Patient satisfaction at 2 months following total knee replacement using a second generation medial-pivot system: follow-up of 250 consecutive cases
Introduction
Total knee replacement (TKR) has been associated with relatively high levels of patient dissatisfaction despite being one of the most successful orthopaedic surgeries. Recent studies have reported rates of dissatisfied or neutral TKR patients nearing 25% (1-5), which is substantial when compared to the low rate (7%) reported for total hip replacement (THR) (6). The cause of dissatisfaction following TKR is likely multifactorial, but most studies have focused on patient-related factors such as low preoperative functional and mental scores, depression, pre- and postoperative pain, and high preoperative expectations (1,3). Another aspect of TKR that has not been fully evaluated, but almost certainly contributes to patient perception of their procedure, is the design of the implant used.
A recent randomized controlled trial of bilateral patients implanted with different TKR designs in each knee reported that a medial-pivot design (ADVANCE®, MicroPort Orthopedics Inc., Arlington, TN, USA) was preferred by subjects who had posterior-stabilized, mobile-bearing, or posterior cruciate ligament (PCL) retaining designs implanted in their contralateral knees (7). The author of the study hypothesized that implant designs that allow for sliding of the femur on the tiba during movements such as ascending and descending stairs may lead to a feeling of instability and increased synovial fluid generation, which result in reduced patient satisfaction. The author further stated the stability provided by the medial-pivot design in both the anterior and posterior directions may have provided patients with a greater sense of stability than was achieved with the other designs and that the single radius curvature of the medial-pivot femoral component enhanced quadriceps function. This enhanced quadriceps function has been confirmed in recent studies showing increased quadriceps efficiency in patients implanted with this design compared to those implanted with a posterior-stabilized system when performing sit-to-stand, level walking, and inclined walking tasks (8,9).
The primary objective of the current study was to assess patient satisfaction at 2 months for the first 250 consecutive TKRs performed using a second generation medial-pivot system (EVOLUTION®, MicroPort Orthopedics Inc., Arlington, TN, USA). The key differences between the first and second generations are that the second generation features an asymmetrical tibial base, an increased number of sizes, and size interchangeability. This cohort included the surgeon’s initial cases with the system, although the surgeon did have previous experience with the first generation system. It was anticipated that the rate of dissatisfied or neutral patients would be lower than those previously reported for TKR due to the unique design features of this system. These features include: a tibial insert with medial anterior and posterior lips to substitute for both the PCL and anterior cruciate ligament (ACL) and in turn minimize the femoral sliding that could be associated with a patient sensing instability; medial and lateral femoral condyles with constant radii of curvature to enhance quadriceps function (8,9); and a conforming medial compartment on the tibial insert resulting in kinematics that closely replicate the motion of the natural knee (10).
Methods
The first 250 consecutive TKRs performed by a single surgeon using this second generation medial-pivot system were assessed using a patient satisfaction assessment, the Knee Injury and Osteoarthritis Outcome Score (KOOS), range of motion, and radiographs at 2 months. The patient satisfaction assessment consisted of the surgeon asking subjects to rate their satisfaction with their procedure as “very satisfied”, “satisfied”, “OK”, or “not satisfied”. Consecutive subjects were divided into series of 50 consecutive cases to determine if there was any bias towards the initial surgeries with regards to patient satisfaction. Prior to enrollment, this study obtained ethics approval and informed consent was obtained.
All TKRs were implanted by a single surgeon using a modified medial parapatellar approach. The PCL was released in all cases and the ligaments were balanced. All tibial and femoral components were implanted using cemented fixation and the patella was replaced in all subjects. Deep vein thrombosis (DVT) prophylaxis was performed using a 14-day oral regimen of apixaban (2.5 mg, twice daily). The postoperative care regimen included the use of a single shot of a long acting local anaesthetic with immediate mobilization. Epidural pain pumps were not used in any subjects. Subjects were discharged home routinely on the third postoperative day, the majority leaving without walking assistance. This is an accelerated discharge, as the national average in Belgium approximately 8 days.
