
Clinical significance of the diverse interlobar veins hidden in the upper oblique fissure
Introduction
The upper oblique fissure (UOF) potentially separates the posterior segment of the right upper lobe (RUL) and the superior segment of the right lower lobe (RLL) (1). Existing reports reveal that approximately 70% of UOFs are not fully developed (2), and 39% of patients with an incomplete UOF have venous variation (3). Since most right pulmonary operations involve the fissure crest, where the horizontal fissure meets the oblique fissure, and where the interlobar veins are embedded, cursory disposal of this region inevitably causes accidental injury during surgery. However, the distribution of right top pulmonary veins (RTPVs) hidden in the UOF has not been studied thoroughly; to the best of our knowledge, there are no reports on the classification of interlobar veins in the UOF.
Preoperative three-dimensional computed tomography bronchography and angiography (3D-CTBA) allows visualization of anatomical structures and is becoming an indispensable tool in thoracic surgery (4,5). In this study, 3D-CTBA was used to analyze the subtypes of interlobar veins hidden in the UOF. The clinical data of patients who underwent surgery in our center were collected to investigate the relationship between interlobar vein subtypes and accidental injury. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-21-4913/rc).
Methods
Study design and patient collection
This retrospective cohort study was carried out following the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Ethics Committee of The First Affiliated Hospital of Nanjing Medical University (2021-SR-164), and informed consent was obtained from each patient. Patients who underwent thoracoscopic surgery from January 2019 to June 2020 in the Department of Thoracic Surgery were enrolled. The inclusion criteria were as follows: (I) age ≥18 years old; (II) diagnosis of lung cancer; and (III) a right UOF requiring management during thoracoscopic surgery. Records with incomplete imaging data or lesions blurring the identification of interlobar veins were excluded. Records with incomplete videos of the operation with failure to show the upper right oblique fissure were excluded from the surgical data analysis. The flow diagram is shown in Figure 1.
Types of interlobar veins
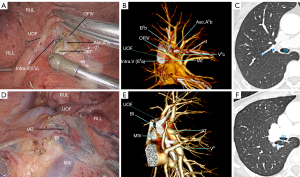
According to the venous origin, the interlobar veins hidden in the UOF of the right lung could be classified as oblique fissure-type interlobar veins (OFIVs) and mediastinal-type interlobar veins (MIVs). The OFIVs originated from the central vein (Central. V) or V2c, ran between the RUL and the RLL, and entered the UOF (Figure 2A,2B). The diameter of the OFIV was measured at the origin in the lung window on contrast-enhanced computed tomography (CT) (Figure 2C). The MIVs originated from the inferior pulmonary vein, V6, or the left atrium and entered the UOF posterior to the bronchus intermedius (BI) (Figure 2D,2E). The diameter of the MIV was measured in the same way as OFIV (Figure 2F). The branches of the interlobar veins were named after the corresponding pulmonary segment where the vein drained. For instance, if the intrasegmental vein (S1a) [Intra.V (S1a)], the Intra.V (S2a), and S2 terminal vein (V2t) drained to the interlobar vein, the subtype was named V2t + Intra.V (S1a) + Intra.V (S6a). Subtype modeling was based on the data of all branch types.
Definition of fissure development
Fissure development was estimated according to Craig and Walker’s criteria, which combine the degree of completeness of the fissures and the location of the pulmonary artery at the base of the oblique fissure (6). A complete UOF is formed by the intact interlobar pleura separating the RUL and RLL. An incomplete UOF refers to the partial fusion of the RUL with the RLL, which requires dissection of the interlobar pleura to expose the intermedial arterial trunk (IAT) or interlobar vein. Fissure agenesis refers to the total absence of the interlobar pleura, which leads to extreme difficulty in exposing the IAT or interlobar vein at the location of the crest.
Analysis of interlobar vein injuries
The above interlobar vein subtypes were further analyzed regarding accidental injury correlated with surgery. In patients with a clear display of interlobar vein branches in a complete UOF, when the branches distributed at the nontarget surgical region were mistransected, accidental injury was recorded. In patients with incomplete or absent interlobar fissures, the distribution of interlobar veins on 3D-CTBA images and the scope of surgical resection were combined to comprehensively determine interlobar vein injury.
Statistical analysis
Statistical analyses were performed using the SPSS (version 23.0; SPSS Inc., Chicago, IL, USA) and GraphPad Prism (version 6.0; GraphPad Software Inc., La Jolla, CA, USA). Quantitative data are expressed as the mean ± standard deviation, and qualitative data are expressed as the number of cases (percentage). A receiver operating characteristic (ROC) curve was used to predict the possibility of single- or multibranched interlobar veins. A P value less than 0.05 was considered indicative of a significant difference.
