
The feasibility of uterine-vaginal axis MRI-based as evaluation of surgical efficacy in women with pelvic organ prolapse
Introduction
Pelvic organ prolapse (POP) is the most common diseases of the pelvic floor, severely affecting women’s quality of life. The incidence of POP in adult women is approximately 50%, with an 11% lifetime risk of undergoing surgery by age 80 (1,2). Current surgical methods have many limitations, such as unsatisfactory treatment effects, complications, and a high recurrence rate, resulting in reoperation rates of up to 30% (3).
Causes of POP are closely related to damage to the uterine and vaginal supporting structures. Morphological changes in the uterus and vagina lead to the further development of pelvic floor dysfunction, although the pathogenesis of POP is still obscure (4). The current study asserts that POP is closely related to changes in the uterine-vaginal axis, which plays a vital role in maintaining the position and function of pelvic floor organs. Furthermore, changes in the uterine-vaginal axis cause an imbalance of pelvic pressure and supporting force, which eventually lead to the occurrence of POP. However, few studies on the axis and position of the uterus and vagina have been reported. Luo et al. (5) proposed a technique to quantify individual differences in shape, axis, and length of the normal vagina in healthy women. However, comparative studies on quantitative data, such as the shape and position of the uterine-vaginal axis between non-prolapsed, preoperative, and postoperative groups, have not been undertaken. In clinical diagnosis and treatment, surgical efficacy is mainly evaluated by symptoms and physical examination, which lacks objective basis and has certain limitations in the evaluation of surgical efficacy. This adversely affects the evaluation of the efficacy of pelvic floor reconstructive surgery.
Therefore, the current study used MRI sagittal images to compare the angles and coordinate positions of the uterine-vaginal axis associated with the progression of prolapse among subjects in three study groups. Differences in the angle, shape, and position of the uterine-vaginal axis related to POP and pelvic floor reconstruction were observed among the three subject groups. We envisage that the findings of this study will provide an evaluation of curative effects. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1173/rc).
Methods
Patients’ characteristics
A retrospective cohort study was performed on MRI images of patients who were obtained from October, 2019 to February, 2021. All subjects received a clinical examination based on the Pelvic Organ Prolapse Quantification (POP-Q) system. Sagittal MRI images of the case group (before and after surgery) (n=30) and the control group (n=16) were analyzed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The current study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University. All subjects provided written informed consent. The inclusion criteria were as follows: female POP diagnosed by clinical POP-Q stage 2–4 (anterior, apical, or posterior support ≥1 cm below the hymen). All study patients underwent total pelvic floor reconstruction surgery, tension-free vaginal tape obturator (TVT-O) and trans-obturator vaginal tape (TOT) combined with pelvic floor reconstruction surgery. No participants had contraindications for MRI. Healthy volunteers with comparable demographic parameters (age, BMI, parity, menopausal time) were enrolled as the control group. The values of each POP-Q point had to be within the normal range (anterior, apical, or posterior support ≥1 cm above the hymen). An absence of organ prolapse was defined as POP-Q stages 0 and 1. A clinical physical examination and questionnaire surveys were used to exclude pelvic floor dysfunction disease, as symptoms such as urinary incontinence or bowel dysfunction, pelvic floor surgery, pelvic floor deformity, presence of pacemaker, pregnancy, or history of claustrophobia were deemed to be contraindications. Six months after surgery, all participants agreed to a follow-up gynecological examination. MRI was performed by all participants 1 week to 6 months postoperatively.
MRI parameters
All subjects were examined using a supine multi-plane proton density MRI with a 3T superconducting magnet. Participants were requested to void their bladder completely 1 hour preceding the examination and were then required to drink 300 mL of water to adequately fill their bladder 30 minutes before the examination. Patients were placed in the supine position with knees bent and valgus to simulate the lithotomy position. In the resting state, T2-weighted fast recovery, fast spin-echo MRI was performed in the sagittal planes. The parameters obtained included TR/TE 7,564/88, field of view 28 cm, slice thickness 4.0 mm interleaved, slice spacing 0.4 mm, and 32 continuous images.
