History of previous knee surgery does not affect the clinical outcomes of primary total knee arthroplasty in an Asian population
Introduction
With the increasing number of knee surgeries performed for patients, it is likely that patients presenting for total knee arthroplasty (TKA) have had previous knee surgeries and certain knee surgeries, such as anterior cruciate ligament reconstruction (ACLR) and high tibial osteotomy (HTO), which will result in a higher likelihood of requiring future TKA (1-4). However, there is relatively limited data in current literature on how previous knee surgery could affect the age at which TKA is performed, as well as the outcomes of TKA (5) in an Asian population. These are clinically significant questions, as patients often enquire about the risks of TKA following a history of previous knee surgery.
Therefore, this study aims to evaluate the impact of previous knee surgeries on the timing and clinical outcomes of future TKA. Parameters assessed include patients’ age, post-operative clinical outcomes, quality of life and patient-reported satisfaction in those who have a history of knee surgery, as compared to those without a history of knee surgery. We hypothesize that patients with a history of knee surgery will undergo TKA at a significantly younger age as compared to those without a history of knee surgery, but they should have similar post-operative clinical outcomes.
Methods
Study design
This study was performed at Singapore General Hospital, Singapore, Republic of Singapore. Centralized Institutional Review Board approval was obtained for this study (CIRB 2015/2626). We retrospectively analyzed prospectively-collected data from a total joint registry of a tertiary hospital of patients who underwent primary TKA by a single senior surgeon over a 5-year period between January 2007 and December 2012, with a minimum of 2 years follow-up. Patients with a diagnosis of contralateral TKA, revision TKA and inflammatory arthroplasty were excluded from the study to limit the number of intra- and post-operative variables. All patients included in the study underwent TKA for symptomatic knee pain caused by osteoarthritis of the knee, which has failed conservative management. All patients were placed on a standardized post-operative clinical pathway for arthroplasty surgery and underwent supervised physical therapy post-operatively by trained physiotherapists.
Patient metrics
The patient’s age, gender, body mass index (BMI) and any history of previous knee surgeries were evaluated at the time of TKA. Information regarding the nature of the previous knee surgery was obtained from the patients’ medical records and intra-operative notes. The time interval between the previous knee surgery and current TKA was also recorded for all patients. Clinical parameters were assessed pre-operatively and post-operatively at 6 months and 2 years. Patient-reported outcome measures were assessed using a self-administered patient questionnaire containing the SF-36 Health Survey, Oxford Knee Score (OKS), and Knee Society Score (KSS), so as to evaluate the impact of TKA pre-operatively and at 6 months and 2 years follow-up. The KSS was further stratified into a functional component (KSS-functional score), which includes ability to walk distances and climb up and down stairs, and a objective component (KSS-objective score), which includes pain, range of motion, stability and alignment.
We also evaluated patients’ opinions as to whether the surgery met their expectations and whether they were satisfied with the results of their surgery, using two questions adopted from the validated North American Spine Society (NASS) questionnaire. The two questions were (I) “Has the surgery met your expectations so far?” and (II) “How would you rate the overall results of surgery?”. For question 1, patients had the choice of selecting from the following answers: (I) yes, totally; (II) yes, almost totally; (III) yes, quite a bit; (IV) more or less; (V) no, not quite; (VI) no, far from it; or (VII) no, not at all. For question 2, patients had the choice of selecting from the following answers: (I) excellent; (II) very good; (III) good; (IV) fair; (V) poor; or (VI) terrible. Patients were defined as either having their expectations met by their surgeries (responses to question 1 =1–4) or not having their expectations met by their surgeries (responses to question 1 =5–7). Patients were defined as either satisfied (responses to question 2 =1–3) or dissatisfied (responses to question 2 =4–6).
Statistical analysis
A paired t-test was used to compare the patients’ age at the time of TKA, BMI and clinical outcomes between patients with previous knee surgery and patients without a history of knee surgery. For all analyses, statistical significance was defined as a P value of 0.05 or less. All statistical analysis was performed using SPSS version 21 (SPSS, Inc., Chicago, Illinois, USA) with consultation from biostatisticians.
Results
A total of 303 patients (220 males, 83 females) met the criteria and were included in this study. Of these 303 patients, 29 (9.6%) had a previous history of knee surgery. Pre-operative radiological investigations showed that these 29 patients had Kellgren-Lawrence grade III/IV before their TKA. The most common type of knee surgery performed prior to TKA was arthroscopic partial meniscectomy and chondroplasty (21 patients; 72.4%), followed by HTO (6 patients; 20.7%) and ACLR (2 patients; 6.9%). All patients with a history of knee surgery underwent a standard midline incision and medial parapatellar approach. Patients who had previous HTO had their HTO staples removed during TKA. In addition, those with a history of previous knee surgery, including HTO, did not undergo revision surgeries at follow-up. The patients who had a previous history of ACLR and HTO had a mean interval of 13.5 and 9.2 years respectively before subsequent TKA. Patients who underwent arthroscopic debridement with pre-existing knee osteoarthritis underwent TKA about 4 years post-arthroscopy. There is one patient with a history of meniscectomy at a young age of 33 underwent TKA 30 years post-knee surgery.
