
Therapeutic efficacy analysis of distal tibia varus syndrome with different classification and different therapy: a cross-sectional study
Introduction
Ankle impingement, including soft-tissue impingement and osseous impingement, often occurs at the anterior, lateral, and posterior portions of the ankle joints (1-6). Soft-tissue impingement can be induced by soft-tissue reactive proliferation around the tibiotalar or talofibular joints. Ankle impingement syndrome can be caused by ankle sprains, the plantarflexion mechanism of injury, slight repetitive injuries, or other peroneal diseases, such as tendonitis, tenosynovitis, tendon subluxation, and synovitis (1). Anterior arthroscopic and posterior endoscopic treatments have achieved good results with minimal complications and low recurrence rates (1-4). Osseous impingement often occurs in cases of severe valgus hindfoot, such as severe flatfoot (7,8) and old calcaneal fractures (9-11). Lateralizing calcaneal osteotomy to correct the hindfoot alignment achieves the desired effects (10-12).
In our clinical practice, we have treated many patients without symptoms or signs of flatfoot or calcaneal fractures, who complain of weight-bearing subfibular pain. Most of these patients were quinquagenarian, and their symptoms were often induced by an ankle sprain, synovial hyperplasia around the tarsal sinus, or had no obvious cause. Initially, the medial displacement calcaneal osteotomy was tried to treat lateral malleolus impingement. Although the symptoms were relieved, we found that osteochondral lesions of talus (OLT) gradually appeared in some patients. At this time, we realized that these patients had varus deformity of the distal tibia. Conversely, calcaneal osteotomy aggravated the varus alignment of the hindfoot, which was obviously the key inducement of OLT. In theory, lateral ankle impingement could be caused by a narrowing of the osseous gap between the lateral malleolus and calcaneal wall, regardless of valgus hindfoot or varus tibia. From the perspective of epidemiology, oriental people are more prone to varus deformity of distal tibia due to their living habits, which has attracted our attention to the diagnosis, classification and treatment of the disease.
The radiographic characteristics of the above-mentioned patients are as follows: (I) a varus surface of distal tibia; (II) the relative extension and medial translocation of the fibula; (III) congruent ankle mortise; and (IV) normal or slight compensatory valgus calcaneal alignment without flatfoot. To date, no research appears to have been conducted on this kind of impingement syndrome caused by the varus alignment of the distal tibia. Thus, we named it distal tibia varus syndrome (DTVS). The purpose of this retrospective study was to summarize the similarity and specialty of these cases, and propose a diagnosis and classification system for distal tibia varus syndrome based primarily on the clinical symptoms and secondarily on the imaging manifestations. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-997/rc).
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Ruijin Hospital [No. 75 (2013)] and informed consent was taken from all the patients. A case series of patients with lateral ankle impingement syndrome examined at our hospital between January 2010 and December 2018 were included in this retrospective study. To be eligible for inclusion in this study, patients had to meet the following inclusion criteria: (I) show varus alignment of the distal tibia and congruent ankle mortise on the lower extremity radiographs; (II) have normal or slight valgus calcaneal alignment; (III) display no apparent ankle degeneration; and (IV) have subfibular pain that may worsen with weight-bearing or vigorous activities. Patients were excluded if they met any of the following exclusion criteria: (I) had a history of fracture or had undergone an operation on their foot and ankle; (II) had severe trauma or deformity of the foot and ankle; (III) had rheumatism or other systemic inflammatory disease around the ankle joint; and/or (IV) were lost during the follow-up period. The treatment strategies mainly depend on the patient’s symptoms and imaging manifestations.
Evaluations
Patients’ subjective complaints and clinical function were evaluated using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) (13) scores, the American Orthopedic Foot and Ankle Society (AOFAS) rating system ankle-hindfoot scores (14), and the Visual Analogue Scale (VAS) scores. The physical examination focused on pain in the ankle and hindfoot. Weight-bearing anteroposterior and Mortise’s ankle radiographs and ankle magnetic resonance imaging (MRI) scans were performed at the first visit. The following parameters on the radiographs measured by our hospital’s picture archiving and communication system UniWeb Viewer 6.1 (EBM Co., Ltd.) software (13) were assessed: the distal tibial anterior surface angle (TAS); and the distal tibial tilt angle (TTA). The authors jointly performed the clinical examinations and analyzed the radiological data. Each diagnosis was established based on the clinical examination and radiographs. Afterwards, summarizing all the symptoms, measured data, and MRI manifestations, we developed a classification system, and compared the relationship and differences among all patients. Based on the clinical symptoms and image changes, all patients received relevant treatments.