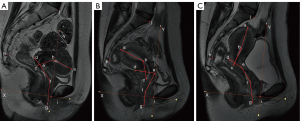
MRI image files were saved in a DICOM (Digital Imaging and Communications in Medicine) format and imported into the medical image processing software, Mimics 19.01 (Materialise Inc., Leuven, Belgium), which displays uterine and vaginal landmarks and contours in the median sagittal position. Two senior radiologists evaluated the MRI sagittal images of subjects, and marks were made on the MRI images after reaching a consensus. A senior urologist also checked the images. The position and shape of the uterine-vaginal axis were marked with seven points in the MRI mid-sagittal plane (Figure 1).
Measurement of the positions and angles of the uterine-vaginal axis
The uterine-vaginal axis was quantified and determined upon obtaining sagittal images of the uterus and vagina in the three study groups. The uterus was divided into the uterus body and cervix, whereas the vagina was divided into upper, middle, and lower segments. The sacro-coccygeal inferior pubic point (SCIPP line) (obtained by connecting a line drawn from the inferior point of the pubic symphysis to the junction between the fifth sacral and first coccygeal bone) was drawn on the median sagittal MRI. The Pelvic Inclination Correction System (PICS) line (X-axis) was established by a 34° clockwise rotation of the SCIPP line. The upper part of the vagina was formed by connecting the apex of the anterior and posterior fornices. The middle and lower vagina sections were divided by the pelvic septum. Each of the uterine and vaginal areas was connected to a straight line. The angles between the uterine and vaginal axes, as well as the angle between the vaginal axis and PICS line, were determined. The PICS line produces an axis system aligned with the bodY-axis (Y-axis) acting on gravity. The Y-axis passed through the inferior point of the pubic symphysis. Bone marker i (the inferior point of the pubic symphysis) was combined with the PICS line (5-7) to create a coordinate system, which provided the same coordinate system to compare the shape and position of the uterine-vaginal axis of each subject. The angles and coordinates of the uterine-vaginal axis were determined using MIMICS software (Figures 1,2).
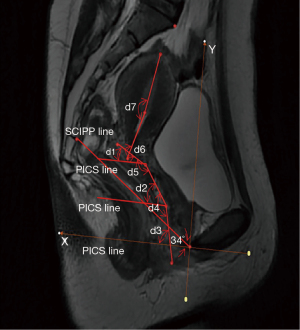
A comparison of the positions and angles of the uterine-vaginal axis among the study subjects was undertaken by creating a coordinate system to quantify the shape of the uterus and vagina, as shown in Figure 1. The OX-axis was created by a 34° clockwise rotation of the SCIPP line. The OY-axis was perpendicular to the X-axis through the inferior point of the pubic symphysis. A corrected coordinate system was used to compare the position and angle of the uterine-vaginal axis of each subject.
Statistical analyses
Demographic information, POP-Q, angle, and coordinate position of the uterine-vaginal axis were recorded. Differences among participants in the three study groups were compared. The Shapiro-Wilk test was used to assess whether variables were normally distributed. The uniformity of variance was determined using homogeneity of variance, and the measurement data were expressed as the mean ± standard deviation (SD). Differences between the control and case (before and after surgery) groups were analyzed using Student’s t-tests and Mann-Whitney U-tests for normally distributed variables and nonparametric independent samples, respectively. Paired t-tests or nonparametric Wilcoxon signed-rank tests were undertaken to determine the differences in the mean values between case groups before and after surgery in the paired samples. Fisher exact test was used to identify differences of POP-Q values before and after surgery (for categoric values). All P values less than 0.05 (P<0.05) were considered statistically significant. All P<0.05 is two-sided. SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis.
Results
Demographic and POP-Q data
The demographic data of all study subjects are displayed in Table 1. No significant differences in age (t=−0.777, P=0.441), body mass index (t=−1.934, P=0.060), vaginal parity (t=−0.671, P=0.506), and menopausal time (t=0.197, P=0.845) were observed among the study subjects. POP-Q classification results differed significantly between the preoperative and postoperative groups (Table 2). Significant improvements were found in the postoperative group compared to the preoperative group, The POP-Q classification of postoperative group restored to normal range 6 months after surgery.