Results
The clinical data of 419 consecutive patients who underwent thoracoscopic surgery from January 1st, 2019, to June 30th, 2020, were collected. Finally, 21 patients were excluded due to incomplete imaging data or lesions blurring the identification of interlobar veins, and 398 patients were enrolled. Among these patients, 237 received contrast-enhanced CT scans, and 161 received plain CT scans. 3D-CTBA images were reconstructed with Deepinsight software (Key Laboratory of Intelligent Computing in Medical Image, Ministry of Education, Northeastern University, Shenyang, China). Then, the morphology and distribution of the interlobar vein in the UOF were independently analyzed by 2 thoracic surgeons. Two experienced radiologists measured the diameters of the interlobar veins in the lung windows of the contrast-enhanced CT images of 237 patients (window width =1,400 HU, window position =−500 HU). The images of 161 patients with noncontrast CT scans were analyzed only to determine interlobar vein subtypes. Furthermore, 153 patients with complete videos of the operation, including details of the UOF, were included for surgical data analysis. Participation at each stage is shown in the flow diagram (Figure 1).
Interlobar vein subtypes
The results of the 3D-CTBA image analysis of 398 patients showed diversity in the interlobar vein subtypes (Table 1). An OFIV was the most frequent type, accounting for 85.9% (342/398) of cases, and vastly outnumbered the MIV type (13.8%, 55/398). Interlobar vein absence was observed in 0.3% of cases (1/398). Various main types could be further subdivided into 30 distribution manifestations. A total of 73.6% (293/398) of patients had branches distributed bilaterally into the upper and lower lobes, and 26.1% (104/398) had branches distributed only into the upper lobe. Additionally, 69.6% (238/342) of OFIVs had Intra.V (S6a) branches distributed into the lower lobe. All MIV types contained branches distributed into the RUL (55/55), originating from S2 or S1 veins.
Table 1
| Types of interlobar veins | Only upper lobe branches (n=104) | Both upper and lower lobe branches (n=293) | |||
|---|---|---|---|---|---|
| Subtypes | N | Subtypes | N | ||
| OFIV (n=342) | V2t | 56 | V2t + Intra.V (S1a) + Intra.V (S6a) | 2 | |
| V2t + Intra.V (S2a) | 14 | V2t + Intra.V (S2a) + Intra.V (S6a) | 41 | ||
| V2t + V2a | 1 | V2t + V2a + Intra.V (S6a) | 10 | ||
| V2t + V2a2 | 17 | V2t + V2a2 + Intra.V (S6a) | 34 | ||
| V2t + V2b | 11 | V2t + V2b + V1a + Intra.V (S6a) | 1 | ||
| V2t + V2b + V2a + V1a | 1 | V2t + V2b + V2a + Intra.V (S6a) | 11 | ||
| V2t + V2b + V2a2 | 1 | V2t + V2b + V2a2 + Intra.V (S6a) | 8 | ||
| V2t + V2b2 | 3 | V2t + V2b + Intra.V (S6a) | 59 | ||
| – | – | V2t + V2b2 + V2a2 + Intra.V (S6a) | 1 | ||
| – | – | V2t + V2b2 + Intra.V (S6a) | 1 | ||
| – | – | V2t + Intra.V (S6a) | 70 | ||
| MIV (n=55) | – | – | V2t + Intra.V (S1a) | 1 | |
| – | – | V2t + Intra.V (S2a) | 10 | ||
| – | – | V2t + V2a | 1 | ||
| – | – | V2t + V2a2 | 8 | ||
| – | – | V2t + V2b + V2a | 2 | ||
| – | – | V2t + V2b + V2a2 | 2 | ||
| – | – | V2t + V2b + V2c | 1 | ||
| – | – | V2t + V2b | 4 | ||
| – | – | V2t + V2b2 | 1 | ||
| – | – | V2t + V2b2 + V2a2 | 1 | ||
| – | – | V2t | 24 | ||
One patient had no interlobar veins. 3D-CTBA, three-dimensional computed tomography bronchography and angiography; OFIV, oblique fissure-type interlobar vein; MIV, mediastinal-type interlobar vein; Intra.V, intrasegmental vein.
