
Interaction between delivery mode and maternal age in predicting overweight and obesity in 1,123 Chinese preschool children
Introduction
The past decades have witnessed a dramatic rise in the prevalence of pediatric overweight and obesity around the world (1). In China, an estimated 10% and 12% young children aged 2–6 years are separately classified as overweight and obese (2). The problem of pediatric overweight/obesity has received wide scientific attention, and we must expand this attention by developing effective strategies to curb this global problem. Hence, efforts to identify potential risk factors attributable to pediatric overweight/obesity must be proceeded.
Growing evidence indicates that cesarean delivery can increase the risk of overweight and obesity in childhood (3-6), whereas other studies failed to reveal any supportive evidence (7-9). Li and colleagues meta-analyzed the results of 9 studies, and found that relative to vaginal birth, cesarean delivery was significantly associated with a 33% increased risk of being overweight or obese in offspring (10). Another meta-analysis by Sutharsan and colleagues showed a relative risk of 1.15 for overweight and obesity due to cesarean delivery in early childhood (0 to 5 years), and a similar trend was noted for mid-childhood and adolescence (5 to 18 years) (11). Above evidence collectively indicates that cesarean delivery is a significant risk factor for pediatric overweight and obesity.
Additionally, pregnancy at advanced maternal age is common in both developed and developing countries (12). Some studies have shown that maternal age was closely related to cesarean delivery, and cesarean delivery rate increased consistently with advancing maternal age (12-14). Maternal age seemed to be the strongest predictor of cesarean delivery for the first birth of “low risk” women (15). In a cohort study, Triunfo and colleagues reported that maternal age had a significant and independent contribution to cesarean delivery rate (16). Maternal age not only increased the risk of cesarean delivery, but also associated with pediatric overweight and obesity. Although little research is available on the relationship between maternal age and pediatric obesity, the results of previous studies were inconsistent and inconclusive (17,18). A recent study indicated that the risk of overweight and obesity decreased with increasing maternal age (19). The role of delivery mode and maternal age, acting independently or in an interactive manner, in pediatric overweight and obesity is still unclear.
We here developed a hypothesis that delivery mode and maternal age might act interactively in predisposition to pediatric overweight and obesity. To verify the hypothesis, we examined the association of delivery mode and maternal age, both individually and interactively, with the risk of overweight/obesity among Chinese preschool children using data from a cross-sectional survey.
Methods
Study population
The cross-sectional study recruited preschool children aged 3–6 years from five kindergartens in Chaoyang District, Beijing during the period between March and May in 2017.
This study was approved by the Ethics Committee of China-Japan Friendship Hospital, and the parents or supervisors of all involved children provided written informed consent prior to participation.
Data collection and quality control
Using a stratified cluster random sampling strategy, 1,333 preschool-aged children were selected in this study, and data were collected by a pre-validated self-developed questionnaire. Initially, we collected 1,327 questionnaires, and after excluding questionnaires with invalid gender, body height, and weight, 1,123 validated questionnaires were left in the final analysis. Of all eligible preschool-aged children, 49.8% were boys and 50.2% were girls.
The parents or supervisors of all involved children were requested to complete the self-developed questionnaire to collect data on age of both children and parents, gender, weight, height, and birth weight of children, gestational age, cesarean delivery, feeding patterns, gravidity, parity, and breastfeeding duration, if available. Body weight and height of children and birth history were reported by their parents or supervisors. Gestational age was divided into <37 weeks, 37–42 weeks, and >42 weeks. Delivery mode included cesarean delivery and vaginal delivery. Feeding patterns were classified into breast feeding, mixed feeding, and artificial feeding. Gravidity was defined as a number of pregnancies, while parity was defined as the number of births. The dates of maternal and paternal birth were collected, and their parents’ age was calculated as the difference between the child’s date of birth and the date of the parents’ birth. Maternal age was divided as <28 years, 28–32 years, and >32 years by interquartile range, and paternal age was classified as <30 years, 30–35 years, and >35 years. In cases of children whose mother was dead, relevant data were not recorded and analyzed in this study.
There was strict quality control in process of questionnaires distribution and recovery, as described in our recent publication (20). We provided the same training on investigation methods to health physicians from five kindergartens before distributing questionnaires. The questionnaires were distributed to children and then to their parents or supervisors by kindergarten teachers who were responsible for distributing and collecting the questionnaires. After collecting the questionnaires, health physicians conducted the first check, and we double checked for questionnaires by telephone interview. In addition, questionnaires with missing or unreasonable data were returned to kindergarten teachers, who contacted parents to request or validate the relevant information.