Table 1
| Variables | Control group (mean ± SD) (n=16) | Case group before and after surgery (mean ± SD) (n=30) | P value |
|---|---|---|---|
| Age (y) | 64.31±8.84 | 66.53±9.43 | 0.441* |
| BMI (kg/m2) | 22.34±2.17 | 23.89±2.79 | 0.060* |
| Parity (n) | 2.44±0.96 | 2.70±1.39 | 0.506* |
| Menopausal time (y) | 17.25±9.25 | 16.63±10.54 | 0.845* |
*, independent-sample t-test, where P<0.05 is considered statistically significant. BMI, body mass index; SD, standard deviation.
Table 2
| Variables | Preoperatively (n=30) | Postoperatively (n=30) | P value |
|---|---|---|---|
| Anterior prolapse | 0.001* | ||
| Stage 0 and 1 | 0 (0.0) | 30 (100.0) | |
| Stage 2 | 5 (16.7) | 0 (0.0) | |
| Stage 3 and 4 | 25 (83.3) | 0 (0.0) | |
| Apical prolapse | 0.001* | ||
| Stage 0 and 1 | 2 (6.7) | 30 (100.0) | |
| Stage 2 | 22 (73.3) | 0 (0.0) | |
| Stage 3 and 4 | 6 (20.0) | 0 (0.0) | |
| Posterior prolapse | 0.001* | ||
| Stage 0 and 1 | 0 (0.0) | 30 (100.0) | |
| Stage 2 | 21 (70.0) | 0 (0.0) | |
| Stage 3 and 4 | 9 (30.0) | 0 (0.0) |
*, Fisher’s exact test; P<0.05 is considered statistically significant.
Measurement of the angle of uterus and vagina
The angles of the upper-cervical vagina in the preoperative group were smaller than those in the control and postoperative groups. Statistically significant differences between the control and case groups were observed. However, differences in case groups before and after surgery were not statistically significant. Furthermore, differences in the angles of the uterus body and cervix, angles of the upper and middle vagina, and the upper vaginal-PICS line angles were not statistically significant among the three study groups. Our findings established that the lower vaginal-PICS line angle in the preoperative group was smaller than that of the control and postoperative groups. Notably, the lower vaginal-PICS line angle in the postoperative group was smaller than the angle in the control group. Differences among the three study groups were statistically significant. The middle vaginal-PICS line angle and the middle-lower vaginal angle in the preoperative group were significantly larger than those in the control and postoperative groups. In addition, differences among the three study groups were statistically significant. Therefore, our results demonstrated that the angle of the upper vagina-cervical before and after surgery became smaller due to retroflection of the uterus, which made the uterine-vaginal angle smaller. The lower vaginal-PICS line angle in the case group decreased due to a backward and downward vaginal movement. Moreover, after surgical repair, the lower vaginal-PICS line angle was closer to the angle of the control group subjects than the angle in the case group subjects. The middle vaginal-PICS line and the middle-lower vaginal angles in the preoperative group were greater than the angles in the control group subjects. However, after POP surgery, these angles were noticeably closer to the angle of the control group subjects. Measurements of the uterine and vaginal angles are shown in Table 3.