Statistical analysis
All the data are presented as the mean ± standard deviation. First, the global null hypothesis (i.e., that there were no differences between the 3 types of subfibular impingement) was tested using analysis of variance tests for the SF-36 scores, AOFAS ankle-hindfoot scores, and VAS scores, and the TAS and TTA data. If the level of significance was not reached, the parameter examined was excluded from the local tests. The local tests were then performed using the Kruskal-Wallis test to identify significant differences between the 3 types (15). Additionally, the t-test was used to compare the results before and after treatment. The level of statistical significance was set at P<0.05. All statistical tests were two-sided. All the statistical analyses were performed using SPSS software (IBM SPSS Statistics for Windows, Version 19.0; IBM Corp., Armonk, NY, USA).
Results
In total, 76 patients (43 female and 33 male) were included in the study. The patients had a mean age of 46 years (range, 28−68 years) at the time of examination. Patients had a mean body mass index (BMI) of about 25.5 kg/m2. The average course of disease was about 18 months (Table 1). In total, 51 (67%) of the patients, who included peasants, teachers, laborers, cooks, surgeons, and soldiers, had to stand for long periods at work. Among the other patients, 20 (26%) engaged in sedentary behaviors at work, and these patients included office staff and drivers. The other (7%) patients were sports enthusiasts (Table 2).
Table 1
| Scores | All types | Type I | Type II | Type III |
|---|---|---|---|---|
| Number of cases (%) | 76 (100) | 26 (34) | 22 (30) | 28 (37) |
| Gender (female), n (%) | 43 (57) | 16 (62) | 13 (59) | 14 (50) |
| Mean age (years) | 46 | 44 | 47 | 49 |
| BMI (kg/m2) | 25.5±2.9 | 23.1±2.5 | 26.3±2.0 | 27.2±2.0 |
| Course of disease (months) | 18±18 | 5±4 | 19±16 | 28±20 |
BMI, body mass index.
Table 2
| Occupation | Number | Ratio |
|---|---|---|
| Office staff | 16 | 21% |
| Peasant | 16 | 21% |
| Teacher | 14 | 18% |
| Laborer | 9 | 12% |
| Cook | 8 | 11% |
| Driver | 4 | 5% |
| Surgeon | 2 | 3% |
| Soldier | 2 | 3% |
| Other sports enthusiast | 5 | 7% |
Based on the patients’ clinical symptoms and imaging findings, the diagnosis of distal tibia varus syndrome was confirmed, and 3 different types were discerned (Types I, II and III). The scoring system and angle measurements before and after treatment, and the distribution of each type are set out in Table 3. The characteristic clinical symptoms and ankle morphologies shown on the X-ray and MRI images were identified for each type.
Table 3
| Scores | Before | After | t | P |
|---|---|---|---|---|
| All patients | ||||
| SF-36 (points) | 74.14±12.50 | 85.22±8.83 | −17.31 | <0.01 |
| AOFAS (points) | 71.14±15.19 | 87.53±8.62 | −12.26 | <0.01 |
| VAS (points) | 5.41±1.10 | 1.82±1.08 | 23.94 | <0.01 |
| TAS (degrees) | 80.38±4.80 | 90.44±3.96 | −23.51 | <0.01 |
| TTA (degrees) | 13.02±3.41 | 0.62±2.67 | 25.96 | <0.01 |
| Type I | ||||
| SF-36 (points) | 81.92±5.68 | 91.87±3.64 | −11.89 | <0.01 |
| AOFAS (points) | 87.31±2.35 | 94.42±4.70 | −7.35 | <0.01 |
| VAS (points) | 5.07±1.13 | 1.27±1.08 | 11.95 | <0.01 |
| TAS (degrees) | 80.87±4.97 | − | − | − |
| TTA (degrees) | 12.88±3.69 | − | − | − |
| Type II | ||||
| SF-36 (points) | 74.96±10.16 | 85.67±6.50 | −9.09 | <0.01 |
| AOFAS (points) | 65.77±10.72 | 82.72±7.77 | −7.35 | <0.01 |
| VAS (points) | 5.09±0.81 | 1.82±1.05 | 12.77 | <0.01 |
| TAS (degrees) | 80.01±4.73 | 90.12±4.55 | −16.81 | <0.01 |
| TTA (degrees) | 13.07±3.57 | 0.78±2.31 | 14.61 | <0.01 |
| Type III | ||||
| SF-36 (points) | 66.26±14.16 | 78.69±9.18 | −10.06 | <0.01 |
| AOFAS (points) | 60.36±12.28 | 84.89±8.22 | −12.28 | <0.01 |
| VAS (points) | 5.96±1.07 | 2.32±0.86 | 18.79 | <0.01 |
| TAS (degrees) | 80.22±4.83 | 90.70±3.50 | −16.56 | <0.01 |
| TTA (degrees) | 13.11±3.14 | 0.49±2.95 | 22.51 | <0.01 |
SF-36, 36-Item Short-Form Health Survey; AOFAS, American Orthopedic Foot and Ankle Society; VAS, Visual Analogue Scale; TAS, tibial anterior surface angle; TTA, tibial tilt angle.
