
Laparoscopic versus open hemihepatectomy: a 1:1 matched analysis
Introduction
Laparoscopic liver resection was firstly reported in 1990s (1). The use of laparoscopic liver resection for liver lesions is increasing rapidly after dozens of years of exploration by liver surgeons (2-4). The First International Consensus Conference on Laparoscopic Liver Surgery was held in Louisville in 2008 (5). Since then, the reported number of laparoscopic liver resections has increased rapidly and procedure has almost extended to all the types of liver resection. On the Second International Consensus Conference on Laparoscopic Liver Resections which held in Japan in 2014, the status of laparoscopic liver resection was evaluated by 34 experts and a 9-member jury based on reported outcomes of laparoscopic liver resection (6). The jury finally concluded that minor liver resections had become standard practice and that major liver resections, such as hemihepatectomies, were still innovative procedures in the exploration phase and continued cautious introduction of major laparoscopic liver resections was recommended. In Sir Run Run Shaw Hospital, laparoscopic hemihepatectomies (LHs) had been performed as routine procedures for liver lesions in the past decade and a series of patients had been accumulated. Results of these patients were analyzed to evaluate the safety of laparoscopic major liver resection performed as routine procedures in medical centers with experiences in liver surgery and laparoscopic surgery.
Methods
Inclusion criteria for LH
The inclusion criteria for LH have been standardized in Sir Run Run Shaw Hospital, which included: unilateral liver lesion having the indication of hemihepatectomy; liver function of child A to B classification; no extrahepatic bile duct stricture or suppurative cholangitis in patients of hepatolithiasis; no past history of cholangiojejunostomy. In patients with liver malignancy, those who were diagnosed with tumor invasion in or close to the hepatic hilum or the hepatic venous trunk, cancer embolus in the main portal vein or the vena cava, or adjacent organ invasion by preoperative computed tomography (CT) or magnetic resonance imaging (MRI) were excluded.
Patient were excluded: who proceeded associating liver partition and portal vein ligation for staged hepatectomy (ALPPS); simultaneous bilateral liver resection; Simultaneous resection of other organs during the operation; undergoing biliary-enteric anastomosis during the operation; those who with incomplete data.
Procedure
In the LH group, LH was performed as described in previous articles (7,8). Briefly, patients were placed in a supine position under general anesthesia. Four entries were made and liver lesions were located by the direct vision and the laparoscopic ultrasonography. Laparoscopic selective inflow occlusion was performed before the liver transection. The laparoscopic multifunctional operative dissector (LPMOD) was used as the major instrument for transecting the liver parenchyma. Vessels and bile duct were dissected with LPMOD and were ligated with titanic clips, absorbable clips, ham-locks or laparoscopic linear staples. The integral specimen was packed into a plastic bag and was removed via an incision of 4–6 cm.
In the open hemihepatectomy (OH) group, a reverse L-shaped incision was made and Peng’s multifunctional operative dissector (PMOD) was used as an instrument for liver transaction and the manner of liver transection was similar to the LH. Vessels and bile duct were ligated with sutures. All the operations were performed by surgeons who have at least 3-year experience of laparoscopic or OH.
Patients
Patients underwent laparoscopic or OH in Sir Run Run Shaw Hospital from January 2012 to December 2017 were reviewed. These patients had a completely preoperative medical evaluation including liver function, cardiovascular and pulmonary assessment. Preoperative CT scan or MRI was done to locate the liver lesions accessing the feasibility of laparoscopic resection. All patients who met the inclusion criteria for LH were included for matching.
Study design
Each patient who underwent LH was individually matched with one control patient who underwent OH. A case-matched study was performed according to the same gender, age, diagnosis, procedure, liver cirrhosis, child classification, tumor size, branch of portal vein invasion, hepatic vein invasion and pre-operative transarterial chemoembolization (TACE). Patients who failed to be matched were excluded from the analyses.
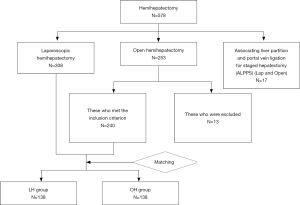
Total of 578 patients underwent hemihepatectomy during the period including 308 LH, 253 OH and 17 ALPPS. One hundred and thirty-eight pairs of patients were matched and constituted LH group and OH group. The detailed flowchart was shown in Figure 1.