Table 3
| Variables (degree) | K (mean ± SD) (n=16) | N (mean ± SD) (n=30) | Q (mean ± SD) (n=30) | P | ||
|---|---|---|---|---|---|---|
| K vs. N | K vs. Q | N vs. Q | ||||
| Upper vaginal-PICS line angle | 26.88±10.01 | 29.89±18.49 | 30.01±14.04 | 0.478* | 0.434* | 0.977ω |
| Middle vaginal-PICS line angle | 61.56±9.58 | 78.12±15.03 | 69.35±11.51 | 0.001* | 0.026* | 0.005ω |
| Lower vaginal-PICS line angle | 93.57±10.51 | 77.65±13.61 | 85.88±8.98 | 0.001* | 0.012* | 0.002ω |
| Middle-lower vaginal angle | 147.01±12.20 | 179.30±12.96 | 161.73±10.42 | 0.001* | 0.001* | 0.001ω |
| Upper-middle vaginal angle | 144.79±14.90 | 133.34±22.25 | 140.58±17.28 | 0.072* | 0.414* | 0.069ω |
| Cervix-upper vaginal angle | 252.57±17.74 | 240.31±13.39 | 240.01±15.14 | 0.012* | 0.007# | 0.813Ψ |
| Uterine body-cervix angle | 189.97±46.61 | 185.23±33.04 | 188.66±29.91 | 0.310# | 0.166# | 0.428Ψ |
*, independent-sample t-test; #, Mann-Whitney U test; ω, paired sample t-test; Ψ, Wilcoxon test. P<0.05 is considered statistically significant. K, control group; N, pelvic organ prolapse before surgery; Q, pelvic organ prolapse after surgery; SD, standard deviation; PICS line, Rotating SCIPP line by 34 degrees in the clockwise direction; SCIPP line: obtained by connecting a line drawn from the inferior point of the pubic symphysis to the junction between the fifth sacral and first coccygeal bone.
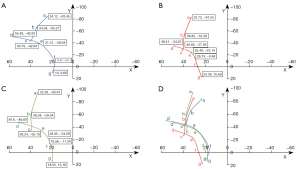
Measurement of coordinate parameters of the position of the uterus and vagina
In the PICS-based coordinate system, the sacral promontory and the junctions between the fifth sacral and first coccygeal bones were not significantly different among subjects in the three study groups. The Y-axis coordinates of the apex of the uterus in the preoperative group were lower than the coordinates in the control and postoperative groups. Statistically significant differences were observed between the control and case groups. The Y-axis coordinates of the endocervical orifice, posterior vaginal fornix, the junction of the middle and lower vagina, and anterior vaginal fornix, as well as the X-axis of the junction of the middle and lower vagina, and the vaginal introitus in the preoperative group were lower compared with the coordinates in the control and postoperative groups. Statistically significant differences were observed between the preoperative and control groups. Statistical differences between the case groups before and after surgery were also significant. However, differences between the control and postoperative groups were not statistically significant. The Y-axes of the external cervical orifice and vaginal introitus in the preoperative group were lower compared with the axes in the control and postoperative groups, and the differences among the three study groups were statistically significant. Our current findings established that the Y-axes of the external cervical orifice and vaginal introitus moved up after POP surgery and were closer to the axes in the control group subjects compared with the axes in the preoperative group. On the other hand, the X-axes of the external cervical orifice, apex of the uterus, internal cervical orifice, posterior vaginal fornix, and anterior vaginal fornix in the three study groups were not significantly different. The coordinate parameters of the uterus and vagina are presented in Table 4.