Overweight and obesity definition
In this study, we calculated children’s body mass index (BMI) as weight (kg) divided by the square of height (m2). Overweight and obesity were defined by BMI using different criteria from the World Health Organization (WHO), the International Obesity Task Force (IOTF), and China, respectively (Table S1). In detail, for the WHO Child Growth Standards, we defined overweight and obesity by age- and sex-specific BMI z-scores and age was considered on account of a difference between over and under 5 years. Under 5 years old, overweight was defined as more than two standard deviations (SD) above the reference median, and obesity was defined as more than three SD (21). Over 5 years old, overweight was greater than one SD above reference median, and obesity was greater than two SD above reference median (22). In the IOTF criteria, we adopted international cut-off points for BMI for overweight and obesity by sex between 2 and 18 years (overweight as over BMI of 25 kg/m2; obesity as over BMI of 30 kg/m2 at age 18) (23). With the China criteria, we defined overweight and obesity as over BMI of 24 and 28 kg/m2 at age 18 respectively (24).

Full table
Statistical analyses
We classified all study children as non-overweight, overweight and obesity groups separately by BMI using the WHO, IOTF, and China criteria. We described categorical variables using count (percentage) and compared between two groups by the use of Chi-squared test. We described continuous variables using the median (interquartile range) comparing among groups by t-test or rank-sum test according to the normality of data distribution (conforming to a normal distribution by t-test, and otherwise by rank-sum test). For delivery mode and maternal age, we used the univariate and multivariable logistic regression model to examine the association with overweight and obesity, individually and interactively, before and after adjusting for age, gender, paternal age, gestational age, feeding patterns, gravidity, parity, breastfeeding duration, and birth weight. Additionally, we explored the interaction by conducting subgroup analysis between gender and age before and after other potential confounders.
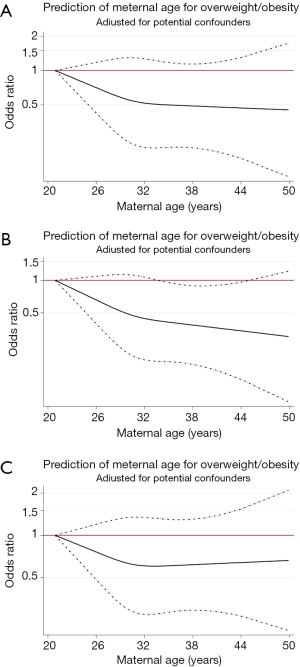
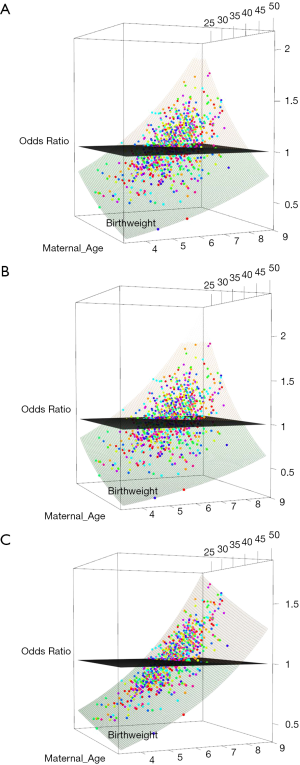
A restricted cubic spline regression model was fitted to delineate the association between maternal age and overweight/obesity risk among preschool children. To affiliate clinical explanation, we created a three-dimension interactive surface between maternal age and birthweight accounting for the predict risk of overweight and obesity by delivery mode and maternal age.
Three-dimension interactive surface was plotted using the “rgl.surface” program in the “rgl” package, which is a library of functions that offers three-dimensional, real-time visualization functionality to the R programming environment. The core of the “rgl” package is a shared library that acts as an interface between R and OpenGL.
Unless otherwise indicated, the STATA software Release 14.0 (Stata Corp, TX) were applied in statistical analyses. P value of less than 0.05 was considered as statistically significant.
