Professor Jianxing He was granted AATS membership
The 95th AATS Annual Meeting 2015 was held on April 25-29 at the Washington State Convention Center. The AATS, short for American Association for Thoracic Surgery, was founded in 1917 and has become an international organization of over 1,300 of the world’s foremost cardiothoracic surgeons representing 41 countries. AATS Annual Meeting has always been dedicated to continuing education as the top conference in the cardiothoracic field and has attracted cardiothoracic surgeons from across the world to attend.
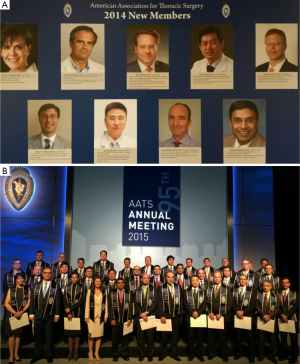
At the AATS Annual Meeting 2015, Prof. Jianxing He, Director of the First Affiliated Hospital of Guangzhou Medical University and Director of the Thoracic Department, was elected a member of AATS (Figures 1,2). We are honored to have an interview with Prof. He to share his perspective in thoracic surgery.

Fast-track recovery
Prof. He is among the first thoracic surgeons in China using video-assisted thoracoscopic surgery (VATS). In 2011, he began to perform spontaneous respiratory surgeries. The new practice has sharply reduced patients’ recovery time and made fast-track recovery possible. So far, 1,100 such surgeries have been performed, including 165 cases of radical resection for lung cancer and one case of sleeve resection. Earlier this year, Prof. He and his team came up with a new idea—“Tubeless VATS”. Under this concept, VATS may be performed without placing a chest drainage tube into the chest, which allows some patients, especially those with pulmonary small nodules, to be discharged within 24 hours after the surgery.
“‘Tubeless VATS’ places higher demand on thoracic surgeons, because you need to make sure the trachea and the surface of lung incision have no air leak.” said Prof. He, “from patients’ perspective, this brings more benefits to them. In combination with spontaneous respiratory surgery, we can offer 24-hour solutions to patients”.
Taking sleeve resection as an example, Prof. He shared his experience on how to carry out complicated surgeries. Interrupted anastomosis has been extensively used in sleeve resection, according to literature; however, Prof. He figured out an innovative approach called one-stitch anastomosis. Sleeve resection involves the division of two parts—bronchus and blood vessels. For a thoracic surgery, the most difficult jobs include the partial resection of the left atrium, dual sleeve resection of bronchus and vessels, and resection and reconstruction of carina. There are two reconstruction methods: interrupted anastomosis in the earlier years and now the continuous suture. Prof. He and his team have so far performed surgeries in 13 cases by using the continuous suture. This technique has also been applied in surgeries for bronchus and arteries. Continuous suture features two primary benefits. First, it can be completed in a short period of time. It generally takes about 20 minutes for bronchus and blood vessel anastomosis. Second, there are fewer complications (e.g., blood leakage). Based on a large number of practical cases and years of clinical practices, he concluded that continuous suture is convenient, safe, and reliable.
He noted that it’s more than a matter of how a surgery is carried out. The application of total thoracoscopy can also make a traditionally complicated surgery successful, and a successful surgery can increase the thoracic surgeons’ confidence on thoracic surgeries. Obviously, when a surgeon can successfully carry out a complicated surgery, he should be able to do a better job for less complex surgeries.
It’s noteworthy that Prof. He’s spontaneous respiratory sleeve resection is reportedly the world’s first such surgery. This record has inarguably lifted China’s profile in the international medical community and inspired more Chinese doctors and medical researchers to innovate. Prof. He revealed that it was quite a challenge for his team when they began to perform Spontaneous respiratory pulmonary operations 3 years ago, which is more of a departure from traditional perception than technical hurdles. For the cardiac surgery, it can be performed when the heart is beating or not and the off-pump heart bypass surgery can be successful conducted. Similarly, a lung surgery can also be successfully carried out while the patient maintains spontaneous breathing.