Table 4
| Variables (mm) | Control group (mean ± SD) (n=16) |
Preoperatively (mean ± SD) (n=30) |
Postoperatively (mean ± SD) (n=30) | P | ||
|---|---|---|---|---|---|---|
| Control group vs. preoperatively | Control group vs. postoperatively | Preoperatively vs. postoperatively | ||||
| a-x value | 24.12±28.34 | 32.72±26.66 | 32.39±20.58 | 0.313* | 0.262* | 0.948ω |
| a-y value | −83.45±14.81 | −81.55±20.73 | −93.33±14.31 | 0.747* | 0.033* | 0.001ω |
| b-x value | 34.04±11.67 | 38.85±12.29 | 38.34±13.18 | 0.447# | 0.279* | 0.894Ψ |
| b-y value | −65.27±7.25 | −52.39±15.63 | −59.04±11.49 | 0.001* | 0.056* | 0.027ω |
| c-x value | 40.79±8.26 | 40.66±10.08 | 38.24±9.71 | 0.966* | 0.378* | 0.262ω |
| c-y value | −42.64±5.76 | −27.09±14.28 | −35.19±9.59 | 0.001* | 0.007* | 0.005ω |
| d-x value | 56.49±14.86 | 48.41±9.63 | 49.90±10.50 | 0.053# | 0.289# | 0.508ω |
| d-y value | −49.93±8.02 | −34.25±13.30 | −46.69±11.09 | 0.001* | 0.309* | 0.001ω |
| e-x value | 31.31±7.70 | 32.49±9.43 | 28.85±9.21 | 0.670* | 0.367* | 0.073ω |
| e-y value | −38.64±6.48 | −23.14±13.71 | −34.68±9.07 | 0.001* | 0.129* | 0.001ω |
| f-x value | 17.67±5.81 | 26.79±6.71 | 19.56±5.24 | 0.001* | 0.268* | 0.001ω |
| f-y value | −10.11±9.77 | −0.48±8.65 | −11.34±7.33 | 0.001*# | 0.631* | 0.001ωΨ |
| g-x value | 19.00±4.55 | 23.39±7.12 | 18.55±4.22 | 0.014*# | 0.504# | 0.001ωΨ |
| g-y value | 9.66±4.00 | 16.69±10.24 | 13.18±4.78 | 0.018*# | 0.040*# | 0.045ωΨ |
*, independent-sample t-test; #, Mann-Whitney U test; ω, paired sample t-test; Ψ, Wilcoxon test. P<0.05 is considered statistically significant. a: apex of the uterus; b: internal orifice of the cervix; c: external orifice of the cervix; d: posterior vaginal fornix; e: anterior vaginal fornix; f: the junction of the middle and lower vagina; g: vaginal introitus. x value: X-axis coordinate value; y value: Y-axis coordinate value. SD, standard deviation.
In the coordinate system, descriptive statistics of the average coordinate parameters of the uterus and vagina based on the PICS coordinate system are shown in Figure 3. The findings of the current study demonstrated that the uterine-vaginal axis in the preoperative group moved backward and downward relative to the control group subjects, and the uterine-vaginal axis moved forward and upward after POP surgery, which more closely resembled the uterine-vaginal axis in the control group subjects.
Discussion
In the early stage of this study, it showed that the vaginal axis of patients before POP surgery was different from healthy women. These changes are not easy to study by gynecological examination because colposcopy will straighten the vagina and affect the evaluation of the vaginal axis and the vaginal angle (8). In addition, the uterine-vaginal axes of the corpse and living body are markedly different. Therefore, this study attempted to use indirect methods to assess the shape and position of the uterine-vaginal axis of the human body. Currently, magnetic resonance imaging (MRI) has shown success in evaluating pelvic structure, especially the soft tissue of the pelvic floor. By revealing the boundary of the uterus and vagina, MRI can accurately measure the position of the uterus and vagina and does not distort their axis and angle during inspection (3). Therefore, pelvic floor MRI is useful in studying the structure of pelvic floor organs of living women. Furthermore, dynamic MRI is useful for observing and studying relationships between internal pelvic organs and response to abdominal pressure.
The uterine-vaginal axis plays an essential role in maintaining the normal shape and position of the pelvic floor organs. Restoration of the uterine-vaginal axis is the hallmark of pelvic floor reconstructive surgery. Studies have shown that there is almost no difference in the position and angle of the vagina of healthy women in different body positions (8). Changes in vaginal morphology predict the degree of prolapse and indicate the type of POP (9). Huebner et al. (10) showed a significant positive correlation between distortion of the vaginal structure and an abnormal decline of pelvic organs. Conventional pelvic MRI shows distortion of vaginal morphology, which may indicate pelvic floor dysfunction (11). A standardized PICS system has been developed by Betschart and colleagues (12). PICS is an advanced standardized system to interpret pelvic MRIs, and previous study (5) has reported on the anatomy of the vagina using MRI. A retrospective study by Luo et al. (5) of 80 women with normal pelvic support established the average axis of the vaginal axis relative to the PICS line. Barnhart et al. (8) used MRI technology to study the vaginal anatomy of 28 healthy women and found that the vagina is divided into two parts, the lower part shows a vertical direction from the vaginal orifice to the pelvic diaphragm, and the upper part shows a more horizontal direction from the pelvic diaphragm to the cervix. The current study established that women with POP had a straighter axis with blunt angles in different parts of the vagina compared with postoperative and control group women, which is consistent with the findings of predictive quantity result in the early stage of this study. Notably, the uterine-vaginal axis was tilted backward and turned forward. Changes in the uterine-vaginal axis occur in POP patients, which cause a biomechanical imbalance of the pelvic floor. This ultimately leads to changes in the uterine-vaginal axis due to gravity as a result of pressure from the abdominal cavity, thereby aggravating prolapse or causing rapid progression from early asymptomatic prolapse to symptomatic prolapse.
