
A comparative study of changes in audiological characteristics when using endoscopic and microscopic stapes surgery in patients with otosclerosis
Introduction
Otosclerosis, a progressive disease caused by genetic and inflammatory influences (1,2), develops within the inner ear’s bony labyrinth and is characterized by a pathological bone remodeling that could lead to stapes footplate fixation and progressive conductive hearing loss (HL) (3-5).
Middle ear implants, pharmacological therapies, and stapes surgeries could be considered for treating otosclerosis (5). However, middle ear implants and pharmacological therapies are not widely accepted due to controversial outcomes (6-8). Stapedotomy is currently considered the gold standard surgical treatment for otosclerosis (9). Shiao et al. and Babighian et al. demonstrated significant improvement in average air conduction (AC) and air-bone gap (ABG) (P<0.001) and no difference in bone conduction (BC) after surgery were reported in their cases (10,11). In their study, Roychowdhury et al. reported that low-frequency (LF) AC and ABG improved significantly more after stapedotomy than high-frequency (HF) AC and ABG (12).
Patients usually undergo stapedotomy via microscope. The endoscope was initially introduced as an alternative tool for viewing the middle ear during surgery (5,13). Recent accumulating evidence has demonstrated that endoscopic stapedotomy is feasible and has similar, and often better, audiological outcomes compared with microscopic stapedotomy. For instance, in a meta-analysis report, no statistically significant difference was found in surgery success rates (postoperative ABG ≤10 dB) between endoscopic and microscopic stapedotomy (14), while in another meta-analysis, a change in ABG favoring endoscopic stapedotomy was found (15).
Endoscopic stapedotomy has the advantages of a wide field of view and better visualization of the structures in the middle ear, which leads to reduced rates of removal of the scutum or injury to the chorda tympani, as well as lower pain scores and a lower incidence of dysgeusia in patients (15-17).
The 1-hand technique, heating effects of the endoscope’s light, and lack of stereoscopic view are limitations of endoscopic stapes surgery (ESS) method and can sometimes cause surgical trauma to the chorda tympani and other structures in the middle ear which were supposed to be preserved, such as the malleus and the incus (18-20).
The aim of the present study was to analyze and compare the audiological outcomes (AC, BC, ABG) in different frequencies (LF, MF, and HF) between 2 cohorts of patients with otosclerosis undergoing ESS or microscopic stapes surgery (MSS), and to investigate which of these could be an efficient surgical indicator for future clinical use. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1252/rc).
Methods
Our clinical research design was firstly to search the medical record system and the audiometry system for otosclerosis patients who underwent either ESS or MSS and had complete preoperative and postoperative audiological data and medical records, then to summarize the descriptive data and compare preoperative and postoperative audiological data of ESS and MSS groups.
Participants
The integrity of descriptive and preoperative and postoperative audiological data determined the sample size of this cohort study. Sixty-five otosclerosis patients who underwent either ESS (n=30) or MSS (n=35) between April 2017 and April 2021 at Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, China, were included in the present study. Otosclerosis diagnoses were based on a history of progressive conductive or mixed HL, a mean HL ≥25 dB in the range of 0.25–4 kHz, and normal otoscopic findings. Exclusion criteria were as follows: patients who had had former ear surgeries, malformation of the ossicular chain, any other causes for stapes footplate fixation, and absence of follow up, which reduced the potential bias as much as we could. Among the 65 patients, 5 reported no tinnitus before and after ESS, and 6 patients reported no tinnitus before and after MSS. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Sun Yat-Sen Memorial Hospital (No. SYSEC-KY-KS-2022-120), and informed consent was not required because this was a cohort and retrospective study, and all data were collected after the patients were discharged.
Medical records/clinical factors measurements and audiological measurements
We searched the medical record system for the medical records of diagnosed otosclerosis patients, and we documented the types of surgery they underwent, and their sex, age, side of affected ear, operating side.
Preoperative and postoperative audiological evaluation was carried out using pure-tone audiometry. ABG was calculated for AC minus BC. LF referred to 0.125 and 0.25 kHz; MF referred to 0.5, 1, and 2 kHz; and HF referred to 4 and 8 kHz. Pure-tone average (PTA) referred to 0.5, 1, 2, and 4 kHz.
Auditory gains were calculated from preoperative and postoperative audiograms, and are shown as Δs.
Surgical techniques
All surgeries were performed under general anesthesia. ESS was performed using a 3-mm diameter, 0° rigid endoscope with a high-definition camera and monitor. An incision was made in the posterior external ear canal, then the tympanomeatal flap was lifted. Attachment of the tympanic membrane to the malleus and to the chorda tympani was preserved. Atticotomy was performed for better exposure of the oval window region. After dislocation of the incudostapedial joint, the stapedius tendon and the posterior crus were divided by microscissors. The distance between the long prominence of the incus and footplate was measured, and then a fenestration was created in the footplate by a handheld microperforator. The ideal-sized prosthesis was inserted into the fenestration, and the hook was crimped on the long prominence of the incus. The footplate was sealed by blood. The tympanomeatal flap was then replaced, and the external auditory canal was packed with gelatin foam. MSS was performed similarly to ESS, with the exception of an endaural skin incision being made.