The patients’ age, gender, pre-operative BMI and clinical parameters are shown in Table 1. There was no significant difference in BMI between the two groups of patients (27.0 vs. 27.2; P=0.77). The mean time interval from index knee surgery to subsequent TKA is 6.6 and 5.2 years in patients with previous knee arthroscopy with meniscectomy and chondroplasty. At the time of primary TKA, the mean age of patients with a history of knee surgery was significantly younger (61.0±6.2, P=0.0002) than the mean age of those without a history of knee surgery (66.1±7.7).
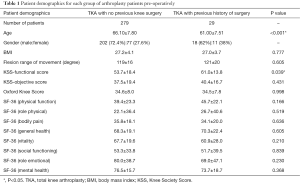
Full table
Pre-operatively, only the KSS-function score was significantly different between the two groups of patients with and without previous history of knee surgery (61.0 vs. 53.7; P=0.039). The rest of the clinical scores (flexion range of movement, KSS-knee score, OKS and SF-36) were similar between the two groups (P>0.05).
The same trend is seen at 6 months follow-up, when there was no significant difference between both groups in terms of flexion range of movement, KSS-knee score, SF-36 and OKS (P>0.05), while the KSS-function score remained significantly higher in patients with previous knee surgery (76.8 vs. 69.5; P=0.045). This is shown in Table 2.
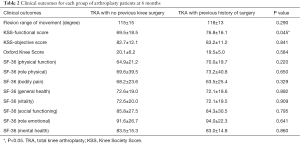
Full table
At 2 years follow-up, only SF-36 (physical role functioning) was significantly different between the two groups of patients with and without previous history of knee surgery (58.6 vs. 77.6; P=0.038). Those patients without a previous knee surgery had a better SF-36 (physical role functioning) outcome. The remaining clinical outcome scores for both groups did not show any significant difference (P>0.05). The post-operative clinical outcomes at 2 years are shown in Table 3.
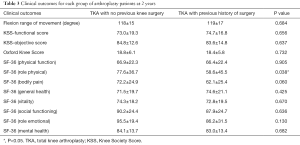
Full table
In terms of patient-reported satisfaction and expectation scores at 2 years follow-up, 85.7% of patients who had a history of knee surgery reported that they were satisfied with the results of surgery and 92.6% felt that the surgery met their expectations. In patients without a history of knee surgery, 89.2% were satisfied with the results of surgery and 87.4% felt that the surgery met their expectations.
Discussion
In our study, approximately 10% of patients who underwent TKA had a history of previous knee surgery, of which knee arthroscopy, followed by HTO and ACLR were commonest. This finding corresponds with current literature, in which many studies have shown that the incidence of TKA is increased by previous knee surgery (1,5-10). For ACLR, it is reported that the cumulative incidence of TKA is low at 1.4% (4). However, this incidence is still seven times greater than the general population (4,7-15). Similarly, in a 10-year follow-up study by Wasserstein et al. [2014] (11), 7.3% of patients who underwent fracture fixation of the tibial plateau subsequently had a TKA. This corresponds to a 5.3 times increase in likelihood of requiring a TKA as compared to a matched group from the general population. In addition, Brophy et al. [2014] (1) reported that 30% of their patients who underwent TKA for osteoarthritis or post-traumatic arthritis had a history of previous knee surgery.
A history of previous knee surgery did not appear to have a significant relationship with pre-operative baseline clinical scores and BMI, as these parameters were relatively similar between the two groups of patients. However, a larger proportion of patients with a history of previous knee surgery in our study were male (62%), which corresponds with the current literature (1). Patients with a history of knee surgery were also shown to undergo TKA at a significantly younger age of 61 years old as compared to those without with a mean interval time of 6.6 years from index knee surgery to subsequent TKA. Patients with a history of knee surgery have a better pre-operative KSS functional score, which could be due to this younger group of patients having greater function pre-operatively. The other pre-operative clinical scores for patients with a history of knee surgery were similar to those without previous knee surgery. This may signify that the former group of patients have developed symptomatic osteoarthritis necessitating TKA at a younger age, as they have relatively similar pre-operative baseline scores as their more elderly counterparts. Having a TKA at a younger age carries its implications, such as the potential need for revision TKA in the future and an overall increase in the demand for TKA in the general population (16-18). Nonetheless, this should not deter patients from undergoing knee surgery when necessary, as the development of osteoarthritis is multifactorial and cannot be solely attributed to a previous surgery. For example, in ACL injuries, concomitant meniscal or chondral injuries, post-operative excessive musculoskeletal loading, high BMI and inadequate strength training can all result in early osteoarthritis (19-21). In our study, patients who underwent previous knee surgery had no reported complications necessitating re-operation or revision surgeries on their follow-up visits (longest follow-up being up to 8 years after TKA).
