
The analysis of risk for peptic ulcer disease using Korean national health and nutrition examination survey: a cross-sectional analysis of a national survey sample
Introduction
Although the fact that the etiology of peptic ulcer disease (PUD) is multifactorial is widely known, relative impact of each risk factors is not well studied. After the discovery of Helicobacter pylori (HP) infection, the causes, pathogenesis, and treatment of PUD have been rewritten (1). Among environmental factors, cigarette smoking is well-known etiologic factor that have a close relationship with PUD (2,3). Alcohol consumption has been presumed to be associated with PUD. The inflammatory changes are likely to be related to concurrent HP infection that is common among alcoholics (4). The aim of this prospective, Korean population-based study using the data from Korea National Health and Nutrition Examination Survey (KNHANES) was to estimate the effect of environmental and social factors and on the risk of subsequent PUD.
Methods
Data resource
KNHANES is a national surveillance system that collets the health and nutritional status of Koreans since 1998. In this study, the data from the KNHANES between 2008 and 2009 by the Division of Chronic Disease Surveillance under the Korea Centers for Disease Control and Prevention and the Korean Ministry of Health and Welfare were used (5). KNHANES is a research for non-institutionalized civilians across the country that used a stratified and multi-stage probability sampling design with a rolling survey-sampling model (6). The sampling units were based on the population and housing consensus from the 2005 National Census Registry in Korea, which includes age, sex, and geographic area (7). The survey was divided into three sections: a health interview survey, a health examination survey, and a nutrition survey. At the mobile examination center, physical examinations, blood sampling, and urine sampling were done (5,6). Ethical approval was waived from institutional review board because study used data of national survey sample.
Demographic variables
Alcohol intake, regular exercise, educational status, medical history including PUD, and smoking status were used as demographic variables. Individuals with the lowest household incomes were designated as the low income group (5). When the respondent did not graduate middle school, the education level was classified as low. Individuals were also divided into three groups: non-smokers, ex-smokers, and current smokers. If the individuals exercise for at least 20 minutes at a time for at least three times a week, they were classified as regular exercise group.
Data psychological stress was evaluated from responses indicative of cognitive complaints collected with a questionnaire using a 4-point Likert scale as follows: 1 (very severe), 2 (severe), 3 (moderate), and 4 (low). Meaningful cognition of stress was defined as psychological stress rated as more than severe (scale 1 or 2). Participants who answered “yes” to the question, “During the past year, has your daily life been burdened by feelings of hopelessness or dejection for more than 2 continuous weeks?” were categorized as having depressed mood. When the individuals had thoughts of committing suicide for the past year, they were designated as suicidal ideation group. To gather the data about residential place (rural versus urban) and occupation, a face-to-face interview was done (8).
Anthropometric measurements and biochemical measurements
The measurements of the participants were carried out by staff who was trained in the Division of Chronic Disease Surveillance under the Korea Centers for Disease Control and Prevention and the Korean Ministry of Health and Welfare (6). Weight was measured to the nearest 0.1 kg with participants wearing light indoor clothing, and height was measured to the nearest 0.1 cm without wearing shoes (7). Waist circumference was measured at the narrowest point between the lower border of the rib cage and the iliac crest (6). Body mass index (BMI) was calculated using the following formula: weight/height2 (kg/m2), standard mercury sphygmomanometer was carried out a blood pressure on the right arm. It was used in the analysis of the average value between 5 minutes measurements. A blood sample was collected after fasting for at least 8 hours to measure the serum fasting plasma glucose levels (FBG), total cholesterol, high density lipoprotein cholesterol (HDL-C), triglyceride recovery of (TG) from the pole vein of each participant, and insulin, serum D. Serum 25-hydroxy vitamin D blood samples were appropriately refrigerated, transported, and processed immediately at the Central Testing Institute (Seoul, Korea). Blood samples were analyzed within 24 hours of transportation.