Results
Prevalence of overweight/obesity in preschool children
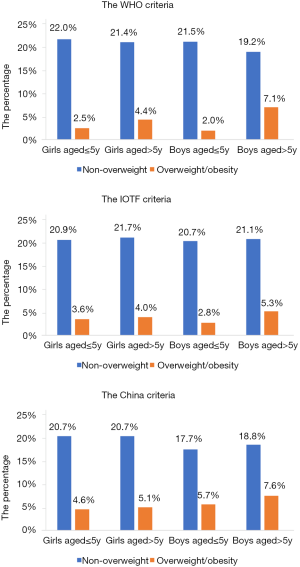
A total of 1,123 children based on gender and age were divided as four subgroups—girls aged ≤5 years, girls aged >5 years, boys aged ≤5 years, and boys aged >5 years groups. The prevalence of overweight and obesity in each subgroup under three growth criteria is described in Figure 1. High rates of overweight and obesity in a group of boys aged over 5 years were seen (WHO: 7.12%; IOTF: 5.25%; China: 7.57%).
Baseline characteristics
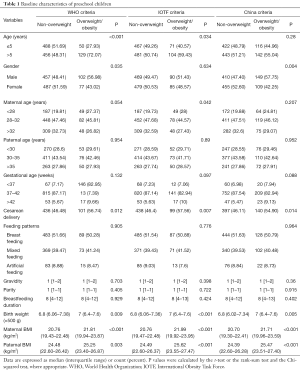
Age, gender, maternal age, paternal age, gestational age, delivery mode, feeding patterns, gravidity, parity, breastfeeding duration, and birth weight were obtained in baseline characteristics (Table 1). Age and gender showed inconsistent difference between the two groups under various growth references. The overweight and obese children born by cesarean delivery was 56.74%, 57.56%, and 54.90% in total overweight and obese children by WHO, IOTF, and China criteria. Compared with vaginal delivery, cesarean delivery rate in overweight and obese group was higher than that in non-overweight group, and reach the statistical difference under three criteria (all P<0.05). Birth weight in overweight and obese group was also high compared with that in non-overweight group, and achieve statistical difference among groups under three criteria (all P<0.05). The overweight and obese children with maternal age <28 years was more than that in non-overweight children, and showed no statistical significance under both WHO and China criteria, as well as reached marginal significance under the IOTF criteria (P=0.042). Parental BMI in overweight and obese children were higher than that in non-overweight children, and reached statistical significance under three criteria (all P<0.05).
Full table
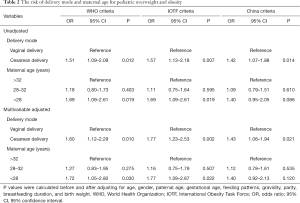
Risk factors for delivery mode and maternal age
The odds of delivery mode and maternal age, as risk factors for overweight and obesity in childhood, were shown in Table 2, and the risk trend of maternal age predicting pediatric overweight and obesity under three criteria (Figure 2). Before and after adjusting for age, gender, paternal age, gestational age, feeding patterns, gravidity, parity, breastfeeding duration and birth weight, cesarean delivery was significant associated with pediatric overweight and obesity under WHO (OR: 1.51 and 1.60, 95% CI: 1.09–2.09 and 1.12–2.29, P=0.012 and 0.010, respectively), IOTF (OR: 1.57 and 1.77, 95% CI: 1.13–2.18 and 1.23–2.53, P: 0.007 and 0.002, respectively), and China (OR: 1.42 and 1.43, 95% CI: 1.07–1.88 and 1.06–1.94, P=0.014 and 0.021, respectively) criteria. Maternal age <28 years showed no statistical difference in increasing the risk of pediatric overweight and obesity by China criteria (OR: 1.40, 95% CI: 0.95–2.05, P=0.086), and reached statistical significance by WHO and IOTF criteria (OR: 1.69, 95% CI: 1.09–2.61, P=0.019). Additionally, the restricted cubic spline regression model indicated that the predict risk for overweight and obesity in childhood was decreased with increase of maternal age, and the trend was moderate until maternal age with 32 years under WHO (Figure 2A), IOTF (Figure 2B), and China (Figure 2C) criteria.
