
The effect of blood lactate and NT-proBNP predict the survival in patients with invasive mechanical ventilation
Introduction
Respiratory failure is one of the most common critical diseases. There may be respiratory failure due to craniocerebral damage, postoperative resuscitation injury, or other serious conditions. It has already been reported that noninvasive mechanical ventilation and invasive mechanical ventilation (IMV) are used to treated respiratory failure. Furthermore, IMV helps stabilize patients with hypoxemic and hypercapnic respiratory failure, decreases inspiratory work of breathing, redistributes blood flow from exercising respiratory muscles to other tissues in patients with shock, and allows for the implementation of lung-protective (low tidal volume) ventilation in patients with acute respiratory distress syndrome (ARDS) (1-3).
Clinical studies have confirmed that ventilation mode ventilation time ventilator-associated pneumonia, gastrointestinal bleeding and other factors that affect patients with significant risk factors in their prognosis. Therefore, some studies aimed to find effective clinical indicators to predict the prognosis of patients in the early stage are conducive to comprehensively reflect the state of the body, the severity of the disease and the treatment effect (1-3). The earlier study showed blood NT- proBNP had a potential role in assessing disease severity, treatment efficacy and prognosis in chronic hypercapnic respiratory failure (4). Then another study showed that APACHE II score applied in combination with arterial blood lactate clearance rate is of clinical significance in assessing the prognosis of ARDS patients (5). One new research showed blood lactate levels might be predictive of the outcome of patients with ARDS (6). However, we do not know whether blood NT- proBNP, lactate, or other parameters can predict the prognosis of patients undergoing IMV.
Therefore, we looked to investigate the value of blood CRP, PCT, NT-proBNP, and lactate in predicting the prognosis of patients undergoing IMV.
Methods
Study sample
From May 2016 to December 2019, 353 incident patients more than 18 years old with coma admitted to the Intensive Care Unit of Shanghai Sixth People’s Hospital East Affiliated to Shanghai University of Medicine & Health Sciences were recruited as the study objects, including 147 men, with an average age of (59.6±17.1) years. All the subjects in this study were assessed by the Glasgow Coma Scale (7,8) about the diagnosis standard of patients with severe coma. All the patients underwent IMV, including 225 cases of postoperative recovery, 76 cases of brain injury, 51 cases of disease aggravation, and 1 case of a traffic accident. In this study, patients with severe hepatic and renal insufficiency, patients with coexisting basic diseases (such as hematological diseases and advanced malignant tumors), patients who have used drugs that affect lactate metabolism (such as metformin, sodium nitroprusside, etc.), Patients with IMV contraindications or who declined to use IMV for treatment were also removed; patients with incomplete clinical data or noncooperation in treatment were also excluded to minimize the interference factors that affect the determination of blood lactate level.
This study was approved by the academic ethics committee of our college and obtained the informed consent of all the subjects.
Clinical assessment
The demographic information, body mass index (BMI), CRP, PCT, NT-proBNP, lactate, during hospitalization, the number of WBCs and neutrophils was calculated at baseline. Lactate in 12 h and lactate in 24 h were determined. Each patient underwent resting measurements of GCS score, duration in ventilation, duration in operation, hemorrhage, crystal, colloid and suspended red liquid input. The primary outcome was death. Survival was estimated from the date of confirmation until their leave from the hospital.
IMV
IMV was performed in all patients (9). IMV includes an endotracheal tube and a mechanical ventilator. IMV helps stabilize patients with hypoxemic and hypercapnic respiratory failure, decreases inspiratory work of breathing, redistributes blood flow from exercising respiratory muscles to other tissues in patients with shock, and allows for the implementation of lung-protective (low tidal volume) ventilation in patients with ARDS. Our patients were received volume-controlled (VC) ventilation and used one common strategy of synchronized intermittent mandatory ventilation (SIMV).
Glasgow Coma Scale (GCS) scoring method
GCs evaluated the severity of severe brain injury. Scoring range: 0–15 points. The GCS score of the patients was positively correlated with the severity of the disease. The critical value of judging the patients as low group and the high group was 9 points.