Statistical analysis
Categorical data were presented as frequency (percentage) and were compared by Pearson Chi-square test or Fisher’s exact test (n≤40 or n≥40 but 1≤T<5). Continuous variables were presented as mean ± standard deviation and were compared by paired-samples t-test. All tests were two-tailed and P<0.05 was considered statistically significant. All analyses were performed with SPSS (IBM SPSS Statistics, Version 20.0).
Results
Patients characteristics
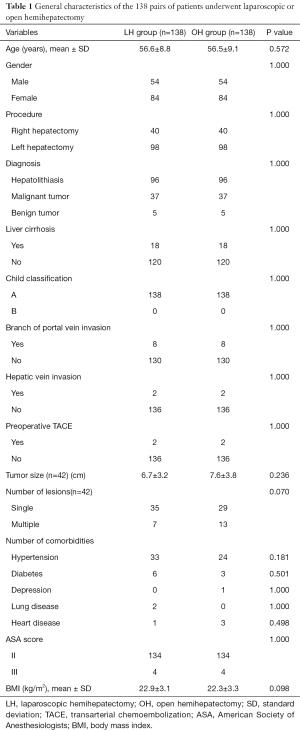
Total of 54 males and 84 females were included in each group. There was no significant difference of the age between LH group and OH group (56.6±8.8 vs. 56.5±9.1 years, P=0.572). Characteristics of the 138 pairs of patients are shown in Table 1.
Full table
Perioperative outcomes
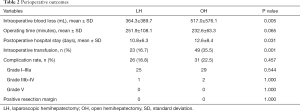
The length of postoperative hospital stay of the LH group was significantly shorter than the OH group. Intraoperative blood loss and transfusion rate in the LH group were significantly lower than the OH group. No significant differences of operating time and complication rate were found between the two groups. There is no positive resection margin found in patients (Table 2).
Full table
Complications
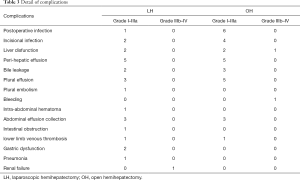
According to the Clavien-Dindo classification of surgical complications (9), total of 26 patients (18.8%) had complications in the LH group including 24 Grade I–IIIa complications and 1 Grade IIIb–V complication, and 31 patients (22.5%) had complications in the OH group including 29 Grade I–IIIa complications and 2 Grade IIIb–V complication. Details of these complications are shown in the Table 3. There was one severe complication, acute renal failure (Grade IV), occurred in LH group and he recovered uneventfully after 3 days of continuous renal replacement therapy in the intensive care unit. Two severe complications, a liver dysfunction (Grade IV) and a bleeding (Grade IIIb), occurred in the OH group. One and a half months of supporting therapy including ICU management was administrated on the patient with liver dysfunction. Laparotomy was performed on the patient with bleeding. All the three patients with severe complications were recovered uneventfully. Two patients in the LH group and 3 patients in the OH group had bile leakage. All of them were treated by percutaneous drainage. One patient in the LH group was found having a hematoma close to the raw surface and vital signs of the patient were stable. The patient was observed without any further treatment. There was no mortality in either group and all these patients with complications recovered uneventfully after immediate treatment.
Full table
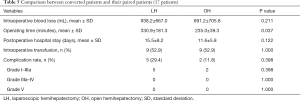
Conversions
Out of the 138 patients in LH group, 17 patients were converted to open procedures. Causes of these conversions were showed in the Table 4. Characteristics of the 17 pairs of patients are shown in Table S1. Three patients had massive bleeding and emergent conversions were carried out immediately. Results of these converted patients were compared to their paired patients in the OH group. The operating time of converted patients was significantly longer than their paired patients, but there was no significant difference in blood loss, transfusion rate, length of postoperative hospital stay and complication rate (Table 5).

Full table

Full table
Full table
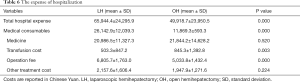
Cost
The expense of hospitalization in the LH and the OH group were showed in the Table 6. The hospital expense of LH group was significantly higher than the OH group. The cost of medical consumables and the operation fee of LH group were significantly higher than the OH group, but no significant differences of medicine cost and other treatment cost was found between the two groups.