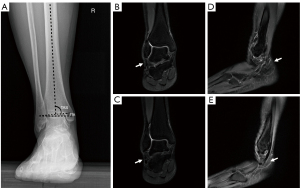
Type I: non-reactive type
In total, 26 patients (10 male and 16 female) with an average age of 44 years (range, 28−68 years), an average disease course of 5 months, and an average mean follow-up period of 14 months were included in the study. An ankle sprain or slight injury was the cause of the symptoms in 22 of the patients, but there was no obvious cause for 4 patients. Type I patients had an average BMI of 23.1±2.5 kg/m2. The main clinical symptom of Type I patients was intermittent pain inferior to the lateral malleolus or lateral to the calcaneus under long-time load and motion, without complete relief at rest. Tenderness inferior to the lateral malleolus was observable, and became worse following passive valgus motion in 6 patients. The varus mid-diaphyseal axes of the tibia could be observed on the weight-bearing anteroposterior ankle radiographs. The measurements of the TAS and TTA were 80.87°±4.97°and 12.88°±3.69°, respectively. No abnormal manifestations were observed in the MRI images (Figure 1). All Type I patients were outpatients, with SF-36 81.92±5.68 scores, AOFAS 87.31±2.35 scores, and VAS 5.07±1.13 scores. The patients were advised to wear sports shoes or arch support cushions. Local pain was relieved effectively by oral non-steroidal anti-inflammatory drugs (NSAIDs) or local glucocorticoid injections. At the last visit, the SF-36 and AOFAS scores increased to 91.87±3.64 and 94.42±4.70, respectively and the VAS scores decreased to 1.27±1.08 (P<0.01).
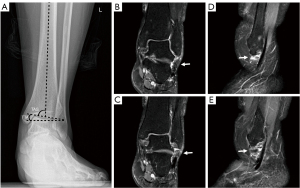
Type II: proliferative type
In total, 22 patients (9 male and 13 female) with an average age of 47 years (range, 28−65 years), an average disease course of 19 months, and an average follow-up period of 29 months were included in the study. Three patients of Type II developed from Type I. Type II patients had an average BMI of 26.3±2.0 kg/m2. The main clinical symptom of the Type II patients was the same as that of the Type I patients. The varus mid-diaphyseal axes of the tibia were displayed on the anteroposterior ankle weight-bearing radiographs with a TAS of 80.01°±4.73° and a TTA of 13.07°±3.57°. Additionally, soft-tissue edema around the peroneal tendons lateral to the calcaneus was visible on the fat-suppression sequences of the T2-weighted images (Figure 2). Type II patients were cured by surgical treatments. A supramalleolar valgus osteotomy to correct the tibial alignment acted as an excellent alternative to Type II patients. The TAS returned to 90.12°±4.55° and the TTA decreased to 0.78°±2.31°after the surgery. The SF-36, AOFAS, and VAS scores changed significantly from 74.96±10.16, 65.77±10.72, and 5.09±0.81 preoperatively to 85.67±6.50, 82.72±7.77, and 1.82±1.05 postoperatively, respectively (P<0.01).