Statistical analysis
Continuous variables were presented by mean or median, and categorical variables were presented by absolute number and percentage. Comparisons were performed using t-tests or Mann-Whitney U-test for continuous variables and chi-square or Fisher’s exact tests for categorical variables. The impact of parameters on prognosis was evaluated using univariate and multivariable cox proportional hazards analyses. Age, BMI, and sex were forced in models to adjust the multivariate analysis. Receiver operating characteristic (ROC) curves for independent parameters were drawn, and the areas under the curves were calculated. For a specific parameter, the cut-off level that resulted in the highest product of sensitivity and specificity was an optimal cutoff value for prognostication. Kaplan-Meier methods were used to estimate the outcome of time to survival, and disparities between the sexes were assessed with the long-rank test. Statistical significance was defined as the two-tailed P value of <0.05 for all analyses. Statistical analysis was performed using SPSS (Statistic Package for Social Science, Chicago, IL, USA) version 25.0 and GraphPad Prism (San Diego, CA, USA) version 8.0.
Results
Characteristics of the studies
A total of 353 patients with IMV matched inclusion criteria, 147 (41.6%) were men. The mean duration of hospitalization was 25.5±20.6 days. Twenty-four men and 41 women died. Demographic and hemodynamic data are presented in Table 1. The mean age was 64.7±16.7 years for non-survivor, 58.5±17.0 years for the survivor. There were significant differences in the types of diagnosis between the two groups. Nonsurvivor had similar percentages of non-craniocerebral trauma, craniocerebral, and another disease, but survivor had many patients with non- craniocerebral trauma and few patients with others disease. There were no differences in sex, duration in operation, hemorrhage, crystal, colloid and blood transfusions input between non-survivor and survivor patients. Nonsurvivor had a longer duration of ventilation compared with a survivor. The median survival time for nonsurvivors was six days, but the median survival time for survivors was 22 days, so there was a significant statistical difference between the two groups.
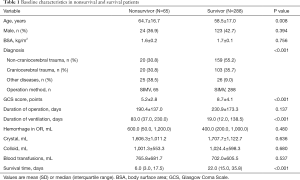
Full table
Expressions of several plasma protein markers in patients
There were no significant differences in expressions of CRP between the nonsurvivors group and the survivor group (Figure 1A). Survival patients had significant lower PCT, NT-proBNP, lactate in baseline (2.8±2.0 vs. 4.5±3.5 mmol/L), lactate in 12 h (2.5±1.5 vs. 3.5±3.1 mmol/L) and lactate in 24 h (1.8±1.2 vs. 2.6±1.5 mmol/L) compared with nonsurgical patients respectively (Figure 1B,C,D,E,F). Although there were no significant differences in 12 h lactate clearance and 24 h lactate clearance between nonsurvivor group and survivor group, nonsurvivors had the lower 12 h lactate clearance and 24 h lactate clearance (Figure 1G,H).

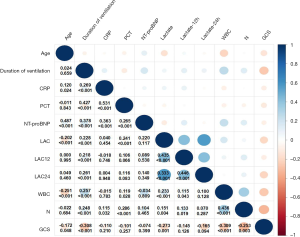
Relationship between duration in ventilation and several clinical parameters in patients
There were various correlations duration in ventilation and several clinical parameters in patients. The major significant positive correlations were demonstrated between duration in ventilation and CRP, PCT, NT-proBNP, lactate, number of WBC, neutrophils and GCS score (Figure 2). In all patients, age correlated to NT-proBNP, lactate and number of WBC. CRP correlated to PCT, NT-proBNP and number of neutrophils. PCT correlated to NT-proBNP, lactate, and number of WBC and neutrophils. Besides, lactate in baseline and lactate in 12 h had positive correlations to several WBC and neutrophils in patients. However, NT-proBNP had no correlations to lactate and the number of WBC and neutrophils in patients.
Factors influencing survival
On univariate Cox proportional hazards analysis, age, NT-proBNP, CRP, lactate in the baseline, lactate in 12 h and lactate in 24 h were related to survival in all patients. On multivariate forward stepwise Cox proportional hazards analysis, the model adjusted by age, gender and BMI associated the above parameters, age, NT-proBNP, and lactate was the independent predictor of survival in patients (Figure 3A,B). However, blood lactate clearance is not the predictor of survival rate in these patients (Figure 3A).