Full table
Discussion
Laparoscopic local resection of liver lesion was firstly reported in 1991 (1) and it is still the major procedure of laparoscopically non-anatomical liver resection now. Left lateral segmentectomy is the major procedure of laparoscopically anatomical liver resection. It was recommended as a routine procedure by the first international expert consensus on laparoscopic liver resection (5). Some procedures, including isolated caudate lobectomy, trisegmentectomy and middle hepatic lobectomy (segments 4, 5, and 8), are rarely performed even in experienced institutes because of technique difficulties and the risk of massive bleeding (10,11). For tumors located in segment VII and VIII, normal laparoscopic instruments are difficult to reach, but it could be resected laparoscopically by experienced surgeons or with special instruments such as trans-thoracic laparoscopic devices (12-15). Laparoscopic major liver resection including left hemihepatectomy and right hemihepatectomy were performed in some institutes, but it is still in controversy. Experts of laparoscopic liver resection still could not reach a consensus on its outcomes and cost because of the lack of high or moderate quality evidence from clinical practice (5,6). However, LH is still a promising procedure even for patients with liver cirrhosis (16). Laparoscopic hemihepatectomies have been performed as a routine procedure in our institute for a decade. Here we tried to provide some evidences on the potential value of this procedure by performing the 1:1 matched study between LH and OH.
According to the definition of major hepatectomy, it includes the resection of 3 or more Couinaud segments (6,17). Some experts have the resection of right posterior section or anterior section included in major hepatectomy because of the unique techniques required (18). In our institute, the majority of laparoscopic liver resection of 3 or more Couinaud segments was hemihepatectomy and laparoscopic extended hemihepatectomy did not be performed routinely for the risk of intraoperative massive bleeding. Indications for laparoscopic major hepatectomy included hepatolithiasis, hepatocellular carcinoma, metastatic liver cancer, cholangiocarcinoma and benign tumors. Hepatolithiasis is a prevalent liver disease in eastern China where our institute is located in and hemihepatectomy is the most common procedure for this disease (19,20). A large number of patients underwent hemihepatectomy for this disease in our institute.
In 2009, we had reported the initial experience of LH as well as the learning curve of this procedure (8). With the accumulation of experience on this procedure, laparoscopic left and right hemihepatectomy became a routine procedure in our institute and surgical results might be improved, so we collected the data in recent years and compared it with OH by the matched method for the potential value of the procedure. In this study, the blood loss and transfusion rate of LH group was significantly lower than the OH group. The magnification of operating area by the laparoscope as well as the meticulous dissection could explain these results. Vessels in the transection plane could be clearly observed in laparoscope and were meticulously freed and ligated by experienced laparoscopic surgeons. Blood loss, as well as the possibility of massive bleeding, decreased as the consequence of less injury of vessels. There was no difference of mortality and morbidity between the LH group and the OH group. Complications were classified according to the Clavien-Dindo classification (9). Three patients had severe complications and need ICU management or re-operation under general anesthesia. All patients with complications recovered uneventfully after immediate treatments. According to these results, LH could be as safe as OH if performed in an experienced laparoscopic center. In this study, LH still had merits of laparoscopic surgery over conventional open surgery. The length of postoperative hospital stay was decreased and the incision was minimized.
Previously, Cleary et al. had reviewed published literatures and found that the overall cost of laparoscopic liver resection was less than open liver resection because of the short hospital stay and the evidence was strongest for minor hepatic resection (21). In this study, cost did not decrease along with the decreased length of postoperative hospital stay, on the contrary, the hospital expense of LH group was significantly higher than the OH group. The cost of medical consumables and operation fee were significantly higher in the LH group as compared to the OH group that lead to a high hospital cost of laparoscopic hemihepatectomies. The use of kinds of clips and more linear staples for ligating blood vessels and bile duct in laparoscopic surgery, as well as disposable trocars, could be the major reason for the high cost of medical consumables in the LH group. The high operation fee in LH group could be explained by the charge policy in which charge of a laparoscopic surgery is higher than its open equivalent. Lower transfusion rate in the LH group could explain the lower transfusion fee in LH group compared with the OH group.
Recently, there is a multicenter retrospective study published in 2019 by Cipriani et al. containing 545 pairs of laparoscopic and open hemihepatectomies from nine European referral centers after propensity score matching. They found that Laparoscopy was associated with reduced blood loss, postoperative stay and minor morbidity (22). Our study found that the length of postoperative hospital stay of LH group was significant shorter than the OH group (P=0.031). Intraoperative blood loss (P=0.005) and transfusion rate (P=0.001) in the LH group were significantly lower than the OH group which were consistent with their results.