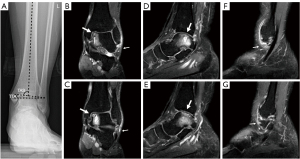
Type III: osteochondral lesion type
In total, 28 patients (14 male and 14 female) with an average age of 49 years (range, 32−65 years), an average disease course of 28 months, and an average follow-up period of 29 months were included in the study. In 20 patients, the cause was an ankle sprain or another slight injury. While, in the other 8 patients, the cause was unclear. Type III patients had an average BMI of 27.2±2.0 kg/m2. The symptoms of the Type III patients were worse than those of the Types I and II patients due to the pain at the anteromedial aspect of the ankle joint and the inferior aspect of the lateral malleolus that occurred after walking or exercising for a long period. Tenderness and edema at the medial and lateral sides of the ankle joint were easily examinable, and worsened following passive motion. As in the Types I and II, the distal tibial surface showed apparent varus inclination with a TAS of 80.22°±4.83°, and a TTA of 13.11°±3.14° on the ankle weight-bearing radiographs.
Additionally, medial osteochondral lesions of the talus (OLT) (1 case at the lateral aspect) more than soft-tissue edema at the lateral region of ankle joints were observed on the MRI images (Figure 3). A supramalleolar opening wedge osteotomy was performed in all patients with tibial tilt alignment (16-19). Due to the severity of the OLT, 18 patients also underwent talar microfracture surgery, while the others underwent osteochondral autograft transplantation (20-22). As a result, the SF-36 and AOFAS scores increased from 66.26±14.16 and 60.36±12.28 preoperatively to 78.69±9.18 and 84.89±8.22 postoperatively, respectively (P<0.05). The postoperative VAS assessment (2.32±0.86) score was significantly lower than the preoperative the VAS assessment (5.96±1.07) score (P<0.05). Following the supramalleolar open osteotomy, the TAS and the TTA returned to a normal size (90.70±3.50 and 0.49±2.95, respectively).
Comparison of the 3 types
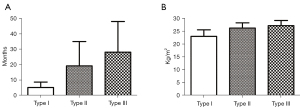
The comparison results of the 3 types in terms of the general demography, scoring system, and angle measurement are shown in Table 4. No significant difference was found in terms of age across the different types (P>0.05). Type I patients had a slightly lower BMI than Types II and III patient (P<0.01), but no significant difference was observed between Type II and III patients (P=0.14). The course of disease lengthened gradually from Type I to III (P<0.05; Figure 4). Due to the degree of symptom severity, the SF-36 scores decreased gradually (P<0.05). The AOFAS scores of the Type I patients were lower than those of the Type II and III patients, but no significant difference was found between the Type II and III patients. Additionally, there were no differences between the VAS scores of the Type I and II patients (P=0.96), but the VAS scores of the Type III patients were higher than those of the Type I and II patients (P<0.01) (Figure 5). Among the 3 types in our study, no significant differences were found in relation to the TAS and TTA (P>0.05).
Table 4
| Types | Demography | Scores | Angles | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | BMI | Course of disease | SF-36 | AOFAS | VAS | TAS | TTA | ||||||||||||||||
| Mean difference | P | Mean difference | P | Mean difference | P | Mean difference | P | Mean difference | P | Mean difference | P | Mean difference | P | Mean difference | P | ||||||||
| Type I vs. Type II | −2.97 | 0.37 | −3.24 | <0.01 | −14.00 | <0.01 | 6.97 | 0.03 | 21.53 | <0.01 | −0.01 | 0.96 | 0.86 | 0.55 | −0.20 | 0.85 | |||||||
| Type I vs. Type III | −5.35 | 0.09 | −4.18 | <0.01 | −23.04 | <0.01 | 15.67 | <0.01 | 26.95 | <0.01 | −0.89 | <0.01 | 0.65 | 0.63 | −0.23 | 0.81 | |||||||
| Type II vs. Type III | −2.38 | 0.47 | −0.94 | 0.14 | −9.04 | 0.04 | 8.70 | 0.01 | 5.42 | 0.05 | −0.87 | <0.01 | −0.21 | 0.88 | −0.04 | 0.97 | |||||||
BMI, body mass index; SF-36, 36-Item Short-Form Health Survey; AOFAS, American Orthopedic Foot and Ankle Society; VAS, Visual Analogue Scale; TAS, tibial anterior surface angle; TTA, tibial tilt angle.

Discussion
The terms “lateral ankle impingement”, “lateral hindfoot impingement”, and “subfibular impingement” are rarely mentioned as independent diagnoses (23-26); rather, they are often considered signs of calcaneal malunion or symptomatic flatfoot (6,7,10,11,27-29). However, little research has been conducted on patients complaining of lateral heel pain, who have no history of flatfoot or calcaneal fracture. Distal tibia varus deformity appears to be the only common point among these patients. Thus, in this study, we proposed a diagnosis of “distal tibia varus syndrome” to represent lateral ankle impingement caused by distal tibia varus deformity, and a classification system based on the symptoms and imaging manifestations.