Definition of disease categories
The presence of PUD is determined by the health interview survey based on history of endoscopic diagnosis and its treatment. Metabolic syndrome was defined based on the American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement criteria for Asians (6). Metabolic syndrome, the diagnosis can be made in three or more of the following conditions are met: waist circumference ≥90 cm for men and ≥80 cm for women; fasting TG ≥150 mg/dL or use of lipid-lowering medication; HDL-C <40 mg/dL in men and <50 mg/dL in women or use of medication; blood pressure ≥130/85 mmHg medication or use of antihypertensive medication; and FBG ≥100 mg/dL or current use of anti-diabetes medication (5). Diabetes was diagnosed when fasting blood sugar was >126 mg/dL or when the individual was currently using anti-diabetic medications. Systolic blood pressure higher than 160 mmHg and diastolic blood pressure higher than 90 mmHg, or usage of antihypertensive medication was defined as systemic hypertension (2).
Statistical analyses
All data are presented as mean ± standard error or as % (percent or proportion). Logarithmic transformation was performed to achieve a normal distribution, when necessary. P values <0.05 indicate the statistical significance. Student’s t-test was employed to compare paired continuous variables. To assess the differences in presence of PUD according to the variables, Chi-squire exact test was used. Multiple logistic regression model was used to assess the risk of PUD. A multiple logistic regression is a logistic regression with only one response but several predictors. In this study predicting PUD status (positive or negative) using the number of factors as possible predictors. The various potential risk factors for an outcome were identified, and stepwise logistic regression models (3 models) were constructed for the PUD status variable using Akaike’s Information Criterion (AIC) model selection to maximize model fit (7). Otherwise, age was adjusted for Model 1, the same variables as Model 1 in addition to socio-economic factors for Model 2, the same variables as Model 2 with the mental health factors for Model 3. Odds ratios and 95% confidence intervals were estimated after the adjustment for potential confounders (7). Statistical analyses were performed using the survey procedure of the statistical software package SAS 9.2 to account for the complex sampling design.
Results
Study population
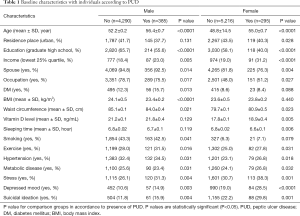
Total of 20,277 individuals who were available for entire data set were used for this study. Among 20,277, 5,206 less than 19 years old populations were excluded and legal adult in Korea were only included in the primary cohort. Among 15,071 individuals, non-responders who reported having had a PUD before study entry (n=4,885) were also excluded. Finally, 10,166 individuals were included for this investigation. A total of 10,166 adults were included in this study and Table 1 describes the characteristics of the study population by PUD status and gender. Among 10,186 individuals, there were 4,675 males and 5,511 (54.1%) females. 385 (8.2%) males among 4,675 had a PUD and 4,290 (91.8%) did not have. Female PUD population was 295 (5.4%) and without PUD were 5,216 (94.6%).
Full table
Baseline characteristics of male population
Men with PUD were significantly older and showed lower education level and income. BMI and waist circumference are lower in PUD group in male populations (P<0.0001, P=0.021, respectively). They showed more vulnerable psychiatric indexes: stress recognition, depression recognition, and suicidal thoughts (P=0.026, P=0.026, P=0.034, respectively) (Table 1).
Baseline characteristics of female population
Women PUD group significantly older (P<0.0001) and more likely to be lower level of education, income (P=0.0006, P<0.0001, respectively). PUD population in female significantly more to be solo (P=0.0311) and had larger proportion of each psychiatric index with higher levels: stress recognition (P=0.0063), depression recognition P<0.0001), and suicidal thoughts (P=0.0005). Their waist circumferences were longer (P=0.0232) and vitamin D level was higher than those of non-PUD population (P=0.0047). Their sleeping time was shorter than those of non-PUD population (P=0.006) (Table 1).
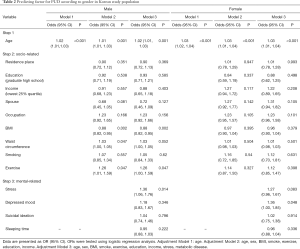
Risk for PUD on both genders using multiple logistic regression model
We examined 3 models adjusted for different variables. Table 2 shows adjusted odds ratios (ORs) and their 95% confidence intervals (CIs) from multiple logistic regression analyses controlling for age in Model 1; Model 1 add socio-economic and physical factors in Model 2; Model 2 add Mental health factors in Model 3. On both gender, older age was significant risk for PUD in all three models. In male, lower BMI and stress was significant risk for PUD. Older age and episode of depressed mood were risk for PUD in female group.
