A rare case of metastatic germ cell tumor to stomach and duodenum masquerading as signet ring cell adenocarcinoma
Introduction
Adenocarcinoma of stomach is the commonest malignancy involving the stomach. It consists of two distinct types: intestinal type and diffuse type. A conventional intestinal type of adenocarcinoma consists of glandular structures of varying proportions depending on degree of differentiation while diffuse type of adenocarcinoma consists of singly permeating tumor cells. A ‘signet ring’ cell is a prototype of diffuse gastric cancer, although several morphologic variations exist. There are certain uncommon tumors occurring in stomach which can mimic adenocarcinoma of stomach. We report an extremely rare occurrence of metastatic seminoma to stomach which had a striking histologic resemblance to signet ring carcinoma. Implications of correct diagnosis are also discussed along with recognising this diagnostic pitfall.
Case presentation
A 49 years old male presented to us with moderate intensity abdominal pain for the last 1 month. The pain was dull aching in nature and localised to epigastric region without any radiation or any specific aggravating and relieving factors and subsided spontaneously or sometimes with antacids. It did not restrict his activities of daily living. The patient was taking carbimazole for last 4–5 years for hyperthyroidism which was currently controlled. On examination there were no significant findings. The patient underwent an upper GI endoscopy before he presented to us wherein an ulceroproliferative growth was mentioned in the distal stomach. Biopsy was obtained from the tumor and sent for histology examination; the report of which stated the diagnosis of adenocarcinoma.
He was investigated further at Tata Memorial Hospital. Contrast-enhanced computed tomography (CECT) of abdomen, thorax and pelvis revealed a large soft tissue mass in suprarenal region bilaterally which was inseparable from adrenal glands with prominent external iliac and mesenteric nodes. There were no liver or lung metastasis or ascites. Biopsy from the tumor was reviewed and revealed a malignant tumor diffusely permeating through the gastric antral type of mucosal fragments. Tumor cells showed ‘diffuse’ pattern without any glandular formations. Individual tumor cells displayed large, hyperchromatic nucleus and clear cytoplasm. Morphology of tumor cells had a striking resemblance to diffuse type of gastric adenocarcinoma with signet ring cell morphology. However, immunohistochemistry (IHC) revealed only weak positivity for AE1/AE3 (epithelial marker) while other epithelial markers namely cytokeratin (CK), epithelial membrane antigen (EMA) and carcino embryonic antigen (CEA) as well as markers for lymphoma were negative. Diagnosis of poorly differentiated adenocarcinoma was offered mainly based on tumor cell morphology supported to some extent by weak positivity for AE1/AE3. Clinically, the diagnosis of metastatic adenocarcinoma of stomach was acceptable due to endoscopic findings of a gastric antral mass and bilateral adrenal metastasis.
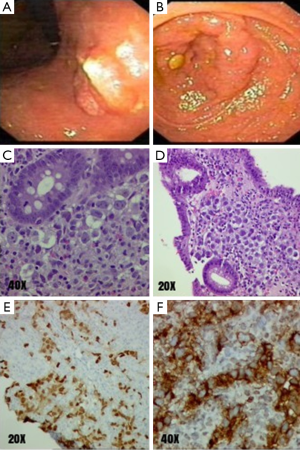
Repeat endoscopy examination at our hospital showed a 1 cm × 2 cm area of nodularity on the posterior wall of stomach and a circumferential proliferative growth in second portion of duodenum which caused luminal stenosis (Figure 1). Biopsy was taken from both sites. Histopathological examination revealed tumor morphology to be exactly similar to the one seen in earlier biopsy. A diffuse infiltration by a malignant tumor was seen in the lamina propria. The tumor cells were arranged in small clusters cords and also singly scattered. They showed large vesicular nuclei with prominent nucleoli and abundant clear cytoplasm. Conspicuous granulomatous response was also seen within the gastric mucosa. IHC for epithelial markers (AE1/AE3, CK and EMA) and lymphoma markers were negative except weak and focal positivity for AE1/AE3 similar to earlier findings. In view of these unexpected findings after IHC, possibility of germ cell tumor (GCT) was considered and appropriate markers were asked for. Tumor cells strongly expressed markers used for GCT, namely (Ckit, D2-40 and Oct3/4). Hence at this juncture, diagnosis was revised to metastatic GCT and further clinical evaluation in this regard was advised in order to substantiate the diagnosis. Tumor cell morphology was indicative of seminoma.