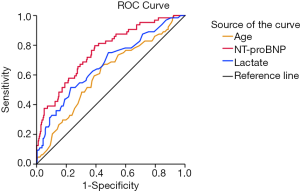
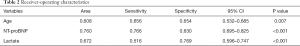
Receiver-operating characteristic
ROC curves were plotted for age, NT-proBNP, and lactate in all patients (Figure 4 and Table 2). Age <61.5 years had a sensitivity of 65.6% and specificity of 65.4% in predicting the survival in all patients. NT-proBNP <230.5 pg/mL had a high sensitivity of 76.6% and specificity of 63.0% in patients. Lactate <3.7 mmol/L in patients had a sensitivity of 51.6% and specificity of 76.9% to predict survival.
Full table
Kaplan-meier event-free survival analysis
Kaplan-Meier event-free survival curves according to the cutoff values of age, NT-proBNP and lactate by ROC analysis. In analysis of all patients, patients with an age ≥61.5 years had a significantly poorer prognosis than those with an age <61.5 years (1-month survival, 87.7% vs. 89.9%; 2-month survival, 84.0% vs. 88.4%, 3-month survival, 79.7% vs. 87.9%, respectively; P=0.001; Figure 5A). Patients with NT-proBNP <230.5 pg/mL had a significantly better survival rate than male patients with a NT-proBNP ≥230.5 pg/mL (1-month survival, 86.7% vs. 95.1%; 2-month survival, 82.0% vs. 94.1%, 3-month survival, 77.3% vs. 93.6%, respectively; P<0.001; Figure 5B). Patients with lactate ≥3.7 mmol/L had significantly worse survival (1-month survival, 72.2% vs. 94.5%; 2-month survival, 67.0% vs. 94.1%, 3-month survival, 65.9% vs. 92.9%,respectively; P<0.001; Figure 5C).

Then we used two or three of the three parameters to the group and analyzed the survival rate in patients. Patients with age <61.5 years and NT-proBNP <230.5 pg/mL and lactate <3.7 mmol/L had the best survival rate, and the 1- and 2-year survival rates were 98.8% and 97.6%, respectively (Figure 5D,E,F,G). Patients with NT-proBNP ≥230.5 pg/mL and lactate ≥3.7 mmol/L had the worst survival rate whose the 1- and 2-year survival rates were 46.5% and 44.2%, respectively (Figure 5D,E,F,G).
Discussion
This study suggests that age, blood NT-proBNP and lactate are the independent predictors of survival in patients undergoing IMV. And the blood NT-proBNP may be the best independent predictors of survival in these patients. Blood lactate clearance rate, however, is not the predictors of survival rate in these patients. So, blood NT-proBNP and lactate may be used as biomarkers to predict the prognosis of patients undergoing IMV.
In the present study, we include the patients with craniocerebral, non- craniocerebral and other diseases such as liver cancer, gastric carcinoma, and glioma and so on. These findings are inconsistent with earlier studies. The earlier studies only focused on one kind of disease, but in our study, we include patients with respiratory failure caused by all different aspects. If the patient needs IMV in our department, the patient was included in the present study. So, the data are representative.
The increase of plasma NT-proBNP is positively related to the severity of heart failure and can evaluate the cardiovascular function. When patients suffer from cardiac insufficiency, due to the increase of cardiac volume load or pressure load, the myocardium is more stretched or the ventricular wall pressure will increase, which will increase the plasma NT-proBNP concentration. Our data is consistent with earlier studies (4). And the plasma NT-proBNP levels can also reflect the amount of liquid input. So, the nonsurvivors had higher plasma NT-proBNP levels, and the plasma NT-proBNP levels can predict the prognosis of the patient undergoing IMV.
It is not difficult to understand why older people are more likely to die in our data. The data is consistent with the latest research study (10,11). They reported the elderly patients with acute respiratory failure had higher mortality. In the present study, nonsurvivor was the older people and had a worse pulmonary function and poorer recovery ability so as they are more prone to respiratory failure and need IMV, then they need a longer duration of ventilation and have shorter survival time.
