of several factors:
- The Host: type and degree of immune system compromise (cellular vs. humoral, length of impairment, neutropenia), and presence of disruption of natural defense barrier (external devices such as catheters, or mucositis). While patients suffering leukemia (acute and chronic) or lymphoma, have predominant impairment on cellular immunity and phagocytosis; bone marrow transplant patients have the whole immunity (cellular and humoral) impaired, and also long periods or neutropenia. On the other hand, patient with solid malignancy suffer from anatomical issues, such as compression, ulceration or obstruction due to the mass (6).
- The Bug: the possible etiologies of infections are diverse, they range from common bacterial and viral pathogens, to opportunistic organisms that are clinically relevant only for immunocompromised hosts;
- The Setting: these patients are not only in risk for community acquired infections, but they are also continuously exposed to health care contact, and therefore prone to acquire multidrug resistant organisms’ infections.
The combination of these components as long as the specific treatments, affect patient condition augmenting the susceptibilities for specific microorganisms.
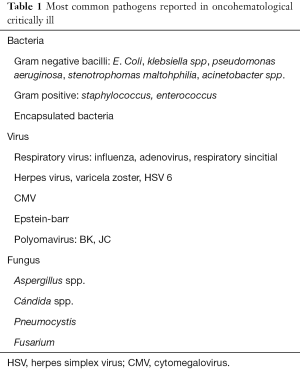
Among all the etiologies, bacteria remain globally the most common pathogen, while the fungus predominate on patients with longer neutropenia periods; also viruses are becoming more important due to the increased potency of the immunosuppressant treatments.
Although gram negative bacilli colonizing digestive tract mucosa remain the main cause of infections, in the last years the incidence of gram positive bacterial infection has increased. This might be related to the extended use of medical devices (e.g., central lines, urinary catheters) or to the frequent use of chemoprophylaxis. Table 1 shows most common pathogens reported in these patients (7).
Full table
Regarding site of infection in patients presenting with septic shock, when compared to no cancer patients, some differences have been noticed when assessed (8), being the first location the lung, followed by abdominal sepsis more common in solid tumor patients, and blood stream infection was more common in hematological patients.
Ethics: admission criteria and end-of-life decision
Nowadays, taking into account only the diagnosis of cancer to consider ICU admission of patients who need full-supporting management is no longer justified, even more, there is some data that ICU and hospital mortality rates were similar in patients with solid tumors and those without cancer (8). However, some discrepancies exist with hematological patients admitted to an ICU due to septic shock; in that same report this group had the higher ICU and Hospital mortality, associated with a higher need of vasopressors, and renal replacement therapy but no differences in mechanical ventilation days.
The classical criteria have showed poor prediction when triaging cancer patients, as reported by Thiéry et al. (9). In that report the authors evaluated the characteristics of both solid and hematological cancer patients considered for admission to ICU for different clinical conditions (shock, respiratory failure, coma, sepsis). A 51% was admitted, 26.2% were considered too sick to benefit, and 22.8% were described as too well to benefit. Of the patients considered too sick to benefit, 26% were alive on day 30, and 16.7% on day 180. Among patients considered too well to benefit, the 30-day mortality was 21.3%. This suggests that current clinical indications for the admission of these patients may not be sufficient and probably translated into increased mortality for the patients. Both the excess mortality in too-well patients and the relatively good survival of too-sick patients suggest the need for a broader admission policy, where future studies are required.
When a doubt exists about the criteria for ICU admission, not only a trial of ICU management should be proposed to assert that no patients could benefit from it or withhold the opportunity for recovering from the acute condition (10), but also an early admission, to prevent more derangement, and thus impact on mortality (11).
Recent opinions (10,12) promote the idea of intensive management over the first three to seven days, before making a final decision (ICU trial) to consider keep down intensive, or the change in label, from full code treatment to trial or end-life-decision; allowing an interdisciplinary meeting to the better assessment. A reliable tool to asses which cancer patients are more likely going to benefit from intensive care is yet to be designed. More studies are needed to develop the ideal method to discriminate who might benefit from intensive treatment; for example, to know if 72 hours are enough or the intensity of the initial treatment in an already fragile patient.
Conclusions
Even when life expectancy of oncohematolgical patients has increased, mortality when admitted to ICU remains high. Sepsis is one of the leading causes of admission of these patients. Admission criteria to the ICU urges to get new recommendations since the classic predictors of mortality among these patients has expired. Finally, we encourage an early ICU admission to prevent further organ derangement, and a concise, multidisciplinary and continuous re-evaluation, addressing response to treatment, or reconsideration of re-labeling in case of deterioration despite full support.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009;302:2323-9. [Crossref] [PubMed]
- Rosolem MM, Rabello LS, Lisboa T, et al. Critically ill patients with cancer and sepsis: clinical course and prognostic factors. J Crit Care 2012;27:301-7. [Crossref] [PubMed]
- de Montmollin E, Tandjaoui-Lambiotte Y, Legrand M, et al. Outcomes in critically ill cancer patients with septic shock of pulmonary origin. Shock 2013;39:250-4. [Crossref] [PubMed]
- Zafrani L, Azoulay E. How to treat severe infections in critically ill neutropenic patients? BMC Infect Dis 2014;14:512. [Crossref] [PubMed]
- Azoulay E, Pène F, Darmon M, et al. Managing critically Ill hematology patients: Time to think differently. Blood Rev 2015;29:359-67. [Crossref] [PubMed]
- Azoulay E, Schlemmer B. Diagnostic strategy in cancer patients with acute respiratory failure. Intensive Care Med 2006;32:808-22. [Crossref] [PubMed]
- Infección en el paciente crítico inmunodeprimido. XXIII reunión del grupo de trabajo de enfermedades infecciosas (G.T.E.I.) de la semicyuc. Available online: http://www.semicyuc.org/sites/default/files/00.01-programa_preliminar_gtei__valencia-2012_0.pdf.
- Taccone FS, Artigas AA, Sprung CL, et al. Characteristics and outcomes of cancer patients in European ICUs. Crit Care 2009;13:R15. [Crossref] [PubMed]
- Thiéry G, Azoulay E, Darmon M, et al. Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 2005;23:4406-13. [Crossref] [PubMed]
- Ñamendys-Silva SA, Plata-Menchaca EP, Rivero-Sigarroa E, et al. Opening the doors of the intensive care unit to cancer patients: A current perspective. World J Crit Care Med 2015;4:159-62. [PubMed]
- Song JU, Suh GY, Park HY, et al. Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med 2012;38:1505-13. [Crossref] [PubMed]
- Xia R, Wang D. Intensive care unit prognostic factors in critically ill patients with advanced solid tumors: a 3-year retrospective study. BMC Cancer 2016;16:188. [Crossref] [PubMed]