Full table
Interaction between delivery mode and maternal age
The effect-size estimates of the interaction between delivery mode and maternal age using three criteria were presented in Table 3. According to categories of delivery mode and maternal age, we recombined six new variables and considered vaginal delivery and maternal age >32 years as a reference to explore their potential interaction. The OR of the single presence of either maternal age <28 years and 28-32 years or cesarean delivery had an increasing trend until the largest effect-size in cesarean delivery and maternal age <28 years by WHO (OR: 2.33, 95% CI: 1.19–4.58), IOTF (OR: 2.61, 95% CI: 1.34–5.08), China (OR: 2.35, 95% CI: 1.29–4.29) criteria. After multivariable adjustment, the preschool children with cesarean delivery and maternal age <28 years was 2.26, 2.92, and 2.36 times for the risk of being overweight and obese under WHO, IOTF, and China criteria, respectively. In view of a higher prevalence of overweight and obesity in boys aged over 5 years, we examined the interaction of delivery mode and maternal age in the risk of overweight and obesity for boys aged over 5 years, and found a rise in odds of overweight and obesity for boys aged over 5 years cesarean delivery with and maternal age <28 years before and after adjustment under WHO (OR: 3.86 and 3.5, 95% CI: 1.20–12.39 and 1.05–11.60, P: 0.023 and 0.041, respectively), IOTF (OR: 6.78 and 6.08, 95% CI: 1.73–26.59 and 1.49–24.90, P: 0.006 and 0.012, respectively), and China (OR: 3.86 and 3.43, 95% CI: 1.20–12.39 and 1.04–11.31, P: 0.023 and 0.043, respectively) criteria, respectively.
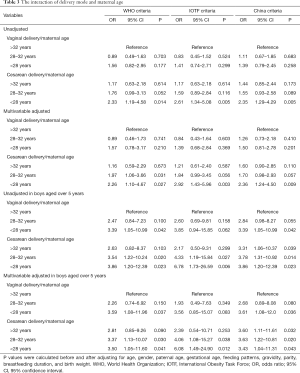
Full table
Three-dimension interactive surface
To affiliate clinical explanation, we created a three-dimension interactive surface between maternal age and birthweight in Figure 3, showing that the younger the mother is, the more weight the child is born with, and the greater the risk of being overweight or obese, and on the contrary the residual age of the mother and the small birthweight of the child were protective factors of overweight and obesity under WHO (Figure 3A) and IOTF criteria (Figure 3B). The association between maternal age and birthweight was more obvious in China criteria (Figure 3C) than the other two criteria.
Discussion
The study aimed to examine the individual and interactive association of delivery mode and maternal age with the risk of overweight and obesity in childhood. The results found that cesarean delivery and maternal age <28 years might be predictors for overweight and obesity, the interaction of which increased at least double risk of overweight and obesity compared with others, especially in boys aged over 5 years. As far as we know, this is the first report on the synergistic effect of delivery mode and maternal age in predicting preschool overweight and obesity. Its important clinical significance lies in the reduction of cesarean delivery rate and providing information of the benefits of age-appropriate birth to help prevent preschool children from being overweight and obesity.
In this study, the rate of cesarean delivery was nearly 58% in the overweight and obesity group, and higher than that in the non-overweight group. A number of studies have reported that birth by cesarean delivery was closely associated with pediatric overweight and obesity (25-27). The influence of cesarean delivery for offspring overweight and obesity was found in multiple stages of growth and development, such as infancy period, preschool stages, adolescence, and early adulthood (3,6,27,28). Compared to vaginal delivery, cesarean delivery influenced the newborn acquisition of maternal vaginal microbiota, result in the microbiota dysbiosis (29). An early study showed the primary gut microbiota in infants born by cesarean delivery might be disturbed for up to six months after the birth (30). There was a significant difference in the gut microbiota composition of important bacterial species between obese and lean children (31). Additionally, Gut microbiome transplantation was considered as a protective strategy against obesity and obesity-related diseases while the method was still experimental (32,33). It is possible that intestinal microbiota plays an essential role in the association between delivery mode and pediatric obesity. Besides, there were other underlying mechanisms independent of the intestinal microbiota in the pathophysiology of obesity, such as inflammation and immune factors.
In view of maternal age, we found the rate of overweight and obesity in preschool children decreased with advancing maternal age, which was consistent with a previous study (19). It was a possible mechanism that older mothers were known to give birth to smaller infants, which might be last in later in life. Higher maternal age (OR: 1.11, 95% CI: 1.01–1.22) was one of the strongest predictors of both onset and resolution of overweight/obesity between the primary school children and adolescents (34), which is consistent with our study results.
It is known that cesarean delivery increases the risk of overweight and obesity in childhood. Maternal age was affected by some other factors so that it had a small contribution to predict overweight and obesity later in life. We hypothesized that interaction of delivery mode and maternal age made a larger impact on predicting the risk for pediatric overweight and obesity. Our study results found that the interaction of cesarean delivery and maternal age <28 years increased 1.26–1.92 times in the risk of being overweight and obese under three criteria compared with vaginal delivery and maternal age >32 years, and the risk in boys over 5 years was higher to reach 3.43–6.08 times.