Statistical analyses
Statistical analyses were performed using SPSS version 26.0 (IBM, Armonk, NY, USA). First, we verified that our audiological data of the two groups were normally distributed using normality test. Then, we used independent sample t-tests to compare the preoperative hearing parameters between the groups to verify if the 2 groups could be considered homogeneous so that we could continue with the following statistical analyses. Associations between hearing outcomes and clinical data were analyzed using paired sample t-tests (comparisons of preoperative and postoperative audiological parameters), independent-sample t-tests (comparisons of auditory gains), Mann-Whitney U-tests, and χ2-tests (comparison of surgery success rates) and linear regression tests (associations between preoperative audiological parameters and their changes). Data are expressed as mean, standard deviation of the mean, and percentages. P≤0.05 was considered statistically significant and was two-sided. Bar charts and line graphs were made using SPSS version 26.0 and GraphPad version 9.0, respectively.
Results
Complete audiological data of 65 patients undergoing stapes surgery were collected and analyzed (Table 1). Incomplete descriptive and preoperative and postoperative audiological data were not collected.
Table 1
| Type of surgery | ESS | MSS |
|---|---|---|
| Sex, n (%) | ||
| Female | 20 (66.67) | 25 (71.43) |
| Male | 10 (33.33) | 10 (28.57) |
| Mean age, years | 39.6 | 40.66 |
| Side of affected ear, n (%) | ||
| Right | 5 (16.67) | 7 (20.00) |
| Left | 3 (10.00) | 6 (17.14) |
| Bilateral | 22 (73.33) | 22 (62.86) |
| Operating side, n (%) | ||
| Right | 16 (53.33) | 14 (40.00) |
| Left | 14 (46.67) | 21 (60.00) |
| Bilateral | 0 (0.00) | 0 (0.00) |
ESS, endoscopic stapes surgery; MSS, microscopic stapes surgery.
A total of 30 ESS were performed on 30 patients. Five (16.67%) of these patients had right ear otosclerosis, 3 (10%) had left ear otosclerosis, and 22 (73.33%) had bilateral otosclerosis. Of all 30 ESS patients, 16 (53.33%) underwent surgery on their right ear and 14 (46.67%) underwent surgery on their left ear. Female patients accounted for 66.67% (n=20) of the ESS cohort (10). The mean age of the ESS cohort was 39.6 years.
A total of 35 MSS were performed on 35 patients. Seven (20%) of these patients had right ear otosclerosis, 6 (17.14%) had left ear otosclerosis, and 22 (62.86%) had bilateral otosclerosis. Of all 35 MSS patients, 14 (40%) underwent surgery on their right ear and 21 (60%) underwent surgery on their left ear. Female patients accounted for 71.43% (n=25) of the MSS cohort. The mean age of the MSS cohort was 40.66 years.
Preoperative PTA tests were performed <4 weeks before surgery, whereas postoperative testing was performed from 1 to 14 months (average: 3 months) after surgery, depending on patients’ adherence to surgeons’ instructions that they should go to outpatient for follow-up checks and tests 1 month, 3 months and 6 months each, after surgery.
Table 2 shows the preoperative and postoperative hearing thresholds between the 2 groups. Independent sample comparisons of preoperative hearing parameters (AC-PTA, BC-PTA, ABG-PTA) between the groups showed no significant difference (P>0.05).
Table 2
| Audiological parameter | ESS | MSS | t | P value |
|---|---|---|---|---|
| Preoperative (dB) | ||||
| AC-PTA | 60.21±14.64 | 63.93±15.85 | –0.98 | 0.332 |
| BC-PTA | 29.96±11.51 | 35.04±13.11 | –1.65 | 0.105 |
| ABG-PTA | 29.74±11.16 | 28.89±8.49 | 0.35 | 0.730 |
| Postoperative (dB) | ||||
| AC-PTA | 39.38±12.55 | 42.89±17.89 | –0.90 | 0.370 |
| BC-PTA | 29.38±10.76 | 29.93±12.87 | –0.19 | 0.853 |
| ABG-PTA | 10.67±6.21 | 12.96±9.18 | –1.12 | 0.268 |
Results are shown as mean ± standard deviation. PTA, pure-tone averages; ESS, endoscopic stapes surgery; MSS, microscopic stapes surgery; ABG, air-bone gap; AC, air-conduction; BC, bone-conduction.