The prevalence of the impingement is correlated with the hindfoot valgus angle (26). Malicky et al. (7) indicated that lateral hindfoot impingement might first occur in the sinus tarsi, and later progress to the calcaneofibular space. However, the relationship between hindfoot impingement and the tibia varus angle has not yet been described. Donovan and Rosenberg observed that (26) impingement did not occur if the hindfoot angle was lower than 14.1°, but isolated talocalcaneal osseous impingement occurred when the hindfoot valgus angle was 26.5°, and combined talocalcaneal-subfibular impingement occurred when the valgus angle was 27.1°. Similar to hindfoot valgus deformity, distal tibia varus deformity contributes to lateral ankle impingement. Conversely, the severe tibial deformity of calcaneus never appears. Thus, we assumed that soft-tissue impingement or combined talocalcaneal osseous impingement emerge in cases of distal tibia varus deformity combined with congruent ankle mortise and normal hindfoot alignment.
In this study, we found that the distal tibia varus deformity usually presented on both sides due to congenital causes, and it tended to occur in patients who needed to stand or sit for long periods when working, especially in women in their 40s and 50s. As weight increases, the fat and synovium tissues around the ankle joints become obviously proliferated, and as a result, these patients are more susceptible to symptoms of impingement. Notably, in most situations, the symptoms do not arise unless mild ankle injuries or sprains have occurred. The diagnosis of distal tibia varus syndrome was mainly based on the following symptoms and radiograph data: (I) subfibular pain and tenderness due to long-time loads or sports; and (II) varus inclination of the distal tibial joint surfaces on the anteroposterior ankle weight-bearing radiographs.
Plain radiographs are essential for diagnosis, both to identify the deformity and thus select the appropriate procedure, and to quantify the degree of correction that is required (30). The TAS is a crucial factor in assessments of the supramalleolar alignment and quantifications of the valgus or varus deformity (31). It was measured as 92.4°±3.1° (range, 84°−100°) in a radiographic study (32). In our study, the mean value of TAS (80.38°±4.80°) was significantly lower than the normal size that contributed to the subfibular impingement (P<0.01). Further, as a corresponding change, the tibial tilt angle, representing the varus degree of the distal tibial surface, increased to approximately 13°.
If the leg becomes misaligned in the coronal plane due to knee joint deformity, the subtalar joint will supinate or pronate to adjust the leg alignment in response to the varus or valgus deformity (33). Additionally, the subtalar joint plays a significant role in maintaining a normal relationship between the talus and the tibia (34). Inman (35) hypothesized that the subtalar joint acted as a torque transmitter and compensated for tibia varus and valgus deformities. Calcaneal eversion, which normally occurs in midstance, could maintain lateral tibiotalar contact. Additionally, research on foot pressure distribution demonstrated that the lateral contact of the sole was more significant in patients with varus knee, and revealed that mild-moderate abnormal leg alignment was compensated by the forefoot and midfoot in the latter half of the gait cycle. This explains why patients with distal tibia varus deformity have normal hindfoot alignment.
An experimental study (36) indicated that angular deformities of the tibia shaft <10° do not significantly alter ankle joint contact. A cadaveric study (37) confirmed that the location of the contact area was dependent on the joint position. When a stable ankle is in the varus and the supination position, it has a minimum contact area and a maximum pressure lying on the medial border of the talus. Thus, 13° varus malalignment of distal tibia coronal plane may place an asymmetric load on the ankle joint. As we observed, Type III of DTVS combined with all but 1 medial OLT was the result of asymmetric contact stresses on the ankle joint. However, Knupp et al. (38) performed a cadaveric study to quantify changes in pressure and force transfer in an ankle with a supramalleolar deformity, and found that the center of force and peak pressure moved in a posterolateral direction for varus deformities in isolated frontal plane deformity, as the ligaments and the fibula prevented the normalization of the tibiotalar load transfer. This explained why a lateral OLT occurred in a Type III patient.