Full table
Discussion
We demonstrated significant association between mental health and PUD in a nationally representative sample of Korean population. In male, psychological stress was significant risk for PUD, and episode of depressed mood was risk in Korean women. Mental health problems were significantly associated with the history of PUD even after the adjustment of other risk factors such as age, socio-economic status, and physical status.
Each PUD risk factors has different influence on the ulcer occurrence in general populations and also in other parts of the world (9).
In this study, lower income and lower level of education were associated with higher incidence of PUD in univariate analysis on both genders. However, anything of objective evidence was not available on socioeconomic factors such as income, educational grades. HP infection is a widely known major cause for PUD (10-12).
As low educational background increased the risk, social strains, lifestyle and diet habits consists of the multifactorial etiology of peptic ulcer (13). Although the prevalence of HP has decreased in other developed countries, it still remains high in Korea (14-17).
According to the nationwide seroprevalence surveys in 1998 and 2005 among asymptomatic Korean adults, HP prevalence had rates of 66.9% and 59.5% (16). As HP infection is generally more frequent in developing and underdeveloped countries than in developed countries, the socioeconomic status is presumed to play an important role in HP infection (18,19). However, it was impossible to present HP infection rate in this study, because the data was not derived from medical records but nationwide survey.
Previous studies found that there was a relationship between PUD and psychological problems especially stress. For example, after the disastrous Hanshin-Awaji earthquake in the southern part of Hyogo, Japan, which killed more than 6,000 people, incidence of bleeding ulcer increased (20). Japanese group also reported that stress is an important predictor in a multivariable model along with HP, nonsteroidal anti-inflammatory drugs, socioeconomic status, and smoking (21). Despite the increased knowledge regarding the pathogenesis of PUD, the decreasing prevalence of HP infection in the Western societies, and the increased availability of effective therapies, approximately 5% and 20% of patients develop PUD without any identifiable cause and the burden of disease remains high (22,23). Danish study (24) reported that psychological stress results in health risk behaviors, increasing the incidence of peptic ulcer. Whether ulcers were associated with HP or not, stress had similar effects. It also increased the risk for both gastric and duodenal ulcers, with the adjusted odds ratio of 1.19 per point in gastric ulcers and 1.11 in duodenal ulcers (24).
Despite it was impossible to present the stress in quantitative analysis, our study presented the mental health problem using survey which was stratified by scale and three categories such as stress, depressed mood and suicidal thoughts. Our investigation may be different and specific in comparison with the previous studies with regards to measurement of mental health problem. And we could reveal that mental health problem was associated with PUD different somewhat between genders.
Possible pathologic mechanisms for the development of PUD due to mental health problems have been suggested in several previous studies. Stress may enhance the peptic ulcer through increasing the acid load, and starting the activation of hypothalamic-pituitary-adrenal axis (HPA) on healing, altered blood flow, or cytokine-mediated impairment of mucosal defenses (25-28). Enteric Nervous System plays an important role in the regulation of the physiological gut functions. The identification of corticotropin-releasing factor (CRF) and the development of specific CRF receptor antagonists helped to analyze the neurochemical basis of the stress response (29) in three key mechanisms: (I) stress is perceived and processed by higher brain centers; (II) the brain collects a neuroendocrine response by way of the HPA and the autonomic nervous system (ANS), and (III) the brain activates feedback mechanisms by stimulating HPA and ANS to restore homeostasis (29). Although many contributing factors are enumerated though literatures review, the mechanism correlating difference between age prevalence is still not clear. Moreover, the results supporting those mechanisms showed uneven and scarce until now. So, it will be subject which we must reveal the cause and effect precisely in future.