Re-look examination revealed enlarged right testis. An USG examination of scrotum showed right testicular enlargement measuring 4.0 cm × 2.8 cm. An ill-defined heterogeneously hypoechoic mass with foci of calcification and minimal vascularity was seen which was suspicious of right testicular lesion. Serum alpha fetoprotein (AFP) levels were raised −15,810.73 ng/mL while the beta HCG levels were normal at 5.3 mIU/mL. A positron emission tomography-contrast-enhanced computed tomography (PET-CECT) showed metabolically active disease in the duodenum, bilateral adrenals, mediastinal, and pelvic lymph nodes. The possibility of a retroperitoneal node infiltrating into duodenum was considered unlikely as the lesion was circumferential in the duodenum. The suprarenal lesion appeared to arise from the adrenal. Biopsy from the left adrenal too revealed identical tumor histology. Thus the revised histopathological diagnosis of GCT was corroborating with clinical findings and biochemical parameters. The final diagnosis of metastatic GCT (likely to be mixed GCT) of stage III-C was accepted and treatment was advised accordingly.
Discussion
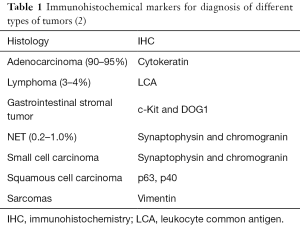
Gastric adenocarcinoma is an aggressive tumor where the survival rates are amongst the worst of any solid tumor—the 5-year survival being 3.1% with advanced gastric cancer and 27% in all cases in the US (1). Although adenocarcinoma is the commonest tumor of the stomach, other primary tumors like gastrointestinal stromal tumors (GIST), neuroendocrine tumors (NET) and lymphomas also occur, albeit infrequently. Histological recognition of different tumors is important since their prognosis and management differ. Histological diagnosis is made upon morphological features and ancillary tests, especially IHC. Table 1 shows typical immunohistochemical profile of malignant tumors occurring in stomach.
Each of these tumor types is associated with its respective distinctive morphological and immunohistochemical features. However, each of the above tumor types also has variations in usual morphology wherein the differential diagnosis of adenocarcinoma would be considered. For example, epithelioid variant of gastrointestinal stromal tumor and a high grade non-Hodgkin’s lymphoma can closely resemble adenocarcinoma of stomach. Such diagnostic dilemmas are often solved with the help of appropriate panel of IHC markers.
The stomach can also be a rare site of tumor metastasis. The most commonly described primary sites are breast, melanoma, lung, ovary, liver, colon and testis (3). The prevalence varies from 1.7–5.4% in autopsy studies (4,5). On the other hand, common sites of metastasis of testicular GCT are the lymph nodes, liver, lung, bones and brain. Metastases to the stomach from a testicular GCT are extremely rare though autopsy findings indicate a much higher incidence (6). Gastric metastases are nonspecific in endoscopic appearance (infiltration, ulcer, proliferative lesion etc.).
The stomach is affected by GCT either primarily or by metastasis from gonadal GCT. Primary GCT of stomach is a rare event; teratoma being the commonest type, rarer are yolk sac tumors and choriocarcinomas (7,8). To the best of our knowledge, primary seminoma has not been reported, although very few reports of metastasis of testicular seminoma to stomach are found in the literature. GCTs are tumors with a good prognosis as against gastric adenocarcinoma. Even for patients with advanced stage testicular GCT, approximately one-half can be cured with aggressive treatment (8–10). Our case exemplifies this rare occurrence and highlights certain histological and clinical challenges.