Nonsurvivors had higher blood lactate levels. And lactate is the independent predictor of survival in these patients undergoing IMV. Lactate is directly produced by anaerobic glucose metabolism. It is a product converted from pyruvic acid by the glycolytic pathway. Therefore, it is considered to be a sensitive biomarker that can reflect intracellular oxygen supply and peripheral tissue perfusion at an early stage and can be used for evaluating disease severity and prognosis, and it is closely related to the hospitalization time and mortality of patients (12). The normal value of blood lactate level is 0.5–1.5 mmol/L. The lactate levels of patients may be more than 5 mmol/L due to tissue hypoxia and hypoperfusion, stress-induced hypercatecholaminemia, organ dysfunction, and other reasons. Our data showed the patients. Under physiological conditions, lungs hardly affect the metabolism of systemic lactate. However, most patients with severe respiratory failure already have tissue hypoperfusion and oxygenation disorders to varying degrees, and then glucose anaerobic metabolism increases, leading to poor injection and oxygenation disorders, and then glucose anaerobic metabolism increases, leading to increased lactate production. At the same time, the infection itself can lead to the reduction of pyruvate dehydrogenase activity, which increases the release of lactate from lung parenchyma (13,14), and lactate release is linked strongly to the degree of lung injury (13-16), which can lead to hyperlactatemia. Therefore, it is speculated that blood lactate concentration can be used as one of the markers to predict the severity and prognosis of patients with severe respiratory failure. In our study, the data show that blood lactate is a better predictor of survival in patients undergoing IMV.
However, some people think that it is not sufficient to detect the blood lactate level at a single moment as a timely and accurate reflection of the patient’s basic condition, the severity of illness and therapeutic reactivity (17-19). And they think if the blood lactate level can return to normal in a short period, it is better after pre-treatment, which indicates that the blood lactate clearance is more accurate and credible as a key indicator for prognosis evaluation. At present, it has been confirmed that the early lactate clearance can directly reflect the prognosis of patients and is closely related to the severity of infection and responsiveness to treatment (20-23). This study shows that the nonsurvivors had lower lactate clearance, so the more serious respiratory failure, the lower lactate clearance, which can partly reflect the degree of lung injury in the body and further indicate the severity of patient’s respiratory failure. At the same time, this study showed that the blood lactate level of patients in the survival group was significantly lower than that of patients in the nonsurvival groups of patients. In the present study, one of the reasons why 12 or 24 h lactate clearance is not the independent predictors of survival is the small sample size, so we need a larger, multicenter study to confirm the data.
There are limitations to the present study. The patients with no serious diseases were not enough included in this study. We feel it is important to evaluate the data on those patients. Furthermore, we do not have long-term follow up data, so we could not analyze the long-term survival rate and only use hospitalized survival to reflect the prognosis. Also, the focus of this analysis was patients with respiratory failure being managed at a single center; therefore, we need a larger sample, multicenter, long-term follow up along with a full cohort of patients with respiratory failure to explore the mechanism and role of these parameters.
Concluding, although the number of patients in this study was limited, the data suggest that blood NT-proBNP and lactate may be used as biomarkers to predict the prognosis of patients undergoing IMV. And age is also a better predictor of survival rate in these patients. Compared with age and blood lactate, blood NT-proBNP may be the best independent predictors of survival in these patients undergoing IMV. The elderly patients and patients with higher blood NT-proBNP and/or lactate had a worse survival rate. These results suggest that patients undergoing IMV may have worse pulmonary ventilatory, gas exchange abnormality, and cardiovascular dysfunction, which need further pay attention to measure the blood NT-proBNP and lactate levels in the baseline.
Acknowledgments
We thank the study investigations, fellows, nurses, and research coordinators who took part in the present study.