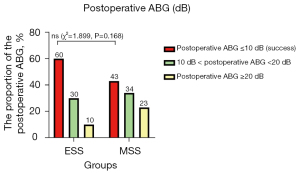
Figure 1 shows the postoperative ABG between the groups. In the ESS group, 18 patients had postoperative ABG ≤10 dB (60%), 9 had postoperative ABG 10–20 dB (30%), and 3 had postoperative ABG >20 dB (10%). In the MSS group, 15 patients had postoperative ABG ≤10 dB (43%), 15 had postoperative ABG 10–20 dB (43%), and 5 had postoperative ABG >20 dB (14%). A 2-independent sample Mann-Whitney U-test demonstrated that there were no significant differences in postoperative ABG between the groups (Z=–1.577, P=0.115). The effective rate, which was defined as the proportion of patients with postoperative ABG ≤10 dB, was 60% in the ESS group and 42.86% in the MSS group; χ2-tests showed there were no significant differences between the groups (χ2=1.899, P=0.168).
Tables 3,4 show the averages of preoperative and postoperative audiological parameters of different frequencies, and the comparative measures of ESS and MSS. In the ESS group, AC-LF (preoperative: 64.08±14.91 dB, postoperative: 33.00±11.07 dB), AC-MF (preoperative: 61.67±14.19 dB, postoperative: 36.67±12.54 dB), AC-PTA (preoperative: 60.21±14.64 dB, postoperative: 39.38±12.55 dB), ABG-LF (preoperative: 51.00±15.61 dB, postoperative: 21.67±11.17 dB), ABG-MF (preoperative: 30.89±11.48 dB, postoperative: 8.22±5.60 dB), ABG-HF (preoperative: 28.33±12.62 dB, postoperative: 18.00±11.93 dB), and ABG-PTA (preoperative: 29.74±11.16 dB, postoperative: 10.76±6.14 dB) significantly decreased after surgery (P<0.05); however, there were no significant differences in terms of AC-HF and BC-LF, BC-MF, BC-HF, and BC-PTA (P>0.05). In the MSS group, AC-LF (preoperative: 6.14±11.41 dB, postoperative: 38.57±17.26 dB), AC-MF (preoperative: 65.00±14.57 dB, postoperative: 40.90±16.75 dB), AC-PTA (preoperative: 63.93±15.85 dB, postoperative: 42.89±17.89 dB), BC-MF (preoperative: 35.67±12.34 dB, postoperative: 29.19±12.08 dB), BC-PTA (preoperative: 35.04±13.11 dB, postoperative: 29.93±12.87 dB), ABG-LF (preoperative: 48.29±10.64 dB, postoperative: 23.57±13.26 dB), ABG-MF (preoperative: 29.33±8.08 dB, postoperative: 11.71±9.20 dB), ABG-HF (preoperative: 27.57±14.87 dB, postoperative: 16.71±12.60 dB), and ABG-PTA (preoperative: 28.89±8.49 dB, postoperative: 12.96±9.18 dB) significantly decreased after surgery (P<0.05); however, there were no significant differences in terms of AC-HF, BC-LF, and BC-HF (P>0.05).
Table 3
| ESS frequency | AC | BC | ABG | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative (dB) | Postoperative (dB) | t | P value | Preoperative (dB) | Postoperative (dB) | t | P value | Preoperative (dB) | Postoperative (dB) | t | P value | |||
| Low frequency | 64.08±14.91 | 33.00±11.07 | 12.52 | 0.000 | 14.83±10.54 | 13.00±10.31 | 0.95 | 0.352 | 51.00±15.61 | 21.67±11.17 | 9.93 | 0.000 | ||
| Mid frequency | 61.67±14.19 | 36.67±12.54 | 10.66 | 0.000 | 30.78±11.23 | 28.89±11.35 | 1.13 | 0.267 | 30.89±11.48 | 8.22±5.60 | 12.42 | 0.000 | ||
| High frequency | 60.00±20.80 | 57.58±19.54 | 0.90 | 0.370 | 27.50±17.65 | 30.83±15.49 | −1.92 | 0.064 | 28.33±12.62 | 18.00±11.93 | 3.43 | 0.002 | ||
| PTA | 60.21±14.64 | 39.38±12.55 | 8.74 | 0.000 | 29.96±11.51 | 29.96±11.51 | 0.40 | 0.692 | 29.74±11.16 | 10.76±6.14 | 9.79 | 0.000 | ||
Results are shown as mean ± standard deviation. PTA, pure-tone averages; ESS, endoscopic stapes surgery; ABG, air-bone gap; AC, air-conduction; BC, bone-conduction.