In our case, gastric mucosa was being permeated by metastatic seminoma cells which were found in small clusters and mostly singly scattered within the lamina propria. The tumor cells showed a striking resemblance to signet ring cell adenocarcinoma cells. Due to the rarity of possibility of metastasis of a seminoma to stomach, this diagnosis was not at all considered in the first instance. Low index of suspicion could have led to a serious misdiagnosis with corresponding potential for mistreatment. Moreover, presence of disseminated disease in the form of bilateral adrenal metastasis was also in favour of gastric adenocarcinoma. However, IHC for epithelial markers was consistently negative except weak and focal positivity for AE1/AE3 which raised the doubt about the diagnosis of adenocarcinoma. Differential diagnoses of epithelioid gastrointestinal stromal tumor, metastatic malignant melanoma and non-Hodgkin’s lymphoma were considered and respective panels of IHC were asked for. Amongst the panel, tumor cells strongly expressed Ckit, however DOG1 was negative. At this juncture, a possibility of metastatic seminoma was thought about and additional markers namely D2-40 and Oct3/4 were done which were positive in tumor cells. Thus we arrived at this diagnosis in a step wise fashion. Lack of typical IHC profile for adenocarcinoma combined with tumor morphology eventually guided us towards the correct diagnosis. Following revised histopathology diagnosis, clinical examination and biochemical parameters revealed a testicular mass and raised serum alpha-fetoprotein levels. These findings further supported the diagnosis of metastasis of seminoma to stomach. Raised levels of serum AFP indicated a possibility of mixed GCT. The gastric biopsy however did not reveal any other component than seminoma. The patient was started on chemotherapy for high risk testicular GCT.
In every day clinical practice, it is always prudent to think of ‘common’ conditions first. However, rare diagnosis should also be kept in mind. Any deviations from conventional situations should lead to further thoughts and corresponding investigations. Our case is an example of one such occurrence wherein metastatic seminoma masqueraded as signet ring cell adenocarcinoma of stomach. Our patient could have been misdiagnosed and mistreated as an advanced gastric cancer in the absence of an accurate pathology report when he actually had a tumor amenable for cure despite having metastases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- NIH Surveillance, Epidemiology, and End Results Program. SEER Stat Fact Sheets: Stomach Cancer. Accessed September 7, 2014. Available online: http://seer.cancer.gov/statfacts/html/stomach.html
- Oien KA, Dennis JL. Diagnostic work-up of carcinoma of unknown primary: from immunohistochemistry to molecular profiling. Ann Oncol 2012;23 Suppl 10:x271-7. [Crossref] [PubMed]
- Menuck LS, Amberg JR. Metastatic disease involving the stomach. Am J Dig Dis 1975;20:903-13. [Crossref] [PubMed]
- Higgins PM. Pyloric obstructions due to a metastatic deposit from carcinoma of the bronchus. Can J Surg 1962;5:438-41. [PubMed]
- Davis GH, Zollinger RW. Metastatic melanoma of the stomach. Am J Surg 1960;99:94-6. [Crossref] [PubMed]
- Bredael JJ, Vugrin D, Whitmore WF Jr. Autopsy findings in 154 patients with germ cell tumors of the testis. Cancer 1982;50:548-51. [Crossref] [PubMed]
- Knapp RH, Hurt RD, Payne WS, et al. Malignant germ cell tumors of the mediastinum. J Thorac Cardiovasc Surg 1985;89:82-9. [PubMed]
- Takeda S, Miyoshi S, Ohta M, et al. Primary germ cell tumors in the mediastinum: a 50-year experience at a single Japanese institution. Cancer 2003;97:367-76. [Crossref] [PubMed]
- Dueland S, Stenwig AE, Heilo A, et al. Treatment and outcome of patients with extragonadal germ cell tumours--the Norwegian Radium Hospital's experience 1979-94. Br J Cancer 1998;77:329-35. [Crossref] [PubMed]
- Albany C, Einhorn LH. Extragonadal germ cell tumors: clinical presentation and management. Curr Opin Oncol 2013;25:261-5. [PubMed]