Funding: This work was supported by the Program of Shanghai Sixth People’s Hospital East Affiliated to Shanghai University of Medicine & Health Sciences Institute level scientific research fund (Grant No. DY201903).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.140). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the academic ethics committee of our college (No. 2017-001) and obtained the informed consent of all the subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. [Crossref] [PubMed]
- Tan J, Song Z, Bian Q, et al. Effects of volume-controlled ventilation vs. pressure-controlled ventilation on respiratory function and inflammatory factors in patients undergoing video-assisted thoracoscopic radical resection of pulmonary carcinoma. J Thorac Dis 2018;10:1483-9. [Crossref] [PubMed]
- Kapitan KS. Ventilatory failure. Can you sustain what you need? Ann Am Thorac Soc 2013;10:396-9. [Crossref] [PubMed]
- Budweiser S, Luchner A, Jorres RA, et al. NT-proBNP in chronic hypercapnic respiratory failure: a marker of disease severity, treatment effect and prognosis. Respir Med 2007;101:2003-10. [Crossref] [PubMed]
- Wu WH, Niu YY, Zhang CR, et al. Combined APACH II score and arterial blood lactate clearance rate to predict the prognosis of ARDS patients. Asian Pac J Trop Med 2012;5:656-60. [Crossref] [PubMed]
- Kamo T, Tasaka S, Suzuki T, et al. Prognostic values of the Berlin definition criteria, blood lactate level, and fibroproliferative changes on high-resolution computed tomography in ARDS patients. BMC Pulm Med 2019;19:37. [Crossref] [PubMed]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974;2:81-4. [Crossref] [PubMed]
- Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery 2017;80:6-15.
- Walter JM, Corbridge TC, Singer BD. Invasive Mechanical Ventilation. South Med J 2018;111:746-53. [Crossref] [PubMed]
- Baek MS, Chung CR, Kim HJ, et al. Age is major factor for predicting survival in patients with acute respiratory failure on extracorporeal membrane oxygenation: a Korean multicenter study. J Thorac Dis 2018;10:1406-17. [Crossref] [PubMed]
- Eachempati SR, Hydo LJ, Shou J, et al. Outcomes of acute respiratory distress syndrome (ARDS) in elderly patients. J Trauma 2007;63:344-50. [Crossref] [PubMed]
- Krishna U, Joshi SP, Modh M. An evaluation of serial blood lactate measurement as an early predictor of shock and its outcome in patients of trauma or sepsis. Indian J Crit Care Med 2009;13:66-73. [Crossref] [PubMed]
- Jackson TC, Zhang YV, Sime PJ, et al. Development of an accurate and sensitive method for lactate analysis in exhaled breath condensate by LC MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci 2017;1061-1062:468-73. [Crossref] [PubMed]
- Bakker J.. Lactate levels and hemodynamic coherence in acute circulatory failure. 1. Best Pract Res Clin Anaesthesiol 2016;30:523-30. [Crossref] [PubMed]
- Umbrello M, Chiumello D. Interpretation of the transpulmonary pressure in the critically ill patient. Ann Transl Med 2018;6:383. [Crossref] [PubMed]
- Routsi C, Bardouniotou H, Delivoria-Ioannidou V, et al. Pulmonary lactate release in patients with acute lung injury is not attributable to lung tissue hypoxia. Crit Care Med 1999;27:2469-73. [Crossref] [PubMed]
- Haas SA, Lange T, Saugel B, et al. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med 2016;42:202-10. [Crossref] [PubMed]
- Düring J, Dankiewicz J, Cronberg T, et al. Lactate, lactate clearance and outcome after cardiac arrest: A post-hoc analysis of the TTM-Trial. Acta Anaesthesiol Scand 2018;62:1436-42. [Crossref] [PubMed]
- Ryoo SM, Lee J, Lee YS, et al. Lactate Level Versus Lactate Clearance for Predicting Mortality in Patients With Septic Shock Defined by Sepsis-3. Crit Care Med 2018;46:e489-95. [Crossref] [PubMed]
- Shang XL, Liu DW, Wang XT, et al. The relationship between arterial blood lactate clearance, prognosis and myocardial damage in patients with septic shock after early goal-directed therapy. Zhonghua Nei Ke Za Zhi 2018;57:345-50. [PubMed]
- Ryoo SM, Lee J, Lee YS, et al. Lactate Level Versus Lactate Clearance for Predicting Mortality in Patients With Septic Shock Defined by Sepsis-3. Crit Care Med 2018;46:e489-95. [Crossref] [PubMed]
- Choudhary R, Sitaraman S, Choudhary A. Lactate clearance as the predictor of outcome in pediatric septic shock. J Emerg Trauma Shock 2017;10:55-9. [Crossref] [PubMed]
- Passos RD, Ramos JG, Gobatto A, et al. Lactate clearance is associated with mortality in septic patients with acute kidney injury requiring continuous renal replacement therapy: A cohort study. Medicine (Baltimore) 2016;95:e5112. [Crossref] [PubMed]