Table 4
| MSS frequency | AC | BC | ABG | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative (dB) | Postoperative (dB) | t | P value | Preoperative (dB) | Postoperative (dB) | t | P value | Preoperative (dB) | Postoperative (dB) | t | P value | |||
| Low frequency | 66.14±11.41 | 38.57±17.26 | 11.23 | 0.000 | 18.57±8.36 | 15.71±10.86 | 1.64 | 0.110 | 48.29±10.64 | 23.57±13.26 | 10.12 | 0.000 | ||
| Mid frequency | 65.00±14.57 | 40.90±16.75 | 9.89 | 0.000 | 35.67±12.34 | 29.19±12.08 | 3.90 | 0.000 | 29.33±8.08 | 11.71±9.20 | 8.16 | 0.000 | ||
| High frequency | 63.93±21.38 | 59.93±21.77 | 1.21 | 0.235 | 33.14±18.11 | 32.14±18.52 | 0.45 | 0.659 | 27.57±14.87 | 16.71±12.60 | 3.31 | 0.002 | ||
| PTA | 63.93±15.85 | 42.89±17.89 | 8.39 | 0.000 | 35.04±13.11 | 29.93±12.87 | 3.05 | 0.004 | 28.89±8.49 | 12.96±9.18 | 7.39 | 0.000 | ||
Results are shown as mean ± standard deviation. PTA, pure-tone averages; MSS, microscopic stapes surgery; ABG, air-bone gap; AC, air-conduction; BC, bone-conduction.
Table 5 shows the averages of the auditory gains of different frequencies of both groups, and the comparative measures between both types of surgeries. Auditory gain was defined as the difference of value between preoperative and postoperative audiological parameters. There were no significant differences in terms of AC-LF, BC-LF, ABG-LF, AC-MF, BC-MF, ABG-MF, AC-HF, BC-HF, ABG-HF, AC-PTA, and ABG-PTA (P>0.05), but the MSS group demonstrated better results for BC-PTA (P=0.049).
Table 5
| Frequency | Audiological parameter | ESS (dB) | MSS (dB) | t | P value |
|---|---|---|---|---|---|
| Low frequency | AC | 31.08±13.59 | 27.57±14.52 | 1.00 | 0.321 |
| BC | 1.83±10.63 | 2.86±10.31 | –0.39 | 0.695 | |
| ABG | 29.33±16.17 | 24.71±14.45 | 1.22 | 0.229 | |
| Mid frequency | AC | 25.00±12.84 | 24.10±14.42 | 0.27 | 0.792 |
| BC | 1.89±9.15 | 6.48±9.82 | –1.94 | 0.057 | |
| ABG | 22.67±10.00 | 17.62±12.77 | 1.75 | 0.085 | |
| High frequency | AC | 2.42±14.63 | 4.00±19.59 | –0.36 | 0.717 |
| BC | –3.33±9.50 | 1.00±13.27 | –1.49 | 0.141 | |
| ABG | 10.33±16.50 | 10.86±19.42 | –0.12 | 0.908 | |
| PTA | AC | 20.83±13.05 | 21.04±14.84 | –0.06 | 0.954 |
| BC | 0.58±7.98 | 5.11±9.90 | –2.01 | 0.049 | |
| ABG | 18.98±10.62 | 15.93±12.75 | 1.04 | 0.304 |
Results are shown as mean ± standard deviation. PTA, pure-tone averages; ESS, endoscopic stapes surgery; MSS, microscopic stapes surgery; ABG, air-bone gap; AC, air-conduction; BC, bone-conduction.
Table 6 shows the comparative measures of the auditory gains in different frequency ranges for each type of stapes surgery. In the ESS group, for AC, AC-LF improved significantly more than both AC-MF and AC-HF after surgery, and AC-MF improved significantly more than AC-HF (P<0.05). For BC, the auditory gain of BC-MF was significantly higher than that of BC-HF (P<0.05), but there were no significant differences between the auditory gains of BC-LF, BC-MF, BC-LF, and BC-HF (P>0.05). For ABG, the auditory gains of ABG-MF and ABG-LF were significantly higher than that of ABG-HF (P<0.05), but there were no significant differences between the gains of ABG-LF and ABG-MF (P>0.05). In the MSS group, for AC, the auditory gains of AC-MF and AC-LF were significantly higher than that of AC-HF (P<0.05), whereas there were no significant differences between the gains of AC-LF and AC-MF (P>0.05). For BC, there were no significant differences between the auditory gains of BC-LF, BC-MF, and BC-HF (P>0.05). For ABG, the auditory gains of ABG-LF were significantly higher than those of ABG-MF and ABG-HF (P<0.05), and there were no significant differences between the auditory gains of ABG-MF and ABG-HF (P>0.05).
Table 6
| Frequency | ESS | MSS | |||
|---|---|---|---|---|---|
| t | P value | t | P value | ||
| AC | |||||
| LF vs. MF | 1.78 | 0.080 | 1.00 | 0.318 | |
| MF vs. HF | 6.35 | 0.000 | 4.89 | 0.000 | |
| LF vs. HF | 7.86 | 0.000 | 5.72 | 0.000 | |
| BC | |||||
| LF vs. MF | −0.02 | 0.983 | −1.50 | 0.137 | |
| MF vs. HF | 2.17 | 0.034 | 1.68 | 0.098 | |
| LF vs. HF | 1.99 | 0.052 | 0.56 | 0.578 | |
| ABG | |||||
| LF vs. MF | 1.92 | 0.060 | 2.18 | 0.033 | |
| MF vs. HF | 3.5 | 0.001 | 1.72 | 0.090 | |
| LF vs. HF | 4.5 | 0.000 | 3.39 | 0.001 | |
ABG, air-bone gap; AC, air-conduction; BC, bone-conduction; PTA, pure-tone averages; ESS, endoscopic stapes surgery; MSS, microscopic stapes surgery; HF, high frequency; LF, low frequency; MF, mid frequency.