The current study’s findings showed that the uterus demonstrated retroversion and flexion in prolapse patients, and the vaginal axis was straightened and turned forward. Lee et al. (13) studied the vaginal axis of women with an intact uterus and after hysterectomy, where significant differences between the two groups were observed. Notably, in the hysterectomy group, the middle part of the vagina was tilted forward, and the angle among the various parts of the vagina increased. In other studies, Luo et al. (5) confirmed that the angle between the upper and middle vaginal in the normal vagina was about 149 degrees. Moreover, the upper part of the vagina is pressed to a position close to horizontal when the abdominal pressure increases, without changing the shape of the vagina. A further study by Ginath et al. (14) using MRI images established that the angle between the vagina and PCL line were significantly different amongst women with and without prolapse. Changes in axis, angle, and position of the uterus and vagina in prolapse patients make the pelvic floor fragile and unable to withstand abdominal pressure under the action of gravity (15). The current study compared the measurements of the uterine-vaginal axis of normal women and prolapse women (before and after surgery). Notably, the uterus of prolapsed patients tilted backward towards the sacrum, and the uterine-vaginal axis moved back and down. Angles between the various parts of the vagina were enlarged. The uterine-vaginal axis of the postoperative case group subjects was close to that of the control group subjects. In addition, the angle between the various parts of the vagina became smaller, indicating that the biomechanical balance of the pelvic floor was restored after surgery.
Vaginal reconstruction surgery is the restoration of defective vaginal anatomy to its original anatomical position. Correct anatomical repair is essential in pelvic floor reconstructive surgery. However, surgery that displaces the vagina from its anatomical position can lead to compensatory abnormalities in women (16). Previous study (17) has indicated that hysterectomy may increase the incidence of postoperative intestinal bulge. The posterior surface of the upper vagina is exposed to the abdominal cavity after the hysterectomy, which may eventually lead to an intestinal bulge as the pressure in the colon increases. Restoring the relationship between ligaments and the apex of the fornix during hysterectomy and maintaining a normal axial angle of the vagina is important in preventing vaginal fornix prolapse after hysterectomy. Burch surgery is believed to induce changes in the vaginal axis, which may destroy the protection of the vaginal fornix, resulting in the formation of intestinal bulges in the future. Previous study (18) has reported that the incidence of intestinal bulge and rectal protrusion increases after Burch suspension. Senturk et al. (19) suggest that bilateral abdominal sacral uterus fixation (imitating the uterosacral ligament) restores the vagina to its original anatomical position compared with classic abdominal sacral uterus fixation, ultimately improving the functional result. Previous study (19) shows that the best anatomical support of the vagina allows for the improvement of urinary symptoms. After pelvic floor reconstruction, the restored shape of the uterine-vaginal axis further reduces the risk of recurrent postoperative prolapse and associated complications (17,20,21). Pelvic floor reconstruction surgery that aims to restore the uterine-vaginal axis to a normal, or close to normal, level is more likely to be successful. The current comparative study on the morphology and angle of the uterine-vaginal axis in the control and case groups demonstrated that women who had undergone pelvic floor reconstruction surgery had a uterine-vaginal axis that more closely resembled that of the control group subjects. This relieves pelvic floor symptoms and reduces complications, indicating its value in the evaluation of the efficacy of pelvic floor reconstruction surgery.