Results
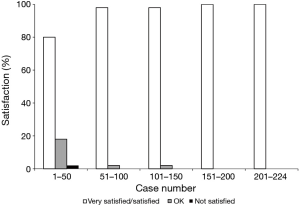
Of the 250 TKRs, 224 (89.6%) completed the 2-month patient satisfaction questionnaire. The overall very satisfied/satisfied rate was 94.6%. Eleven subjects (4.9%) reported “OK” satisfaction and only a single subject (0.4%) reported being “not satisfied”. Figure 1 shows patient satisfaction divided into 50 consecutive cases. The lone “not satisfied” subject and all but 2 of the “OK” subjects occurred within the first 50 cases. Following case 50, the overall very satisfied/satisfied and OK rates were 99.4% and 0.6%, respectively. There were no dissatisfied subjects after case 26.
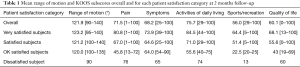
The median range of motion was 125° (range, 90°–140°). KOOS subscores for pain, symptoms, activities of daily living, sports/recreation, and quality of life were 71.5 (range, 1–100), 68.2 (range, 25–100), 75.7 (range, 29–100), 56.0 (29–100), and 60.1 (range, 0–100), respectively (Table 1). Scores were higher for the very satisfied and satisfied subjects than for the OK subjects. Radiographic outcomes showed no indications of loosening or osteolysis in any subjects. There were four incidents of DVT, but no other postoperative complications. At the time of manuscript preparation, there had been no revisions for any reason.
Full table
Discussion
As expected, the rate of dissatisfied (0.4%) or neutral (4.9%) subjects implanted with this second generation medial-pivot system was much lower than has been previously reported for TKR (11.8–23.2%) (1-5) and was very similar to rates reported for THR (7.0%) (6). Unfortunately there is minimal literature detailing patient satisfaction for specific devices available for comparison. Scott et al. reported an overall dissatisfaction rate of 18.6% for a cohort of 1,290 consecutive TKRs performed using mainly three implant designs: PFC Sigma (DePuy Synthes Joint Reconstruction, Warsaw, IN, USA); Kinemax (Stryker Orthopaedics, Mahwah, NJ, USA); and Triathlon (Stryker Orthopaedics, Mahwah, NJ, USA) (3). The authors did not report patient satisfaction for each design individually, but did state that there was no statistical difference in levels for each of the implants. Wylde et al. performed a randomized controlled trial comparing satisfaction following TKR using the Kinemax with either fixed or mobile bearing implants (4). The authors found no statistical difference in dissatisfaction rates with 13.0% of fixed and 11.8% of mobile-bearing patients dissatisfied. Giesinger et al. reported patient dissatisfaction rates of 22.5% and 23.2% at 2 and 12 months, respectively, for over 1,000 consecutive TKRs performed using the LCS rotating platform system (DePuy Syntheses Joint Reconstruction, Warsaw, IN, USA) (5).
The current study is one of the only to report TKR patient satisfaction at follow-up of less than 6 months. The majority of studies report satisfaction rates at 6 or 12 months because patients continue to recover functional abilities for at least 6 months following TKR. Kennedy et al. reported the greatest recovery, as determined by the 6-minute walk test and lower extremity functional scale, occurs during the first 12 weeks following surgery (11). Patients in that study continued to experience slower rates of improvement after 12 weeks until 26 weeks. Overall satisfaction from the current study was 94.6% at 2 months when subjects would be expected to continue to improve in their functional recovery and possibly satisfaction levels. The previously mentioned studies reported dissatisfaction rates of 11.0% to 23.2% at 6 or 12 months when it could be expected that patient functional recovery was complete. It is possible that subjects in the current study experienced higher levels of satisfaction or even faster recovery due to the enhanced quadriceps efficiency and stability previously described for this system.
There was a bias to the first cases with regards to subject satisfaction. Subjects within the first 50 cases had satisfaction rates at 2 months similar to those previously described for TKR. Following these cases, satisfaction rates improved beyond those reported for TKR, and even those for THR, with only two subjects reporting not being satisfied or very satisfied. There are several possible reasons for this bias. The surgeon did not switch exclusively to the subject system initially and continued to use a different TKR system for some patients during this period. Additionally, as with any implant system there are always aspects of the surgical technique that can be perfected over time while also adjusting to new instrumentation. One example with the subject system is ensuring the medial side is tighter than the lateral to ensure the lateral condyle can pivot around the medial.
In addition to patient satisfaction, subjects were also evaluated using traditional measures of clinical success. Functional outcomes, as assessed by the KOOS and range of motion, were all satisfactory and improved at final follow-up. There were no indications of loosening or osteolysis found during the radiographic analyses. Complications were rare and none of those that occurred were related to the implant or the surgical technique. There were no revisions for any reason. Satisfactory early clinical success was expected as the subject medial-pivot system features only minor modifications from its predecessor, which has a nearly 20-year history of clinical success (7,12-18).