MRI is valuable in assessing both the osseous and soft-tissue abnormalities associated with subfibular impingement syndromes (25). MRI is used in routine examinations due to its high sensitivity for displaying pathological changes. The existence of a subfibular impingement, most commonly including the high-signal intensity of soft-tissue entrapment between the calcaneus and fibula on the fat-suppression sequences of T2-weighted images, can be confirmed by MRI findings. Thus, the classification of distal tibia varus syndrome primarily depends on the following manifestations on the MRI images: Type I: no positive change; Type II: edema signs around the peroneal tendon; and Type III: signs of lateral edema and a medial osteochondral lesion.
The results demonstrated that Type I patients were relatively younger, had less severe symptoms, and a shorter course of disease than Type II and Type III patients. Type I patients also had a normal BMI, and were cured by conservative treatment. However, theoretically, Type I could develop into Type II or Type III, because the distal tibia varus deformity still exists. The symptoms of Type II and Type III patients are often recurrent and refractory. These patients often ignore being mildly uncomfortable, and thus received no effective treatments. As a result, the courses of disease of Types II and III were longer and the symptoms were more severe than those of Type I. Additionally, the results showed that the longer the course of disease, the greater the possibility of it developing to Type III. However, it was unclear whether the severity of OLT was related to the course of disease. The BMI analysis revealed that the Type II and Type III patients, especially middle-aged and older women, were a little overweight. Thus, soft-tissue (fat and synovium) proliferation between the calcaneus and fibular tip contributed to the impingement. In this situation, conservative treatments did not decrease the volume of soft tissue efficiently. Conversely, distal tibial valgus osteotomy corrected the tibial varus deformity and amplified the osseous space between the calcaneus and fibula, and prevented soft-tissue impingement and the pathogenic condition from developing. Additionally, regardless of the type, both the TAS and TTA were similar. Thus, a distal tibia varus deformity was the requirement for the diagnosis, but it had no specific relationship with the severity of the symptoms. This also means that the existence of a distal tibia varus deformity does not always cause symptoms unless another incitant occurs.
According to the results of the scoring system, the scores of the Type I patients were lower than those of Types II and III patients. Thus, conservative treatments to enlarge the osseous distance between the fibulas and calcaneus, or lessen the volume of subfibular soft tissue appear to effectively control the pain. As for Types II and III, the reactive proliferation of soft tissue between the lateral malleolus and calcaneus could not be completely eliminated unless surgery was performed to correct the distal tibial alignment.
Supramalleolar valgus osteotomy was commonly used to treat symptoms by redistributing the joint contact forces (39) and was considered an alternative treatment for patients with beginning or mid-stage asymmetric ankle osteoarthritis with concomitant varus deformity (31). Schmid et al. (12) concluded that supramalleolar valgus osteotomy significantly shifted the center of force laterally, and reduced anteromedial ankle joint contact stresses. OLT is an early indicator of varus ankle osteoarthritis (20,40). Based on the results of this study, we believe that this type of surgery could delay or even prevent the degenerative progression of the tibiotalar joint. Both the TAS and TTA were well corrected by tibial supramalleolar valgus osteotomy. Numerous cadaveric studies have been performed to explore the pathological mechanism of lateral ankle impingement and osteochondral lesions, but more clinical research needs to be conducted to determine the effects of supramalleolar osteotomy.
Our study had several limitations. First, the follow-up period was relatively short, and further surveillance of the patients is needed to monitor the effects of the osteotomy. Second, the case number of each type was limited. The frequency at which the impingement occurs and the severity of the deformity before the impingement occurs are not known. Further, it is still uncertain when patients will progress from Type I to Types II or III. Only a natural history study would be able to provide this information. Finally, there was a lack of weight-bearing CT or MRI examinations, and no direct imaging evidence of the subfibular impingement. This study simply provides a starting point for observations that might help us to better understand why distal tibia varus deformity is sometimes a pathological condition. This information also needs to be incorporated into clinical care. Additionally, it is currently unclear why most distal tibia varus deformities are not painful.
In conclusion, this study proposed the new concept of distal tibia varus syndrome. It is characterized by the symptom of subfibular pain and the sign of distal tibial surface varus on weight-bearing radiographs. Depending on the MRI manifestations, it can be classified into 3 types (i.e., Type I: the non-reactive type, Type II: the proliferative type, and Type III: the osteochondral lesion type). Type I patients can be cured using conservative methods. For Type II and III patients, excellent clinical and radiographic outcomes can be achieved following supramalleolar valgus osteotomy. Additionally, OLT needs to be treated in Type III patients via microfracture or osteochondral autograft transplantation simultaneously.