Figure 2 shows that there was 1 negative case in the ESS group and 3 in the MSS group. To be more specific, negative cases referred to those who had ΔABG-PTA ≤0 dB. In both groups, the scattered points show a concentration of 20–40 dB for preoperative ABG. The line graphs and linear relationship show 2 equations—y=0.7833x–4.1116 (R2=0.669, P<0.0001) in the ESS group, and y=1.0436x–14.225 (R2=0.483, P<0.0001) in the MSS group—indicating that ΔABG-PTA is linearly related to preoperative ABG-PTA in both groups (P<0.0001).
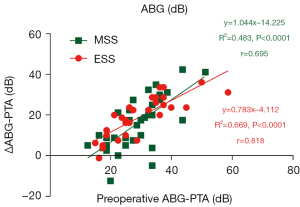
Figure 3 shows that there were 3 negative cases in the ESS group and 1 in the MSS group (ΔAC-PTA ≤0 dB). In both groups, the scattered points show a concentration of 45–80 dB for preoperative AC. The line graphs and linear relationship show 2 equations—y=0.5295x–11.05 (R2=0.3531, P=0.001) in the ESS group, and y=0.301x+1.7943 (R2=0.1034, P=0.060) in the MSS group—indicating that ΔAC-PTA was linearly related to AC-PTA in only the ESS group (P<0.05), but not in the MSS group (P>0.05).
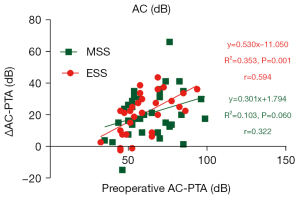
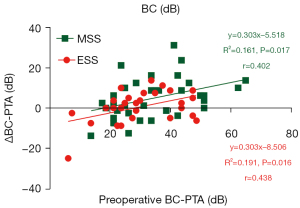
Figure 4 shows that there were 15 negative cases in the ESS group and 12 in the MSS group (ΔBC-PTA ≤0 dB). In both groups, the scattered points show a concentration of 20–50dB for preoperative BC. The line graphs and linear relationship show 2 equations—y=0.3034x–8.5063 (R2=0.1914, P=0.016) in the ESS group, and y=0.3033x–5.5181 (R2=0.1614, P=0.017) in the MSS group—indicating that ΔBC-PTA is linearly related to BC-PTA in both groups (P<0.05).
Discussion
Our analysis of the HL data for the 2 patient cohorts before and after ESS and MSS showed satisfactory and comparatively functional results. There were no significant differences in preoperative hearing between the 2 groups (P>0.05), indicating that the 2 cohorts could be considered homogeneous.
In the evaluation of successful stapes surgery, postoperative ABG <10, 15, 20, and 34.5 dB have been reported and accepted in previous studies, with 10 dB considered the most accepted standard (21-26).
In the present study, a postoperative ABG <10 dB was achieved in 60% of cases in the ESS group and 43% of cases in the MSS group, and there were no significant differences between the groups in terms of effective rates (P=0.168). Daneshi and Jahandideh reported a postoperative ABG <10 dB in 57.9% of cases in the ESS group and in 40% of cases in the MSS group (27), which were similar to our findings. Iannella and Magliulo reported better outcomes; postoperative ABG <10 dB was achieved in 85% of cases in the ESS group and in 80% of cases in the MSS group (28). Although the 6 reports analyzed in Nikolaos et al.’s meta-analysis indicated no significant difference in surgery success rates between ESS and MSS (14), hearing restoration success was the most significant factor in the choice between endoscopy or microscopy in their study.
To explain the wide range of stapes surgery success rates, prosthesis displacement and alterations of the ossicular chain or oval window must be noted as the main causes of failure. Additionally, patients with oval window disturbances presented significantly lower hearing success rates compared with patients with ossicular chain or prosthesis malfunctions (P=0.03, χ2 test) (11).
The statistical significance between preoperative and postoperative averages of AC-PTA, BC-PTA, and ABG-PTA in both groups were reported in the present study. There were no significant differences in either group in terms of postoperative ABG-PTA outcomes (10.67±6.21 vs. 12.96±9.18 dB, P=0.268) and ΔABG-PTA (10.67±6.21 vs. 12.96±9.18 dB, P=0.304). However, in Gulsen and Karatas’s study (24), the ESS group showed a slightly better postoperative ABG-PTA outcome (7.4±4.8 vs. 8.7±3.4 dB), and there was also no significant difference between the groups in terms of hearing gains (P>0.05).