“The sticking point of spontaneous respiratory sleeve resection is the change of the perception that patient safety might be on the line when the surgery is performed under non-intubated anesthesia,” said Prof. He. In fact, this surgery is generally similar to the conventional pulmonary lobectomy and their only difference is that it requires more delicate skills. The suturing should be performed in a gentle manner, and resection should not be carried out when the patient is having a deep breath. The most important issue is that the surgeon must properly deal with blood vessels and take precautionary measures to prevent bleeding during the surgery.
Prof. He has successfully removed some large tumors with the help of VATS, fixing lung problems in a small space and sometimes repairing the cardiac structure and even for the angioplasty of superior vena cava. These challenging surgeries have demonstrated his superb medical skills and delicate techniques, but he said for a doctor the most important is to be scrupulous, have a creative and innovative mind, and dare to try different approaches. In fact, they had associated the skills of open surgeries with the VATS techniques. Their difference is that: for the open surgeries, you are seeing a three-dimension structure; for VATS, in contrast, you are seeing a two-dimension structure. The key point is how to achieve the same goal in a two-dimensional vision. If the whole surgical process is proven safe, the safe techniques can also be used in the two-dimensional surgeries, and that would cause less controversy. Moreover, unlike in the past when all procedures were performed manually, nowadays surgeons have various instruments at their disposal to help them fix blood vessels.
The book Lung cancer in the era of “precision medicine”
Over the past 5 years, medical science and technology has advanced so much that makes individualized and precise treatment a reality. “When we look back,” said Prof. He, “we find that modern technology has witnessed dramatic changes, and many up-to-date technologies have been applied to diagnose and treat lung cancer.” In view of the remarkable changes in the diagnosis and treatment of this disease, Prof. He, Prof. Thomas D’Amico, and Prof. Xiuyi Zhi worked together with the international eminent specialists to publish the book Lung Cancer, arguably the first comprehensive textbook about lung cancer in the era of individualized treatment. The book is published in both Chinese and English languages. In the diagnosis and classification of lung cancers, the book discusses the application of gene sequencing. Clinically, lung cancer is classified based on not only cellular levels but also gene, DNA, RNA and micro RNA, which is helpful to diagnose and treat lung cancer. The individualized treatment marks a significant progress in disease diagnosis, both in medical and surgical oncology. The book also provides detailed introductions of many individualized treatment modes of lung cancer, especially in surgery. In the past decades, we deeply believed “same treatment for the same disease”. But now we found in the clinical practice that lung cancer can be further divided into different categories, such as genetic mutation. Lung cancer patients can also be divided into multiple groups, and surgeons are tasked to find the most effective solutions to reduce patients’ pains.
The book also underlines the development of individualized treatment in surgery, such as the application of non-intubated anesthesia, single port, and VATS. Twenty years ago VATS has not been widely popularized. Since 2005, however, a large number of clinical data from NCCN guideline have proven that VATS can treat lung cancer. After 20 years of research, we are pleased to find that individualized therapy, especially the use of VATS, can not only treat lung cancer but also prolong the patient’s overall survival time. Another example is that we found several years ago that minimally invasive surgeries can prolong lung cancer patients’ survival time by at least 3.5 months. That suggests minimally invasive surgeries can provide more health benefits to patients than being effective against tumors. At present, peripheral lung tumors, and even central lung tumors, are treatable. Complicated resections, such as removing bulges and double sleeve lobectomy, can be completed with the help of an endoscope. A more precise thoracoscope even enables segmentectomy. In the era of “precision medicine”, we hope this book can inspire surgeons and medical researchers to come up with innovative ideas to fight lung cancer. This book is just the beginning, and we hope a second and even a third version can be published later so that we can reach more consensuses on the disease and offer more meaningful guidance in clinical practice.
Patient demand and therapeutic effectiveness is the ultimate goal
Prof. He has been keeping a passionate and innovative mind, whether in the operating room or at medical forums or workshops. “I’m driven by the ultimate goal of meeting patient demand and maximizing the therapeutic effectiveness, and that goal will be constantly elevated, from patient demand/therapeutic effectiveness to shortening postoperative recovery time, reducing pain, and decreasing the duration of pain, along with advances in scientific research and technological development,” Prof. He said, “We need to think how to improve every procedure, and that is every doctor’s ultimate goal.”
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.