Maintenance of the uterine-vaginal shape depends on the support of the uterine paravaginal structure and the mechanical balance under pressure of the abdominal cavity. Damage to the supporting structures and an increase in abdominal pressure may lead to the destruction of the biomechanical balance of the pelvic floor structure, which changes the uterine-vaginal axis, position, and shape accordingly (4,22). Regarding biomechanical balance, the current study postulates a possible POP mechanism. The mechanical action of the normal pelvic floor support structure converts gravity and abdominal pressure of the pelvic tissue into a horizontal force directed to the sacrococcyx, which maintains a dynamic balance in the supporting function of the pelvic floor organs. This dynamic balance in the supporting function of the pelvic floor organs maintains a normal uterine-vaginal axis by supporting the pelvic floor ligaments, fascia, and muscle tissue. The balance resists gravity and pressure in the pelvic cavity to maintain the biomechanical balance of the pelvic floor. Damage to the support structure of the pelvic floor or changes in the direction of the biomechanics causes pelvic floor dysfunction.
The current study has some limitations. Firstly, MRI scans of the study subjects were undertaken in the supine position, which may have reduced the influence of gravity on the pelvic floor structure. Secondly, the current study did not compare uterine and vaginal shapes of patients with different degrees and types of prolapse before and after surgery. The current study established a two-dimensional coordinate system based on two-dimensional MRI images without performing three-dimensional reconstruction. Three-dimensional structures of the uterus and vagina are more complex than the two-dimensional structures used in the current study. In addition, the high cost of MRI resulted in a small sample size in this study. Future studies would benefit from an increased sample size and three-dimensional reconstruction of the pelvic floor organs to advance relevant analysis and research of this topic. However, this study analyzed the shape, position, and angle of the uterine-vaginal axis in two dimensions. Therefore, we envisage that the current study provides an improved understanding of the critical role of the uterine-vaginal axis in maintaining biomechanical balance and further enhances our knowledge of the mechanism of pelvic floor prolapse.
Conclusions
The current study established that the uterine-vaginal axis of patients with prolapse changed to a more forward-inclined direction. An increase of intra-abdominal pressure leads to changes in the mechanical action direction of the uterine-vaginal axis, indicating that stress on the pelvic floor is no longer carried by the sacrococcyx and levator ani muscle but is directed through the vaginal wall towards the perineum and vaginal introitus, which is more likely to lead to POP. Therefore, pelvic floor reconstruction that can restore the uterine-vaginal axis to its normal physiological state is more likely to succeed. So, the uterine-vaginal axis may be a potential surgical efficacy assessment in the treatment of POP.
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China (Grant Nos. 81802548, 81860451, 81960133); the Yunnan Natural Science Foundation (Grant No. 202001AW070001); the Yunnan Health Training Project of High-Level Talents (Grant No. H2018070); and the Provincial Natural Science Foundation of Yunnan-Kunming Medical University Joint Foundation [Grant Nos. 2019FE001(-136), 2019FE001(-005), 202001AY070001-158].