In our 2-year follow-up study, patients with and without a history of previous knee surgery have similar clinical outcome scores, quality of life outcomes, patient-reported satisfaction scores and most were of the opinion that TKA has met their expectations. Also, in our follow-up, patients with a history of previous knee surgery did not require re-operations or revision surgeries. Therefore, this shows that previous knee surgery does not adversely affect the outcome of TKA and does not increase the risk of re-operation or revision surgeries in the early follow-up period. This information is important to clinicians when counselling patients for knee surgery.
One limitation of our study is that there may be a selection bias, as only patients with previous knee surgeries who eventually underwent TKA were analyzed in this study. As such, the actual incidence of future TKA following previous knee surgery is not known. We also do not have a longer follow-up (i.e., more than 10 years) of the younger patients with a history of knee surgery who underwent primary TKA to evaluate if they eventually required revision TKA. Although most studies of primary TKA have a larger proportion of female patients, in our study, we have excluded all patients with a history of contralateral knee arthroplasty, thus there were more male than female patients.
Our study’s strength lies in its contribution to current literature by addressing a clinically important question of whether a history of previous knee surgery would affect the outcomes of TKA. To our knowledge, there has been no reported study in the Asian population with regards to the impact of previous knee surgery on the clinical outcome and time interval to subsequent TKA. This is particularly important for clinicians in Asian populations, where there is a higher prevalence of knee osteoarthritis and hence, a greater need and demand for TKA.
Conclusions
In our study, a history of knee surgery had TKA at a significantly younger age than those without. However, this does not adversely affect the clinical and quality of life outcomes of their TKA. These patients have similar clinical outcomes as those without previous knee surgery; in addition, a high proportion of these patients are satisfied with the results of surgery and feel that their expectations of TKA are met. All of this serves as pertinent information for clinicians, in order to provide accurate and effective pre-operative counselling.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Centralized Institutional Review Board approval was obtained for this study (CIRB 2015/2626).
References
- Brophy RH, Gray BL, Nunley RM, et al. Total knee arthroplasty after previous knee surgery: expected interval and the effect on patient age. J Bone Joint Surg Am 2014;96:801-5. [Crossref] [PubMed]
- MacLean CH. Quality indicators for the management of osteoarthritis in vulnerable elders. Ann Intern Med 2001;135:711-21. [Crossref] [PubMed]
- Jüni P, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol 2006;20:721-40. [Crossref] [PubMed]
- Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 1998;80:163-73. [PubMed]
- Hawker G, Guan J, Judge A, et al. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am 2008;90:2337-45. [Crossref] [PubMed]
- Leroux T, Ogilvie-Harris D, Dwyer T, et al. The risk of knee arthroplasty following cruciate ligament reconstruction: a population-based matched cohort study. J Bone Joint Surg Am 2014;96:2-10. [Crossref] [PubMed]
- Lidén M, Sernert N, Rostgård-Christensen L, et al. Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy 2008;24:899-908. [Crossref] [PubMed]
- Ichiba A, Kishimoto I. Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg 2009;129:409-15. [Crossref] [PubMed]
- Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med 1999;27:143-56. [Crossref] [PubMed]
- Lohmander LS, Englund PM, et al. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35:1756-69. [Crossref] [PubMed]
- Wasserstein D, Henry P, Paterson JM, et al. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am 2014;96:144-50. [Crossref] [PubMed]
- van Raaij TM, Reijman M, Furlan AD, et al. Total knee arthroplasty after high tibial osteotomy. A systematic review. BMC Musculoskelet Disord 2009;10:88. [Crossref] [PubMed]
- van Raaij T, Reijman M, Brouwer RW, et al. Survival of closing-wedge high tibial osteotomy: good outcome in men with low-grade osteoarthritis after 10-16 years. Acta Orthop 2008;79:230-4. [Crossref] [PubMed]
- Amendola A, Rorabeck CH, Bourne RB, et al. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty 1989;4 Suppl:S11-7. [Crossref] [PubMed]
- Lonner JH, Pedlow FX, Siliski JM. Total knee arthroplasty for post-traumatic arthrosis. J Arthroplasty 1999;14:969-75. [Crossref] [PubMed]
- Julin J, Jämsen E, Puolakka T, et al. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop 2010;81:413-9. [Crossref] [PubMed]
- Diduch DR, Insall JN, Scott WN, et al. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am 1997;79:575-82. [PubMed]
- Gioe TJ, Novak C, Sinner P, et al. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res 2007.83-7. [PubMed]
- Mihelic R, Jurdana H, Jotanovic Z, et al. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17-20 years. Int Orthop 2011;35:1093-7. [Crossref] [PubMed]
- Simon D, Mascarenhas R, Saltzman BM, et al. The Relationship between Anterior Cruciate Ligament Injury and Osteoarthritis of the Knee. Adv Orthop 2015;2015:928301.
- Magnussen RA, Duthon V, Servien E, et al. Anterior Cruciate Ligament Reconstruction and Osteoarthritis: Evidence from Long-Term Follow-Up and Potential Solutions. Cartilage 2013;4:22S-6S. [Crossref] [PubMed]