Acknowledgments
We wish to express our sincere thanks to Fangxiu Luo and her teammates from the Pathology Department, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. We would also like to thank the patients.
Funding: This study was supported by the National Natural Science Foundation of China (81772372), the Scientific Research Fund of Shanghai Jiading District Health Committee (2020-QN-01), and the Research Fund of Ruijin Hospital North, Shanghai Jiao Tong University School of Medicine (2020ZY16).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-997/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-997/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-997/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Ruijin Hospital [No. 75 (2013)] and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Henderson I, La Valette D. Ankle impingement: combined anterior and posterior impingement syndrome of the ankle. Foot Ankle Int 2004;25:632-8. [Crossref] [PubMed]
- Kim HK, Jeon JY, Dong Q, et al. Ankle arthroscopy in a hanging position combined with hindfoot endoscopy for the treatment of concurrent anterior and posterior impingement syndrome of the ankle. J Foot Ankle Surg 2013;52:704-9. [Crossref] [PubMed]
- Miyamoto W, Takao M, Matsui K, et al. Simultaneous ankle arthroscopy and hindfoot endoscopy for combined anterior and posterior ankle impingement syndrome in professional athletes. J Orthop Sci 2015;20:642-8. [Crossref] [PubMed]
- Niek van Dijk C. Anterior and posterior ankle impingement. Foot Ankle Clin 2006;11:663-83. [Crossref] [PubMed]
- Song B, Li C, Chen Z, et al. Combined Anterior and Dual Posterolateral Approaches for Ankle Arthroscopy for Posterior and Anterior Ankle Impingement Syndrome. Foot Ankle Int 2016;37:605-10. [Crossref] [PubMed]
- Ellis SJ, Deyer T, Williams BR, et al. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot Ankle Int 2010;31:361-71. [Crossref] [PubMed]
- Malicky ES, Crary JL, Houghton MJ, et al. Talocalcaneal and subfibular impingement in symptomatic flatfoot in adults. J Bone Joint Surg Am 2002;84:2005-9. [Crossref] [PubMed]
- Roberts CC, Morrison WB, Liu PT. Imaging evaluation of foot and ankle pathology: self-assessment module. AJR Am J Roentgenol 2008;190:S18-22. [Crossref] [PubMed]
- Squires B, Allen PE, Livingstone J, et al. Fractures of the tuberosity of the calcaneus. J Bone Joint Surg Br 2001;83:55-61. [Crossref] [PubMed]
- Atkins RM. The treatment of calcaneal malunion. Foot Ankle Clin 2014;19:521-40. [Crossref] [PubMed]
- Al-Ashhab ME. Treatment for calcaneal malunion. Eur J Orthop Surg Traumatol 2013;23:961-6. [Crossref] [PubMed]
- Schmid T, Zurbriggen S, Zderic I, et al. Ankle joint pressure changes in a pes cavovarus model: supramalleolar valgus osteotomy versus lateralizing calcaneal osteotomy. Foot Ankle Int 2013;34:1190-7. [Crossref] [PubMed]
- Yang C, Xu X, Zhu Y, et al. A Long-Term Study of the Effect of Subtalar Arthrodesis on the Ankle and Hindfoot Joints. J Am Podiatr Med Assoc 2016;106:47-53. [Crossref] [PubMed]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Crossref] [PubMed]
- Loew M, Raiss P. A symptom-based classification for shoulders with massive rotator cuff defects. Int Orthop 2010;34:63-9. [Crossref] [PubMed]
- Tanaka Y. The concept of ankle joint preserving surgery: why does supramalleolar osteotomy work and how to decide when to do an osteotomy or joint replacement. Foot Ankle Clin 2012;17:545-53. [Crossref] [PubMed]
- Siddiqui NA, Herzenberg JE, Lamm BM. Supramalleolar osteotomy for realignment of the ankle joint. Clin Podiatr Med Surg 2012;29:465-82. [Crossref] [PubMed]
- Rush SM. Supramalleolar osteotomy. Clin Podiatr Med Surg 2009;26:245-57. [Crossref] [PubMed]
- Becker AS, Myerson MS. The indications and technique of supramalleolar osteotomy. Foot Ankle Clin 2009;14:549-61. [Crossref] [PubMed]