Additionally, a key confounding variable of NSAID use is not captured by the analysis; chronic pain may be a psychological manifestation of distress and be treated with NSAID. Unfortunately, it is just survey based on Questionnaire by healthy persons, so it is impossible or inaccurate to check it. It is unclear the hypothesis that associations may differ for men and women because we didn’t check it by statistical evaluation.
This study is conducted upon the nationally representative samples of Korean with sufficient power for investigation of these relationships and additional information availability of relevant confounding factors (30) while cross-sectional studies may not be able to clarify explicit cause-and-effect relationships as this study only reflects a single moment in time. This study does not take consideration of past and future moment of the survey. Cross-sectional studies results may be also exaggerated by recall bias and by the distressing effects of disease (31). It seems the survey asked for present symptoms/status of the respondent, who was also asked to report retrospectively whether they had had a diagnosis of PUD. It is main limitation that the present health status may be a consequence of the condition, rather than a causative factor.
Despite limitation, present study offers new information that Koreans who have mental health problem were more likely to have a higher prevalence of PUD regardless of their age, socioeconomic factors, systemic conditions in multivariable adjusted models. In the future, further prospective studies are needed to confirm this relationship and to test possible underlying mechanisms.
In conclusion, in Korean, mental health is associated with an increased prevalence of PUD.
Acknowledgments
This study was funded by research grant from Institute of Clinical Medicine Research in the Catholic University of Korea, Yeouido St. Mary’s Hospital.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.126). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethical approval was waived from institutional review board because study used data of national survey sample.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet 2009;374:1449-61. [Crossref] [PubMed]
- Friedman GD, Siegelaub AB, Seltzer CC. Cigarettes, alcohol, coffee and peptic ulcer. N Engl J Med 1974;290:469-73. [Crossref] [PubMed]
- Kato I, Nomura AM, Stemmermann GN, et al. A prospective study of gastric and duodenal ulcer and its relation to smoking, alcohol, and diet. Am J Epidemiol 1992;135:521-30. [Crossref] [PubMed]
- Nagata N, Niikura R, Sekine K, et al. Risk of peptic ulcer bleeding associated with Helicobacter pylori infection, nonsteroidal anti-inflammatory drugs, low-dose aspirin, and antihypertensive drugs: a case-control study. J Gastroenterol Hepatol 2015;30:292-8. [Crossref] [PubMed]
- Kim YH, Cho KH, Choi YS, et al. Low bone mineral density is associated with metabolic syndrome in South Korean men but not in women: The 2008-2010 Korean National Health and Nutrition Examination Survey. Arch Osteoporos 2013;8:142. [Crossref] [PubMed]
- Park JB, Han K, Park YG, et al. Association between alcohol consumption and periodontal disease: the 2008 to 2010 Korea National Health and Nutrition Examination Survey. J Periodontol 2014;85:1521-8. [Crossref] [PubMed]
- Nam GE, Kim DH, Cho KH, et al. 25-Hydroxyvitamin D insufficiency is associated with cardiometabolic risk in Korean adolescents: the 2008-2009 Korea National Health and Nutrition Examination Survey (KNHANES). Public Health Nutr 2014;17:186-94. [Crossref] [PubMed]
- Lee K.. Body composition and vitamin D status: the Korea National Health And Nutrition Examination Survey IV (KNHANES IV). J Hum Nutr Diet 2013;26 Suppl 1:105-13. [Crossref] [PubMed]