A strength of this study was its use of three different growth criteria estimating overweight and obesity. Our results were adjusted for several variables ignored by some previous studies, such as gestational age, feeding patterns, and breastfeeding duration. Similar to other cross-sectional studies, this study had following limitations. Firstly, there was recall bias for some variables in questionnaires, such as weight, height, and birth history, which would have impact on risk estimate. Secondly, our results were not adjusted for maternal pre-pregnancy BMI, maternal education, and antibiotics use during pregnancy due to limited data. Thirdly, cesarean delivery was not divided as planned and unplanned type, although cesarean type was a controversy for the risk of obesity in childhood. A prospective cohort study showed no difference between two types (35), while a study of 8,900 Chinese children found significant difference (3).
Conclusions
Taken together, our findings suggest that the interaction of cesarean delivery and maternal age <28 years, especially in boys over 5 years old, was closely associated with an increased risk of overweight and obesity in Chinese preschool children. We agree that further studies are helpful to call on government and parents to attach importance to control weight in boys over 5 years with maternal age <28 years and cesarean delivery.
Acknowledgments
We are grateful to all participating children and their guardians for their cooperation and willingness, as well as kindergarten teachers and health physicians for their great help.
Funding: This work was financially supported by the National Natural Science Foundation of China (Grant numbers: 41571376 and 81970042) and the Fundamental Research Funds for the Central Universities and Research projects on biomedical transformation of China-Japan Friendship Hospital (Grant numbers: PYBZ1812).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.128). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethical approval was procured from the ethics committee of China-Japan Friendship Hospital. All child guardians provided written informed consent for the use of data in questionnaires, as well as the subsequent analyses. The children, guardians, health physicians, and kindergarten teachers, received no financial compensation or gifts.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 2010;92:1257-64. [Crossref] [PubMed]
- Piernas C, Wang D, Du S, et al. The double burden of under- and overnutrition and nutrient adequacy among Chinese preschool and school-aged children in 2009-2011. Eur J Clin Nutr 2015;69:1323-9. [Crossref] [PubMed]
- Rutayisire E, Wu X, Huang K, et al. Cesarean section may increase the risk of both overweight and obesity in preschool children. BMC Pregnancy Childbirth 2016;16:338. [Crossref] [PubMed]
- Chu S, Zhang Y, Jiang Y, et al. Cesarean section and risks of overweight and obesity in school-aged children: a population-based study. QJM 2018;111:859-65. [Crossref] [PubMed]
- Blustein J, Attina T, Liu M, et al. Association of caesarean delivery with child adiposity from age 6 weeks to 15 years. Int J Obes (Lond) 2013;37:900-6. [Crossref] [PubMed]
- Mueller NT, Zhang M, Hoyo C, et al. Does cesarean delivery impact infant weight gain and adiposity over the first year of life? Int J Obes (Lond) 2019;43:1549-55. [Crossref] [PubMed]
- Pei Z, Heinrich J, Fuertes E, et al. Cesarean delivery and risk of childhood obesity. J Pediatr 2014;164:1068-73.e2. [Crossref] [PubMed]
- Wang L, Alamian A, Southerland J, et al. Cesarean section and the risk of overweight in grade 6 children. Eur J Pediatr 2013;172:1341-7. [Crossref] [PubMed]
- Mueller NT, Whyatt R, Hoepner L, et al. Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. Int J Obes (Lond) 2015;39:665-70. [Crossref] [PubMed]
- Li HT, Zhou YB, Liu JM. The impact of cesarean section on offspring overweight and obesity: a systematic review and meta-analysis. Int J Obes (Lond) 2013;37:893-9. [Crossref] [PubMed]
- Sutharsan R, Mannan M, Doi SA, et al. Caesarean delivery and the risk of offspring overweight and obesity over the life course: a systematic review and bias-adjusted meta-analysis. Clin Obes 2015;5:293-301. [Crossref] [PubMed]
- Kahveci B, Melekoglu R, Evruke IC, et al. The effect of advanced maternal age on perinatal outcomes in nulliparous singleton pregnancies. BMC Pregnancy Childbirth 2018;18:343. [Crossref] [PubMed]
- Rydahl E, Declercq E, Juhl M, et al. Cesarean section on a rise-Does advanced maternal age explain the increase? A population register-based study. PLoS One 2019;14:e0210655. [Crossref] [PubMed]
- Rossen J, Klungsoyr K, Albrechtsen S, et al. Can oxytocin augmentation modify the risk of epidural analgesia by maternal age in cesarean sections? Acta Obstet Gynecol Scand 2018;97:872-9. [Crossref] [PubMed]
- Robson SJ, de Costa CM. Thirty years of the World Health Organization's target caesarean section rate: time to move on. Med J Aust 2017;206:181-5. [Crossref] [PubMed]
- Triunfo S, Ferrazzani S, Draisci G, et al. Role of maternal characteristics and epidural analgesia on caesarean section rate in groups 1 and 3 according to Robson's classification: a cohort study in an Italian university hospital setting. BMJ Open 2018;8:e020011. [Crossref] [PubMed]
- Saunders T. Potential contributors to the canadian pediatric obesity epidemic. ISRN Pediatr 2011;2011:917684.
- Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. BMJ 2005;330:1357. [Crossref] [PubMed]
- Gebremedhin S. Prevalence and differentials of overweight and obesity in preschool children in Sub-Saharan Africa. BMJ Open 2015;5:e009005. [Crossref] [PubMed]
- Liu S, Zhang J, Ma J, et al. Synergistic interaction between bedtime and eating speed in predicting overweight and obesity in Chinese preschool-aged children. Aging (Albany NY) 2019;11:2127-37. [Crossref] [PubMed]
- The Coordinating Team in the Department of Nutrition for Health and Development of the World Health Organization. WHO child Growth Standards. World Health Organization (ISBN 92 4 154693 X). 2006:260-95.
- Obesity and overweight. Available online: (accessed on February 15, 2019).https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240-3. [Crossref] [PubMed]
- Li H, Ji CY, Zong XN, et al. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi 2009;47:493-8. [PubMed]
- Lavin T, Preen DB. Investigating Caesarean Section Birth as a Risk Factor for Childhood Overweight. Child Obes 2018;14:131-8. [Crossref] [PubMed]
- Chen G, Chiang WL, Shu BC, et al. Associations of caesarean delivery and the occurrence of neurodevelopmental disorders, asthma or obesity in childhood based on Taiwan birth cohort study. BMJ Open 2017;7:e017086. [Crossref] [PubMed]
- Yuan C, Gaskins AJ, Blaine AI, et al. Association Between Cesarean Birth and Risk of Obesity in Offspring in Childhood, Adolescence, and Early Adulthood. JAMA Pediatr 2016;170:e162385. [Crossref] [PubMed]
- Kuhle S, Woolcott CG. Caesarean section is associated with offspring obesity in childhood and young adulthood. Evid Based Med 2017;22:111. [Crossref] [PubMed]
- Penders J, Thijs C, Vink C, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 2006;118:511-21. [Crossref] [PubMed]
- Grönlund MM, Lehtonen OP, Eerola E, et al. Fecal microflora in healthy infants born by different methods of delivery: permanent changes in intestinal flora after cesarean delivery. J Pediatr Gastroenterol Nutr 1999;28:19-25. [Crossref] [PubMed]
- Bervoets L, Van Hoorenbeeck K, Kortleven I, et al. Differences in gut microbiota composition between obese and lean children: a cross-sectional study. Gut Pathog 2013;5:10. [Crossref] [PubMed]
- Jayasinghe TN, Chiavaroli V, Holland DJ, et al. The New Era of Treatment for Obesity and Metabolic Disorders: Evidence and Expectations for Gut Microbiome Transplantation. Front Cell Infect Microbiol 2016;6:15. [Crossref] [PubMed]
- Porras D, Nistal E, Martinez-Florez S, et al. Functional Interactions between Gut Microbiota Transplantation, Quercetin, and High-Fat Diet Determine Non-Alcoholic Fatty Liver Disease Development in Germ-Free Mice. Mol Nutr Food Res 2019;63:e1800930. [Crossref] [PubMed]
- Kerr JA, Long C, Clifford SA, et al. Early-life exposures predicting onset and resolution of childhood overweight or obesity. Arch Dis Child 2017;102:915-22. [Crossref] [PubMed]
- Huh SY, Rifas-Shiman SL, Zera CA, et al. Delivery by caesarean section and risk of obesity in preschool age children: a prospective cohort study. Arch Dis Child 2012;97:610-6. [Crossref] [PubMed]


