
Relevance of arm somatic copy number alterations for oncologic outcomes and tumor immune microenvironment in clear cell renal cell carcinoma
Introduction
Renal cell carcinoma (RCC) represents 2–3% adult malignancies and inflicts about 271,000 new patients worldwide every year (1,2). Clear cell renal cell carcinoma (ccRCC) is the most common histological subtype, accounting for around 70–80% of all RCC (3). Within this seemingly homogeneous category, tumors exhibited varying survival prospects. Over 50% of the patients are diagnosed with metastatic disease or develop metastasis after curative surgeries (4). Currently there are clear clinical needs at the two extremes of ccRCC risk: those with early stage disease choosing management strategies and those with localized late stage ccRCC who might benefit from adjuvant tyrosine kinase inhibitor (TKI) therapies after curative nephrectomy (5).
It is well established that genetic alterations and a net accumulation are responsible for cancer development and progression (6). Some genetic alterations are significantly associated with stage, grade and prognosis (7). For example, in ccRCC loss of chromosome arms 8p, 9p and 14q is associated with higher stage and grade; deletions of 9p correlates with early recurrence (8). However, the prognostic value of each arm SCNA in ccRCC has not been systematically evaluated in a large cohort. Besides, it is increasingly recognized that tumor microenvironment plays a fundamental role in tumor progression (9). Previous researches suggested tumor aneuploidy correlated with markers of immune evasion in some malignancies (10). Relations between histologic features, clinical outcomes and cytogenetic aberrations have been studied (11), but further crosstalk between arm SCNA and tumor immune microenvironment in ccRCC remained unknown. Comprehensive genetic profiling and its associations with tumor microenvironment may not only provide insights into the mechanisms of tumor progression, but also provide potential prognostic biomarkers (12).
In this study, we retrospectively correlated arm somatic copy number alterations with clinicopathological information and oncologic outcomes in a cohort of 524 ccRCC patients, demonstrating the prognostic landscape of arm SCNAs. We further analyzed how arm SCNA burden impact patient survival and tumor microenvironment in ccRCC.
Methods
Patients and data collection
We retrospectively analyzed the copy number alterations, gene expression profiles and clinical information of 524 ccRCC patients who had undergone nephrectomy in The Cancer Genome Atlas (TCGA) Kidney Clear Cell Renal Cell Carcinoma (KIRC) cohort. Copy number alterations of each sample were downloaded and processed from cBioPortal (http://www.cbioportal.org/). Clinical information of the TCGA KIRC cohort was obtained from the TCGA Pan-cancer Clinical Data Resource, which provides high-quality clinical data (13). We used the UCSC Xena (https://xenabrowser.net/heatmap/) to download RNA-seq data. The mRNA levels were evaluated with bulk tumor samples. Patients with incomplete genetic or clinical information were excluded. Patients who received neoadjuvant therapy were not included neither. The study was approved by the Clinical Research Ethics Committee of Zhongshan Hospital, Fudan University with the approval number B2015-030.
Estimated immune cell type infiltrations
CIBERSOTR is a computational method for inferring leukocyte representation in bulk tumor transcriptomes and has been proved to have strong agreement with ground truth assessments in bulk tumors (14,15). We used CIBERSORT to calculate the absolute normalized cell count and relative cell fraction of major immune cell types with LM22 gene signature. To support results obtained with CIBERSORT, we also compared the metagene value for Treg cells, macrophages and NK cells with three well-established immune signatures (16). The metagene values were computed to summarize an immune gene signature as the mean value of each gene in the category. Comparison of gene expression profiles of arm SCNAhigh versus SCNAlow tumors was carried out with Gene Set Enrichment Analysis (GSEA) to gain more biological understanding of arm SCNAs in ccRCC (17).