The subtype analysis in Table 1 shows that 83.6% (286/342) of OFIVs had multiple branches. Single-branched OFIVs with only a V2t branch accounted for 16.4% (56/342) of all OFIV cases. Branches of the interlobar vein included S2-related Intra.V (S2a), V2a, V2a2, V2b, V2b2, and V2t, S1 related Intra.V (S1a), V1a, and S6 related Intra.V (S6a). A total of 56.4% (31/55) of MIV cases had multiple branches, 43.6% (24/55) of which were single-branched only with V2t.
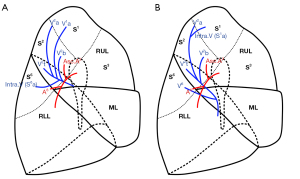
Figure 3 presents the common distribution of the interlobar veins. OFIVs ran in the UOF, branched into Intra.V (S6a) and V2t branches, and then ran in the RUL and branched into V2b, V2b2, V2a, V2a2, ectopic V1a, or Intra.V (S1a) branches in some patients (Figure 3A). The MIV originated from V6, coursed over the BI, extended upward along the posterior mediastinum, and branched into a V2t branch in the UOF. The distribution of other MIV branches in the RUL was similar to that of the OFIV except for an ectopic V1a (Figure 3B).
Analysis of interlobar vein injuries
As shown in Table 2, accidental injuries of the interlobar veins occurred in 19.1% (9/47) of patients with a complete UOF, 35.3% (6/17) of patients without a UOF, and 50.6% (45/89) of patients with an incomplete UOF. The incidence of interlobar vein injury was significantly higher in patients with an incomplete UOF (χ2=12.856, P=0.02). In total, Intra.V (S6a) injury accounted for 91.7% (44/48) of OFIV injuries, and single-branched V2t injury accounted for 75% (9/12) of MIV injuries.
Table 2
| Surgery type | Injuries in the complete fissure (9/47) | Injuries in the incomplete fissure (45/89) | Injuries in the absent fissure (6/17) | |||||
|---|---|---|---|---|---|---|---|---|
| OFIV (9/44)† | MIV (0/2) | OFIV (35/70) | MIV (10/19) | OFIV (4/14) | MIV (2/3) | |||
| RUL [65] | Intra.V (S6a) (4/20)† | – | Intra.V (S6a) (28/34) | 0/5 | Intra.V (S6a) (4/4) | 0/1 | ||
| RS2 [15] | V2a2 (1/7) | – | Intra.V (S6a) (4/7) | 0/1 | – | – | ||
| Intra.V (S6a) (1/7) | Intra.V (S6a) + V2a2 (2/7) | |||||||
| RS1 + S2 [10] | 0/2 | – | Intra.V (S6a) (1/6) | 0/1 | 0/1 | – | ||
| RS1a + S2 [2] | – | – | 0/2 | – | – | – | ||
| RS2 + S3a [1] | V2a2 (1/1) | – | – | – | – | – | ||
| RS2b [4] | Intra.V (S2a) (2/3) | – | – | 0/1 | – | – | ||
| RS2b + S3a [1] | – | – | 0/1 | – | – | – | ||
| RLL [37] | 0/6 | 0/1 | 0/16 | V2t (4/6) | 0/6 | V2t (1/2) | ||
| V2t + V2a2 (1/6) | V2t + Intra.v (S2a) (1/2) | |||||||
| RLL + ML [3] | – | – | – | V2t (1/1) | 0/2 | – | ||
| RS6 [13] | 0/4 | 0/1 | 0/3 | V2t (3/4) | 0/1 | – | ||
| V2t + Intra.V (S2a) (1/4) | ||||||||
| RS6 + S9 + S10 [1] | – | – | 0/1 | – | – | – | ||
| RS6 + S8a [1] | 0/1 | – | – | – | – | – | ||
Data are present as interlobar vein injured cases/total cases in each surgery subtype and interlobar vein type. †, one patient had no interlobar veins. UOF, upper oblique fissure; OFIV, oblique fissure-type interlobar vein; MIV, mediastinal-type interlobar vein; RUL, right upper lobe; RS, right segment; RLL, right upper lobe; ML, middle lobe; Intra.V, intrasegmental vein.
In the complete fissure group, of the 44 patients with OFIVs, 5 patients suffered from injury of Intra.V (S6a) during right upper lobectomy, including 1 with V2a2 injury and 1 with Intra.V (S6a) injury during S2 resection, 1 with V2a2 injury during S2 + S3a resection, and 2 with Intra.V (S2a) injury during S2b resection. No MIV branches were injured in patients with complete fissures.