- Schlemper RJ, van der Werf SD, Vandenbroucke JP, et al. Risk factors of peptic ulcer disease: different impact of Helicobacter pylori in Dutch and Japanese populations? J Gastroenterol Hepatol 1996;11:825-31. [Crossref] [PubMed]
- Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1983;1:1273-5. [PubMed]
- Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7-14 June 1994. IARC Monogr Eval Carcinog Risks Hum 1994;61:1-241. [PubMed]
- NIH Consensus Conference. Helicobacter pylori in peptic ulcer disease. NIH Consensus Development Panel on Helicobacter pylori in Peptic Ulcer Disease. JAMA 1994;272:65-9. [Crossref] [PubMed]
- Johnsen R, Forde OH, Straume B, et al. Aetiology of peptic ulcer: a prospective population study in Norway. J Epidemiol Community Health 1994;48:156-60. [Crossref] [PubMed]
- Jung JH, Choi KD, Han S, et al. Seroconversion rates of Helicobacter pylori infection in Korean adults. Helicobacter 2013;18:299-308. [Crossref] [PubMed]
- Lim SH, Kwon JW, Kim N, et al. Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol 2013;13:104. [Crossref] [PubMed]
- Yim JY, Kim N, Choi SH, et al. Seroprevalence of Helicobacter pylori in South Korea. Helicobacter 2007;12:333-40. [Crossref] [PubMed]
- Kim JH, Kim HY, Kim NY, et al. Seroepidemiological study of Helicobacter pylori infection in asymptomatic people in South Korea. J Gastroenterol Hepatol 2001;16:969-75. [Crossref] [PubMed]
- Graham DY, Adam E, Reddy GT, et al. Seroepidemiology of Helicobacter pylori infection in India. Comparison of developing and developed countries. Dig Dis Sci 1991;36:1084-8. [Crossref] [PubMed]
- Pounder RE, Ng D. The prevalence of Helicobacter pylori infection in different countries. Aliment Pharmacol Ther 1995;9 Suppl 2:33-9. [PubMed]
- Aoyama N, Kinoshita Y, Fujimoto S, et al. Peptic ulcers after the Hanshin-Awaji earthquake: increased incidence of bleeding gastric ulcers. Am J Gastroenterol 1998;93:311-6. [Crossref] [PubMed]
- Kurata JH, Nogawa AN. Meta-analysis of risk factors for peptic ulcer. Nonsteroidal antiinflammatory drugs, Helicobacter pylori, and smoking. J Clin Gastroenterol 1997;24:2-17. [Crossref] [PubMed]
- Konturek SJ, Bielanski W, Plonka M, et al. Helicobacter pylori, non-steroidal anti-inflammatory drugs and smoking in risk pattern of gastroduodenal ulcers. Scand J Gastroenterol 2003;38:923-30. [Crossref] [PubMed]
- Konturek PC. Physiological, immunohistochemical and molecular aspects of gastric adaptation to stress, aspirin and to H. pylori-derived gastrotoxins. J Physiol Pharmacol 1997;48:3-42. [PubMed]
- Levenstein S, Rosenstock S, Jacobsen RK, et al. Psychological stress increases risk for peptic ulcer, regardless of Helicobacter pylori infection or use of nonsteroidal anti-inflammatory drugs. Clin Gastroenterol Hepatol 2015;13:498-506.e1. [Crossref] [PubMed]
- Peters MN, Richardson CT. Stressful life events, acid hypersecretion, and ulcer disease. Gastroenterology 1983;84:114-9. [Crossref] [PubMed]
- Takeuchi K, Furukawa O, Okabe S. Induction of duodenal ulcers in rats under water-immersion stress conditions. Influence of stress on gastric acid and duodenal alkaline secretion. Gastroenterology 1986;91:554-63. [Crossref] [PubMed]
- Kiecolt-Glaser JK, Marucha PT, Malarkey WB, et al. Slowing of wound healing by psychological stress. Lancet 1995;346:1194-6. [Crossref] [PubMed]
- Arakawa T, Watanabe T, Fukuda T, et al. Ulcer recurrence: cytokines and inflammatory response-dependent process. Dig Dis Sci 1998;43:61S-6S. [PubMed]
- Bhatia V, Tandon RK. Stress and the gastrointestinal tract. J Gastroenterol Hepatol 2005;20:332-9. [Crossref] [PubMed]
- Chung W, Lim S, Lee S. Why is high-risk drinking more prevalent among men than women? Evidence from South Korea. BMC Public Health 2012;12:101. [Crossref] [PubMed]
- Wilhelmsen I, Berstad A. Reduced relapse rate in duodenal ulcer disease leads to normalization of psychological distress: twelve-year follow-up. Scand J Gastroenterol 2004;39:717-21. [Crossref] [PubMed]