- Polat G, Erşen A, Erdil ME, et al. Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg Sports Traumatol Arthrosc 2016;24:1299-303. [Crossref] [PubMed]
- Guney A, Yurdakul E, Karaman I, et al. Medium-term outcomes of mosaicplasty versus arthroscopic microfracture with or without platelet-rich plasma in the treatment of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 2016;24:1293-8. [Crossref] [PubMed]
- Park HW, Lee KB. Comparison of chondral versus osteochondral lesions of the talus after arthroscopic microfracture. Knee Surg Sports Traumatol Arthrosc 2015;23:860-7. [Crossref] [PubMed]
- Hauger O, Moinard M, Lasalarie JC, et al. Anterolateral compartment of the ankle in the lateral impingement syndrome: appearance on CT arthrography. AJR Am J Roentgenol 1999;173:685-90. [Crossref] [PubMed]
- Wang PH, Su WR, Jou IM. Lateral Hindfoot Impingement After Nonunion of Fracture of the Lateral Process of the Talus. J Foot Ankle Surg 2016;55:387-90. [Crossref] [PubMed]
- Donovan A, Rosenberg ZS. MRI of ankle and lateral hindfoot impingement syndromes. AJR Am J Roentgenol 2010;195:595-604. [Crossref] [PubMed]
- Donovan A, Rosenberg ZS. Extraarticular lateral hindfoot impingement with posterior tibial tendon tear: MRI correlation. AJR Am J Roentgenol 2009;193:672-8. [Crossref] [PubMed]
- Banerjee R, Saltzman C, Anderson RB, et al. Management of calcaneal malunion. J Am Acad Orthop Surg 2011;19:27-36. [Crossref] [PubMed]
- Reddy V, Fukuda T, Ptaszek AJ. Calcaneus malunion and nonunion. Foot Ankle Clin 2007;12:125-35. [Crossref] [PubMed]
- Elgafy H, Ebraheim NA. Subtalar arthroscopy for persistent subfibular pain after calcaneal fractures. Foot Ankle Int 1999;20:422-7. [Crossref] [PubMed]
- Perera A, Guha A. Clinical and radiographic evaluation of the cavus foot: surgical implications. Foot Ankle Clin 2013;18:619-28. [Crossref] [PubMed]
- Barg A, Saltzman CL. Single-stage supramalleolar osteotomy for coronal plane deformity. Curr Rev Musculoskelet Med 2014;7:277-91. [Crossref] [PubMed]
- Knupp M, Ledermann H, Magerkurth O, et al. The surgical tibiotalar angle: a radiologic study. Foot Ankle Int 2005;26:713-6. [Crossref] [PubMed]
- Olerud C. The pronation capacity of the foot--its consequences for axial deformity after tibial shaft fractures. Arch Orthop Trauma Surg 1985;104:303-6. [Crossref] [PubMed]
- Ting AJ, Tarr RR, Sarmiento A, et al. The role of subtalar motion and ankle contact pressure changes from angular deformities of the tibia. Foot Ankle 1987;7:290-9. [Crossref] [PubMed]
- Inman VT. The influence of the foot-ankle complex on the proximal skeletal structures. Artif Limbs 1969;13:59-65. [PubMed]
- Wagner KS, Tarr RR, Resnick C, et al. The effect of simulated tibial deformities on the ankle joint during the gait cycle. Foot Ankle 1984;5:131-41. [Crossref] [PubMed]
- Bruns J, Rosenbach B. Pressure distribution at the ankle joint. Clin Biomech (Bristol, Avon) 1990;5:153-61. [Crossref] [PubMed]
- Knupp M, Stufkens SA, van Bergen CJ, et al. Effect of supramalleolar varus and valgus deformities on the tibiotalar joint: a cadaveric study. Foot Ankle Int 2011;32:609-15. [Crossref] [PubMed]
- Stufkens SA, van Bergen CJ, Blankevoort L, et al. The role of the fibula in varus and valgus deformity of the tibia: a biomechanical study. J Bone Joint Surg Br 2011;93:1232-9. [Crossref] [PubMed]
- Navid DO, Myerson MS. Approach alternatives for treatment of osteochondral lesions of the talus. Foot Ankle Clin 2002;7:635-49. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)
Cite this article as: Yang C, Liu P, Cao Y, Guo C, Zhu Y, Xu X. Therapeutic efficacy analysis of distal tibia varus syndrome with different classification and different therapy: a cross-sectional study. Ann Transl Med 2022;10:270.