Our findings indicated that AC-LF, AC-MF, AC-PTA, ABG-LF, ABG-MF, ABG-HF, and ABG-PTA significantly decreased after ESS (P<0.05), and AC-LF, AC-MF, AC-PTA, BC-MF, BC-PTA, ABG-LF, ABG-MF, ABG-HF, and ABG-PTA significantly decreased after ESS (P<0.05). Shiao et al. reported similar outcomes (10); the average (0.5, 1, 2, and 3 kHz) AC (from 56.0±13.5 to 40.3±16.4 dB) and ABG (from 28.8±8.8 to 11.3±11.1 dB) significantly decreased after endaural stapes surgery (P<0.001), while the average BC showed no significant deterioration (from 27.5±10.7 to 28.5±11.9 dB, P=0.128). Eighty-six percent of the cases Babighian and Albu’s review demonstrated that the BC threshold remained unchanged after stapes surgery.
Moreover, greater LF and MF auditory gains were shown in both groups in terms of AC and ABG than HF auditory gains. In contrast, auditory gains of BC-MF were significantly greater than the auditory gains of BC-LF and BC-HF in the ESS group (P>0.05). There were no significant differences among BC-LF, BC-MF, and BC-HF in the MSS group. Similarly, Roychowdhury et al. found that ABG-LF improved significantly more than ABG-LF after stapedotomy (12), and presented a simple linear regression model demonstrating that ΔAC (y) decreases as the frequency (x) increases [y=–0.003853x+34.76 (R2=0.951), P<0.001], and indicated that there was no significant difference between preoperative and postoperative thresholds at 8 kHz. One hypothesis could be that the surgical wound is on the vestibular window and HF soundwaves cause vibrations only on the basement membrane around the vestibular window, therefore LF and MF data have better post-stapedotomy outcomes than HF.
In our study, there were no significant differences in terms of the auditory gains (AC-LF, BC-LF, ABG-LF, AC-HF, BC-HF, ABG-HF, AC-PTA, and ABG-PTA) between the groups except for BC-PTA, which slightly favored the MSS group (P=0.049). Likewise, Sproat et al. reported reductions of BC-HF (1, 2, 4 kHz) 6±9 dB in the ESS group and 11±10 dB in the MSS group (29); that reduction was significantly different between the groups, slightly favoring the MSS group.
Taking all hearing outcomes and the comparisons into account, we can conclude that the 2 types of stapedotomies showed similar audiological outcomes. What’s more, for further and more precise investigations of comparisons of audiological outcomes between the 2 types of stapedotomies, Babbage et al. proposed that extended HF (9–16 kHz) data could be more sensitive to compare audiological outcomes between different surgical methods, which could be considered in future clinical applications (30).
Preoperative ABG and AC have been found to be significant prognostic factors for postoperative hearing outcome in otosclerosis patients. Preoperative ABG in particular has been demonstrated to be a significant prognostic factor at multiple frequencies. However, preoperative BC has not demonstrated any influence on postoperative outcomes (31,32).
In their study, Bittermann et al. found that a smaller preoperative ABG (≤30 dB) could lead to a better postoperative ABG (≤10 dB), while a large preoperative ABG (>30 dB) and preoperative AC (>50 dB) could lead to a better AC (>20 dB) (33).
In the present study, we analyzed the statistical association between preoperative ABG-PTA, AC-PTA, BC-PTA, ΔABG-PTA, ΔAC-PTA, and ΔBC-PTA.
In terms of the association between preoperative ABG-PTA and ΔABG-PTA in both groups, we found the concentration of scattered points to be 20–40 dB for preoperative ABG-PTA. In the ESS group, for preoperative ABG-PTA >20 dB, ΔABG-PTA improved more than 10d B, which is considered successful from a surgical perspective. In the MSS group, for preoperative ABG-PTA >25 dB, ΔABG-PTA improved more than 10 dB. Furthermore, we found a greater number of successful cases and less negative values in the ESS group (1 negative case vs. 3). In the ESS group, ΔABG-PTA was linearly related to preoperative ABG-PTA, indicating that preoperative ABG-PTA could explain 66.9% of the change of ΔABG-PTA. In the MSS group, ΔABG-PTA was also linearly related to the preoperative ABG-PTA, indicating that preoperative ABG-PTA could explain 48.3% of the change of ΔABG-PTA.
In terms of the association between preoperative AC-PTA and ΔAC-PTA in both groups, we found the concentration of scattered points to be 45–80 dB for preoperative AC-PTA, as well as a greater number of successful cases and less negative values in the MSS group (3 negative cases vs. 1). In the ESS group, ΔAC-PTA was linearly related to preoperative AC-PTA, indicating that preoperative AC-PTA could explain 35.31% of the change of ΔAC-PTA. However, in the MSS group, ΔAC-PTA was not linearly related to the preoperative AC-PTA (P>0.05).