In the fissure absence group, of the 14 patients with OFIVs, 4 patients suffered from injury of the Intra.V (S6a) branch of the OFIV during right upper lobectomy. Of the 3 patients with MIVs, 2 patients suffered from V2t and Intra.V (S2a) injury during right lower lobectomy.
In the incomplete fissure group, of the 70 patients with OFIVs, 28 patients suffered from Intra.V (S6a) injury during right upper lobectomy, and 6 suffered from Intra.V (S6a) injury during S2 resection. Of the 19 patients with MIVs, 10 patients suffered from injuries, including 4 with V2t injury and 1 with V2t + V2a2 injury during right lower lobectomy, 1 with V2t injury during right lower and middle lobectomy, and 3 with V2t and 1 with V2t + Intra.V (S2a) injury during S6 resection.
ROC curve of single- and multibranched interlobar veins
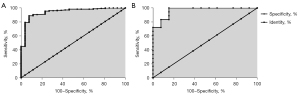
Table 2 shows that Intra.V (S6a) injury accounted for 91.7% of OFIV injuries, and single-branched V2t injury accounted for 75% of MIV injuries. As evidenced from the interlobar vein subtypes (Table 1), the Intra.V (S6a) type was present in OFIVs with multiple branches. MIV injury mainly occurred in the single-branched V2t of the upper lobe. Therefore, we measured the diameters of single- and multibranched interlobar veins in the lung window on contrast-enhanced CT images in 237 of 398 patients (Table 3). In 206 patients with OFIVs, the diameter of the multibranched interlobar vein was 3.84±1.26 mm. In 31 patients with MIVs, the diameter of the single-branched V2t was 1.81±0.42 mm.
Table 3
| Types of interlobar veins | Single-branched | Multi-branched | Lower lobe branches | Upper lobe branches |
|---|---|---|---|---|
| OFIV (n=206) | 1.83±0.57 (n=26) | 3.84±1.26 (n=180) | Intra.V (S6a) (n=152) | – |
| MIV (n=31) | 1.81±0.42 (n=13) | 3.69±1.21 (n=18) | – | V2t (n=31) |
CT, computed tomography; OFIV, oblique fissure-type interlobar vein; MIV, mediastinal-type interlobar vein.
As shown in Figure 4, a ROC curve was applied to analyze the predictive value of interlobar vein diameter for multibranched interlobar veins. The results showed that an OFIV diameter greater than 2.4 mm was a predictor of multibranched interlobar veins. The area under the ROC curve (AUC) was 94.3%, with a sensitivity of 88.9% and a specificity of 92.3% (P<0.001). A MIV diameter less than 2 mm indicated that the interlobar vein was a single-branched V2t. The AUC was 96.6%, with a sensitivity of 100% and a specificity of 84.6% (P<0.001).
Discussion
Intersegmental veins play a vital role in maintaining the ventilation/perfusion ratio of the pulmonary segment. The interlobar veins in the UOF involve multiple intersegmental veins. With the development of precise lung segment surgery, an increasing number of clinicians have paid attention to the diversity of interlobar veins. Our results also revealed 2 major types of interlobar veins, which contained up to 30 distribution patterns. The degree of completeness of the pulmonary fissure and the distribution of the interlobar vein were determinants correlated with the risk of intraoperative interlobar vein injury. The diameter of the interlobar veins on two-dimensional CT images can predict the branching mode of interlobar veins, which provides auxiliary support for the general classification in 3D-CTBA images.
Intersegmental veins were reported in a study by Yamashita (7), in which the emphasis was the central vein, and the branches of the interlobar veins were not analyzed separately. Although Yamashita defined the terminal branch of V2 as V2t (7), the study showed that V2t could accept drainage from other branches. We propose that V2t should be considered an independent branch that is only distributed in S2. Our results showed that only 16.4% of OFIVs were composed of the V2t branch alone, while 83.6% of interlobar veins had multiple branches, with Intra.V (S6a) of the interlobar vein accounting for the highest proportion (69.6%). In addition, the interlobar veins could also produce other branches, such as the rare ectopic V1a and Intra.V (S1a) branches, accounting for 0.6% of all branches.
Some scholars consider a MIV as a RTPV that accepts drainage from V2 and V3, with an incidence of approximately 0.3–9.3% (8-10). In this study, the proportion of MIVs was 13.8%, which was higher than that reported in previous studies. A possible reason is that the RTPV could be more easily identified in 3D-CTBA images.