Limitations
Despite being a follow-up of a relatively large consecutive cohort, there are some limitations to the current study. Mainly, it is not possible to definitively attribute the improvement in patient satisfaction seen to the implant design alone. Factors including surgeon skill and bedside manner, the type of recovery protocol used, the friendliness of the hospital staff, quality of the hospital facilities, and many others can contribute to patient perception of the procedure. Another limitation is that the patient satisfaction questionnaires from each of the previous studies and the current study were all slightly different and administered at different follow-up times. These factors have the potential to contribute to some of the differences seen in patient satisfaction rates.
Conclusions
In conclusion, more subjects implanted with this second generation medial-pivot system were satisfied than previously reported for TKR. Future multicenter studies are needed to determine if this promising trend continues at longer follow-up intervals and for different surgeons.
Acknowledgements
None.
Footnote
Conflicts of Interest: DA Fitch is an employee of MicroPort Orthopedics Inc., the other author has no conflicts of interest to declare.
Ethical Statement: This study obtained ethics approval of AZ Maria Middelares (No. 2015.049) and written informed consent was obtained from all patients.
References
- Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63. [Crossref] [PubMed]
- Robertsson O, Dunbar M, Pehrsson T, et al. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 2000;71:262-7. [Crossref] [PubMed]
- Scott CE, Howie CR, MacDonald D, et al. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 2010;92:1253-8. [Crossref] [PubMed]
- Wylde V, Learmonth I, Potter A, et al. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 2008;90:1172-9. [Crossref] [PubMed]
- Giesinger JM, Hamilton DF, Jost B, et al. WOMAC, EQ-5D and knee society score thresholds for treatment success after total knee arthroplasty. J Arthroplasty 2015;30:2154-8. [Crossref] [PubMed]
- Anakwe RE, Jenkins PJ, Moran M. Predicting dissatisfaction after total hip arthroplasty: a study of 850 patients. J Arthroplasty 2011;26:209-13. [Crossref] [PubMed]
- Pritchett JW. Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty 2011;26:224-8. [Crossref] [PubMed]
- Czyrnyj C, Reynolds S, Dervin G, et al. Muscle activation patterns during inclined gait: Comparison between medial pivot and posterior stabilized knee prostheses. European Federation of National Associationsof Orthopaedics and Traumatology 16th Congress. Prague, Czech Republic, 2015.
- Czyrnyj C, Reynolds S, Dervin G, et al. Muscle activation and functional performance following TKA: a comparison between prosthetic designs. 2015 Canadian Orthopaedic Association Annual Meeting. Vancouver, British Columbia, Canada, 2015.
- Schmidt R, Komistek RD, Blaha JD, et al. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res 2003.139-47. [Crossref] [PubMed]
- Kennedy DM, Stratford PW, Riddle DL, et al. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther 2008;88:22-32. [Crossref] [PubMed]
- Chinzei N, Ishida K, Tsumura N, et al. Satisfactory results at 8 years mean follow-up after ADVANCE® medial-pivot total knee arthroplasty. Knee 2014;21:387-90. [Crossref] [PubMed]
- Fitch DA, Sedacki K, Yang Y. Mid- to long-term outcomes of a medial-pivot system for primary total knee replacement: a systematic review and meta-analysis. Bone Joint Res 2014;3:297-304. [Crossref] [PubMed]
- Karachalios T, Roidis N, Giotikas D, et al. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee 2009;16:484-8. [Crossref] [PubMed]
- Minoda Y, Kobayashi A, Iwaki H, et al. Polyethylene wear particles in synovial fluid after total knee arthroplasty. Clin Orthop Relat Res 2003.165-72. [Crossref] [PubMed]
- Schmidt R, Ogden S, Blaha JD, et al. Midterm clinical and radiographic results of the medial pivot total knee system. Int Orthop 2014;38:2495-8. [Crossref] [PubMed]
- Vecchini E, Christodoulidis A, Magnan B, et al. Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. Knee 2012;19:851-5. [Crossref] [PubMed]
- Karachalios T, Varitimidis S, Bargiotas K, et al. An 11- to 15-year clinical outcome study of the Advance Medial Pivot total knee arthroplasty: pivot knee arthroplasty. Bone Joint J 2016;98-B:1050-5. [Crossref] [PubMed]