In terms of the association between preoperative BC-PTA and ΔBC-PTA in both groups, we found the concentration of scattered points to be 20–50 dB for preoperative BC-PTA, as well as a greater number of successful cases and less negative values in the MSS group (15 negative cases vs. 12). In the ESS group, ΔBC-PTA was linearly related to preoperative BC-PTA, indicating that preoperative ABG-PTA could explain 19.14% of the change of ΔBC-PTA. In the MSS group, ΔBC-PTA was also linearly related to the preoperative BC-PTA, indicating that preoperative BC-PTA could explain 16.14% of the change of ΔBC-PTA.
These findings draw a reasonable conclusion that stapedotomy is greatly effective for patients with preoperative ABG-PTA 20–40 dB or preoperative AC-PTA 45–80 dB, and that ESS seems to be the better option. Patients with preoperative ABG-PTA <20 dB or >40 dB and preoperative AC-PTA <45 dB or >80 dB could seek other more suitable approaches, such as a hearing device. We did not discuss the prognostic use of preoperative BC-PTA in the present study due to multiple failed cases in both groups. However, this warrants further investigation for prospective clinical use. Among preoperative ABG-PTA, preoperative AC-PTA, and preoperative BC-PTA, preoperative ABG-PTA was found to be the best indicator for stapes surgery success.
Our study was limited by the small number of samples and the lack of regular and long-term, follow-up audiological data. In the future, we will expand the number of research samples and create a more detailed and statistic plan for descriptive and audiological data collection.
Conclusions
The findings of our study indicate that postoperative audiological outcomes, surgery success rates, and audiological changes between both types of surgeries are comparable, except for changes in BC-PTA, which favored the MSS group. MSS also improved BC-LF and BC-HF. Moreover, shifts in ABG and BC were linearly related to preoperative ABG and BC in both groups, and shifts in AC were linearly related to preoperative AC in the ESS group (P<0.05). Based on linear regression analysis, preoperative ABG-PTA was the most efficient surgical indicator for both types of stapes surgery for patients with otosclerosis. We propose that ESS could be a more effective alternative treatment for HL caused by otosclerosis, and preoperative ABG-PTA could work as a useful clinical indicator for therapeutic choices.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1252/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1252/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1252/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Sun Yat-Sen Memorial Hospital (No. SYSEC-KY-KS-2022-120), and informed consent was not required because this was a cohort and retrospective study, and all data were collected after the patients were discharged.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rudic M, Keogh I, Wagner R, et al. The pathophysiology of otosclerosis: Review of current research. Hear Res 2015;330:51-6. [Crossref] [PubMed]
- Sziklai I, Batta TJ, Karosi T. Otosclerosis: an organ-specific inflammatory disease with sensorineural hearing loss. Eur Arch Otorhinolaryngol 2009;266:1711-8. [Crossref] [PubMed]
- Job K, Wiatr A, Skladzien J, et al. The Audiometric Assessment of the Effectiveness of Surgical Treatment of Otosclerosis Depending on the Preoperative Incidence of Carhart's Notch. Ear Nose Throat J 2021; Epub ahead of print. [Crossref] [PubMed]
- Crompton M, Cadge BA, Ziff JL, et al. The Epidemiology of Otosclerosis in a British Cohort. Otol Neurotol 2019;40:22-30. [Crossref] [PubMed]
- Batson L, Rizzolo D. Otosclerosis: An update on diagnosis and treatment. JAAPA 2017;30:17-22. [Crossref] [PubMed]
- Lippy WH, Berenholz LP. Pearls on otosclerosis and stapedectomy. Ear Nose Throat J 2008;87:326-8. [Crossref] [PubMed]
- Venail F, Lavieille JP, Meller R, et al. New perspectives for middle ear implants: first results in otosclerosis with mixed hearing loss. Laryngoscope 2007;117:552-5. [Crossref] [PubMed]
- Liktor B, Szekanecz Z, Batta TJ, et al. Perspectives of pharmacological treatment in otosclerosis. Eur Arch Otorhinolaryngol 2013;270:793-804. [Crossref] [PubMed]
- Bartel R, Sanz JJ, Clemente I, et al. Endoscopic stapes surgery outcomes and complication rates: a systematic review. Eur Arch Otorhinolaryngol 2021;278:2673-9. [Crossref] [PubMed]