Interlobar vein injuries were most common in Intra.V (S6a) branches of a multibranched OFIV and V2t of a single-branched MIV. The ROC curve revealed a close correlation between the diameter of the interlobar vein and the branching mode. An OFIV diameter larger than 2.4 mm often indicates multiple branches of the interlobar vein, and increased caution should be taken to prevent accidental injuries. A MIV diameter less than 2 mm often indicates a high risk of single-branched V2t injury.
In addition to the diameter and distribution pattern of the interlobar veins, the completeness of the UOF was also a risk factor for interlobar vein injury. Among 89 patients with an incomplete UOF, interlobar vein injury was common (50.6%). For patients with incomplete or absent UOFs, the right superior pulmonary vein or inferior pulmonary vein was the primary anatomical structure to be divided when using the fissureless technique (11), which can easily cause interlobar vein injury (Figure 3). We suggest disassociating the anterior mediastinal vein branch (V1) of the right superior pulmonary vein first when using the fissureless technique in an upper lobectomy, which helps preserve the interlobar veins. Other techniques include transecting the incomplete UOF above the OFIV in upper lobe surgery and carefully identifying the MIV in the posterior mediastinum in lower lobe surgery.
There are some limitations to this study. First, this was a retrospective study performed at a single institution, and there was a possibility of inherent bias. However, to overcome this limitation, we aimed to include as many patients as possible using logical selection. Second, further analysis of the clinical complications caused by interlobular vein injury was not carried out. We are planning to implement this in the future by collecting more high-quality data.
Conclusions
Diverse interlobar veins could be classified into the OFIV and MIV subtypes according to the distribution pattern. The diversity of the interlobar veins and the completeness of the UOF were noteworthy risk factors in surgery involving dissection of the UOF. The vein diameter on two-dimensional CT images and vein classification on 3D-CTBA images could provide supporting information to avoid accidental injury of interlobar veins.
Acknowledgments
We would like to thank American Journal Experts (https://www.aje.com/) for English language editing.
Funding: This work was supported in part by the National Natural Science Foundation of China (81972175), Key Medical Research Project of Jiangsu Provincial Health Commission (K2019002), Ethicon Excellence in Surgery Grant (HZB-20190528-13), and Jiangsu Province Natural Science Foundation (BK20201492).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-21-4913/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-21-4913/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-21-4913/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study conforms to the provisions of the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The First Affiliated Hospital of Nanjing Medical University (2021-SR-164). All patients signed an informed consent form before participating in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hayashi K, Aziz A, Ashizawa K, et al. Radiographic and CT appearances of the major fissures. Radiographics 2001;21:861-74. [Crossref] [PubMed]
- Raasch BN, Carsky EW, Lane EJ, et al. Radiographic anatomy of the interlobar fissures: a study of 100 specimens. AJR Am J Roentgenol 1982;138:1043-9. [Crossref] [PubMed]
- Sedlackova Z, Ctvrtlik F, Miroslav H. Prevalence of incomplete interlobar fissures of the lung. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016;160:491-4. [Crossref] [PubMed]
- Yamada S, Suga A, Inoue Y, et al. Importance of preoperative assessment of pulmonary venous anomaly for safe video-assisted lobectomy. Interact Cardiovasc Thorac Surg 2010;10:851-4. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery†. Eur J Cardiothorac Surg 2014;46:e120-6. [Crossref] [PubMed]
- Kc S, Shrestha P, Shah AK, et al. Variations in human pulmonary fissures and lobes: a study conducted in nepalese cadavers. Anat Cell Biol 2018;51:85-92. [Crossref] [PubMed]
- Yamashita H. Roentgenologic Anatomy of the Lung. Tokyo: Igaku-Shoin, 1978:53-6.
- Lickfett L, Kato R, Tandri H, et al. Characterization of a new pulmonary vein variant using magnetic resonance angiography: incidence, imaging, and interventional implications of the "right top pulmonary vein". J Cardiovasc Electrophysiol 2004;15:538-43. [Crossref] [PubMed]
- Arslan G, Dincer E, Kabaalioglu A, et al. Right top pulmonary vein: evaluation with 64 section multidetector computed tomography. Eur J Radiol 2008;67:300-3. [Crossref] [PubMed]
- Akiba T, Morikawa T, Inagaki T, et al. A new classification for right top pulmonary vein. Ann Thorac Surg 2013;95:1227-30. [Crossref] [PubMed]
- Nomori H, Ohtsuka T, Horio H, et al. Thoracoscopic lobectomy for lung cancer with a largely fused fissure. Chest 2003;123:619-22. [Crossref] [PubMed]