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1173/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1173/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1173/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The current study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University. All subjects provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fialkow MF, Newton KM, Lentz GM, et al. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:437-40. [Crossref] [PubMed]
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2013;CD004014. [PubMed]
- Juliato CRT, Santos-Junior LC, de Castro EB, et al. Vaginal axis after abdominal sacrocolpopexy versus vaginal sacrospinous fixation-a randomized trial. Neurourol Urodyn 2019;38:1142-51. [Crossref] [PubMed]
- Qiu Z, Song Y. A Hypothesis Generating the Mechanical Systems Underlying Posterior Vaginal Prolapse Based on Observed Displacements by Dynamic Magnetic Resonance Imaging. Female Pelvic Med Reconstr Surg 2020;26:585-90. [Crossref] [PubMed]
- Luo J, Betschart C, Ashton-Miller JA, et al. Quantitative analyses of variability in normal vaginal shape and dimension on MR images. Int Urogynecol J 2016;27:1087-95. [Crossref] [PubMed]
- Reiner CS, Williamson T, Winklehner T, et al. The 3D Pelvic Inclination Correction System (PICS): A universally applicable coordinate system for isovolumetric imaging measurements, tested in women with pelvic organ prolapse (POP). Comput Med Imaging Graph 2017;59:28-37. [Crossref] [PubMed]
- Sinex DCE, Bowen ST, Kashkoush A, et al. The establishment of a 3D anatomical coordinate system for defining vaginal axis and spatial position. Comput Methods Programs Biomed 2021;208:106175. [Crossref] [PubMed]
- Barnhart KT, Izquierdo A, Pretorius ES, et al. Baseline dimensions of the human vagina. Hum Reprod 2006;21:1618-22. [Crossref] [PubMed]
- Hsu Y, Chen L, Delancey JO, et al. Vaginal thickness, cross-sectional area, and perimeter in women with and those without prolapse. Obstet Gynecol 2005;105:1012-7. [Crossref] [PubMed]
- Huebner M, Margulies RU, DeLancey JO. Pelvic architectural distortion is associated with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:863-7. [Crossref] [PubMed]
- Tillack AA, Joe BN, Yeh BM, et al. Vaginal shape at resting pelvic MRI: predictor of pelvic floor weakness? Clin Imaging 2015;39:285-8. [Crossref] [PubMed]
- Betschart C, Chen L, Ashton-Miller JA, et al. On pelvic reference lines and the MR evaluation of genital prolapse: a proposal for standardization using the Pelvic Inclination Correction System. Int Urogynecol J 2013;24:1421-8. [Crossref] [PubMed]
- Lee DD, Siegelman ES, Chua WY, et al. Comparison of Vaginal Axis in Women Who Have Undergone Hysterectomy Versus Women With an Intact Uterus. Female Pelvic Med Reconstr Surg 2019;25:313-7. [Crossref] [PubMed]
- Ginath S, Garely A, Luchs JS, et al. MRI pelvic landmark angles in the assessment of apical pelvic organ prolapse. Arch Gynecol Obstet 2011;284:365-70. [Crossref] [PubMed]
- Fidan U, Keskin U, Ulubay M, et al. Value of vaginal cervical position in estimating uterine anatomy. Clin Anat 2017;30:404-8. [Crossref] [PubMed]
- Siegmann KC, Reisenauer C, Speck S, et al. Dynamic magnetic resonance imaging for assessment of minimally invasive pelvic floor reconstruction with polypropylene implant. Eur J Radiol 2011;80:182-7. [Crossref] [PubMed]
- Balgobin S, Good MM, Dillon SJ, et al. Lowest colpopexy sacral fixation point alters vaginal axis and cul-de-sac depth. Am J Obstet Gynecol 2013;208:488.e1-6. [Crossref] [PubMed]
- Holdø B, Verelst M, Svenningsen R, et al. Long-term clinical outcomes with the retropubic tension-free vaginal tape (TVT) procedure compared to Burch colposuspension for correcting stress urinary incontinence (SUI). Int Urogynecol J 2017;28:1739-46. [Crossref] [PubMed]
- Senturk MB, Kilicci C, Aydin S, et al. Vaginal axis on MRI after unilateral and bilateral sacral hysteropexy: a controlled study. J Obstet Gynaecol 2018;38:115-20. [Crossref] [PubMed]
- Sze EH, Meranus J, Kohli N, et al. Vaginal configuration on MRI after abdominal sacrocolpopexy and sacrospinous ligament suspension. Int Urogynecol J Pelvic Floor Dysfunct 2001;12:375-9; discussion 379-80. [Crossref] [PubMed]
- Pulatoğlu Ç, Yassa M, Turan G, et al. Vaginal axis on MRI after laparoscopic lateral mesh suspension surgery: a controlled study. Int Urogynecol J 2021;32:851-8. [Crossref] [PubMed]
- Pannu HK. Dynamic MR imaging of female organ prolapse. Radiol Clin North Am 2003;41:409-23. [Crossref] [PubMed]
(English Language Editor: D. Fitzgerald)