- Shiao AS, Kuo CL, Cheng HL, et al. Controversial issues of optimal surgical timing and patient selection in the treatment planning of otosclerosis. Eur Arch Otorhinolaryngol 2014;271:1007-14. [Crossref] [PubMed]
- Babighian GG, Albu S. Failures in stapedotomy for otosclerosis. Otolaryngol Head Neck Surg 2009;141:395-400. [Crossref] [PubMed]
- Roychowdhury P, Polanik MD, Kempfle JS, et al. Does stapedotomy improve high frequency conductive hearing? Laryngoscope Investig Otolaryngol 2021;6:824-31. [Crossref] [PubMed]
- Marchioni D, Soloperto D, Villari D, et al. Stapes malformations: the contribute of the endoscopy for diagnosis and surgery. Eur Arch Otorhinolaryngol 2016;273:1723-9. [Crossref] [PubMed]
- Nikolaos T, Aikaterini T, Dimitrios D, et al. Does endoscopic stapedotomy increase hearing restoration rates comparing to microscopic? A systematic review and meta-analysis. Eur Arch Otorhinolaryngol 2018;275:2905-13. [Crossref] [PubMed]
- Ho S, Patel P, Ballard D, et al. Chandrasekhar S. Systematic Review and Meta-analysis of Endoscopic vs Microscopic Stapes Surgery for Stapes Fixation. Otolaryngol Head Neck Surg 2021;165:626-35. [Crossref] [PubMed]
- Koukkoullis A, Tóth I, Gede N, et al. Endoscopic versus microscopic stapes surgery outcomes: A meta-analysis and systematic review. Laryngoscope 2020;130:2019-27. [Crossref] [PubMed]
- Toulouie S, Block-Wheeler NR, Rivero A. Postoperative Pain After Endoscopic vs Microscopic Otologic Surgery: A Systematic Review and Meta-analysis. Otolaryngol Head Neck Surg 2021; Epub ahead of print. [Crossref] [PubMed]
- Pauli N, Strömbäck K, Lundman L, et al. Surgical technique in stapedotomy hearing outcome and complications. Laryngoscope 2020;130:790-6. [Crossref] [PubMed]
- Li B, Zhou L, Wang M, et al. Endoscopic versus microscopic surgery for treatment of middle ear cholesteatoma: A systematic review and meta-analysis. Am J Otolaryngol 2021;42:102451. [Crossref] [PubMed]
- Lucidi D, Molinari G, Reale M, et al. Functional Results and Learning Curve of Endoscopic Stapes Surgery: A 10-Year Experience. Laryngoscope 2021;131:885-91. [Crossref] [PubMed]
- Ueda H, Miyazawa T, Asahi K, et al. Factors affecting hearing results after stapes surgery. J Laryngol Otol 1999;113:417-21. [Crossref] [PubMed]
- Rondini-Gilli E, Bozorg Grayeli A, Boutin P, et al. Otosclerosis surgical techniques and results in 150 patients. Ann Otolaryngol Chir Cervicofac 2002;119:227-33. [PubMed]
- Dankuc D, Pejaković N, Komazec Z, et al. Functional hearing results in patients with otosclerosis before and after stapedotomy. Med Pregl 2012;65:54-8. [Crossref] [PubMed]
- Gulsen S, Karatas E. Comparison of surgical and audiological outcomes of endoscopic and microscopic approach in stapes surgery. Pak J Med Sci 2019;35:1387-91. [Crossref] [PubMed]
- Xie J, Zhang LJ, Zeng N, et al. The clinical characteristics of otosclerosis and benefit from stapedotomy: our experience of 48 patients (58 ears). Acta Otolaryngol 2019;139:843-8. [Crossref] [PubMed]
- Deniz B, Ihsan K, Ismail G, et al. Analysis of factors affecting postoperative functional outcome in patients with otosclerosis. Auris Nasus Larynx 2020;47:203-8. [Crossref] [PubMed]
- Daneshi A, Jahandideh H. Totally endoscopic stapes surgery without packing: novel technique bringing most comfort to the patients. Eur Arch Otorhinolaryngol 2016;273:631-4. [Crossref] [PubMed]
- Iannella G, Magliulo G. Endoscopic Versus Microscopic Approach in Stapes Surgery: Are Operative Times and Learning Curve Important for Making the Choice? Otol Neurotol 2016;37:1350-7. [Crossref] [PubMed]
- Sproat R, Yiannakis C, Iyer A. Endoscopic Stapes Surgery: A Comparison With Microscopic Surgery. Otol Neurotol 2017;38:662-6. [Crossref] [PubMed]
- Babbage MJ, O'Beirne GA, Bergin MJ, et al. Patterns of Extended High-frequency Hearing Loss Following Stapes Surgery. Otol Neurotol 2017;38:1405-10. [Crossref] [PubMed]
- Khorsandi A MT, Jalali MM, Shoshi D V. Predictive factors in 995 stapes surgeries for primary otosclerosis. Laryngoscope 2018;128:2403-7. [Crossref] [PubMed]
- Kishimoto M, Ueda H, Uchida Y, et al. Factors affecting postoperative outcome in otosclerosis patients: Predictive role of audiological and clinical features. Auris Nasus Larynx 2015;42:369-73. [Crossref] [PubMed]
- Bittermann AJ, Rovers MM, Tange RA, et al. Primary stapes surgery in patients with otosclerosis: prediction of postoperative outcome. Arch Otolaryngol Head Neck Surg 2011;137:780-4. [Crossref] [PubMed]
(English Language Editor: R. Scott)