In the second international consensus conference on laparoscopic liver resection in Morioka, a hot debate on the value of laparoscopic living donor hepatectomy occurred between experts and the jury and they failed to reach a consensus on this procedure. The point of the debate was whether surgeons could convert to open in time and finish the operation without a severe consequence. In this study, 17 patients converted to open. As compared to their paired patients in OH group, no significant difference in blood loss and transfusion rate was found. The operating time of converted patients was significantly longer than their paired patients. No mortality or severe complication occurred in these converted patients. These results led us to believe that conversion should not increase the surgical risk as compared with OH and the importance of a judicious surgical attitude toward conversion, which means surgeons should master the timing of conversion to open surgery during laparoscopic liver resection. Cipriani et al. in 2019 confirmed some associated advantages of laparoscopic and highlighting the need for realistic expectations of the minimally invasive approach based on the resected hemiliver and the patients treated (22).
Conclusions
The results of this study lead us to believe that LH is a safe procedure as OH and could be performed routinely in experienced laparoscopic centers. Use of laparoscopic technique for hemihepatectomy could increase the hospital expense as the consequence of using high cost of medical consumables.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.188). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Institutional Review Board of the Sir Run Run Shaw Hospital of Zhejiang University approved protocols of the study (No. 2020-373-01). Informed consent was taken from all the patients
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Reich H, McGlynn F, Decaprio J, et al. Laparoscopic excision of benign liver lesions. Obstet Gynecol 1991;78:956-8. [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection. Ann Surg 2016;263:761-77. [PubMed]
- Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann Surg 2018;268:11-8. [Crossref] [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Cai X, Duan L, Wang Y, et al. Laparoscopic hepatectomy by curettage and aspiration: a report of 855 cases. Surg Endosc 2016;30:2904-13. [Crossref] [PubMed]
- Cai XJ, Wang YF, Liang YL, et al. Laparoscopic left hemihepatectomy: a safety and feasibility study of 19 cases. Surg Endosc 2009;23:2556-62. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Morise Z. Laparoscopic liver resection for posterosuperior tumors using caudal approach and postural changes: A new technical approach. World J Gastroenterol 2016;22:10267-74. [Crossref] [PubMed]
- Ikeda T, Toshima T, Harimoto N, et al. Laparoscopic liver resection in the semiprone position for tumors in the anterosuperior and posterior segments, using a novel dual-handling technique and bipolar irrigation system. Surg Endosc 2014;28:2484-92. [Crossref] [PubMed]
- Ichida H, Ishizawa T, Tanaka M, et al. Use of intercostal trocars for laparoscopic resection of subphrenic hepatic tumors. Surg Endosc 2017;31:1280-6. [Crossref] [PubMed]
- Okuno M, Goumard C, Mizuno T, et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 2018;32:1776-86. [Crossref] [PubMed]
- Coelho FF, Kruger JAP, Fonseca GM, et al. Laparoscopic liver resection: Experience based guidelines. World J Gastrointest Surg 2016;8:5-26. [PubMed]
- Aikawa M, Miyazawa M, Okamoto K, et al. Thoracoscopic hepatectomy for malignant liver tumor. Surg Endosc 2014;28:314. [Crossref] [PubMed]
- Yoon YI, Kim KH, Kang SH, et al. Pure Laparoscopic Versus Open Right Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Propensity Score Matched Analysis. Ann Surg 2017;265:856-63. [Crossref] [PubMed]
- Reiniers MJ, Olthof PB, van Golen RF, et al. Hypothermic perfusion with retrograde outflow during right hepatectomy is safe and feasible. Surgery 2017;162:48-58. [Crossref] [PubMed]
- Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. Ann Surg 2013;257:205-13. [Crossref] [PubMed]
- Cai X, Wang Y, Yu H, et al. Laparoscopic hepatectomy for hepatolithiasis: A feasibility and safety study in 29 patients. Surg Endosc 2007;21:1074-8. [Crossref] [PubMed]
- Jin R-A, Wang Y, Yu H, et al. Total laparoscopic left hepatectomy for primary hepatolithiasis: Eight-year experience in a single center. Surgery 2016;159:834-41. [Crossref] [PubMed]
- Cleary SP, Han HS, Yamamoto M, et al. The comparative costs of laparoscopic and open liver resection: a report for the 2nd International Consensus Conference on Laparoscopic Liver Resection. Surg Endosc 2016;30:4691-6. [Crossref] [PubMed]
- Cipriani F, Alzoubi M, Fuks D, et al. Pure laparoscopic versus open hemihepatectomy: a critical assessment and realistic expectations - a propensity score-based analysis of right and left hemihepatectomies from nine European tertiary referral centers. J Hepatobiliary Pancreat Sci 2020;27:3-15. [Crossref] [PubMed]