Statistical analysis
Kaplan-Meier analysis with log-rank test demonstrated the survival curves and survival differences between arm SCNAhigh and arm SCNAlow tumors. OS was defined as the time of curative surgery to the time of death or last follow up time, while recurrence free survival (RFS) was calculated as the time from surgery to the time of recurrence or metastasis. Patients with metastatic renal cell carcinoma were excluded from RFS analyses. The prognostic value of arm SCNAs was evaluated by univariate and multivariate analyses. Comparisons of clinicopathological parameters between two groups were carried out by Student t test or Mann-Whitney U test depending on normality of the data distribution, Pearson’ s chi-square test and Cochran-Mantel-Haenszel χ2 test. All statistical analyses were two-sided and P<0.05 was considered statistically significant.
Results
Bubble heatmaps demonstrate the prevalence and prognostic landscape of arm somatic copy number alterations in ccRCC
Figure 1 shows the percentage of arm SCNAs and their prognostic value with univariate as well as multivariate analysis respectively. Arm SCNAs present in less than 1% ccRCC samples were not displayed. Amplification of 5q (39.7%), 5p (36.1%), 7p (32.6%), 7q (32.6%), 12q (23.1%), 12p (23.1%), 20q (21.9%) and 20p (21.4%) occurred in over 20% of ccRCC (Figure 1A). In the bubble heatmaps, a dark purple bubble indicated a significant association with worse OS or RFS while the size of the bubble indicated the hazard ratio (HR). In univariate analysis of copy number amplification for OS, 1p (P=0.002, HR =2.497), 3p (P=0.041, HR =1.947), 12p (P=0.009, HR =1.555) and 12q (P=0.013, HR =1.520) were associated with shorter OS. For RFS, 1p (P=0.011, HR =2.538), 1q (P=0.002, HR =2.163), 3q (P=0.002, HR =2.042), 6q (P=0.030, HR =2.696), 8q (P=0.036, HR =1.69), 19p (P=0.010, HR =1.859), 19q (P=0.003, HR =1.985) and 20q (P=0.028, HR =1.584) were adverse risk factors. The prognostic value of arm SCNA was further assessed by multivariable cox regression analyses each, with stage and grade as covariates. Amplification of 1p (P=0.012, HR =2.11), 3p (P=0.034, HR =2.01) and 1q (P=0.022, HR =1834) were independent adverse risk factor for OS or RFS in multivariate analysis (Figure 1A).

The most frequent arm somatic copy number loss is 3p (71.9%), followed by 14q (40.4%), 9q (28.6%), 9p (28.1%), 8p (26.0%) and 6q (24.0%) (Figure 1B). We found that loss of 4p (OS: P<0.001, HR =2.024; RFS: P<0.001, HR =2.57), 4q (OS: P<0.001, HR =2.294; RFS: P<0.001, HR =3.13), 9p (OS: P<0.001, HR =1.898; RFS: P<0.001, HR =1.745), 9q (OS: P<0.001, HR =1.745; RFS: P<0.001, HR =2.624), 13q (OS: P=0.001, HR =1.895; RFS: P=0.018, HR =1.731), 14q (OS: P=0.002, HR =1.623; RFS: P=0.004, HR =1.681), 15q (OS: P=0.002, HR =2.158; RFS: P<0.001, HR =2.695), 18p(OS:P=0.002, HR =1.766; RFS: P=0.049, HR =1.548) and 22q (OS: P=0.008, HR =1.851; RFS: P=0.003, HR =2.240) associated with worse OS and RFS in univariate analyses. After adjustment for stage and grade, deletion of 4p (P=0.018, HR =1.558), 4q (P=0.012, HR =1.614) and 13q (P=0.021, HR =1.588) remained their statistical significance for OS while 4p (P=0.005, HR =1.858), 4q (P=0.001, HR =2.005), 9p (P=0.013, HR =1.629) and 9q (P=0.020, HR =1.583) remained significant as an independent adverse risk factor for RFS (Figure 1B).
Loss of 4q contributes to CD8+ T cell exclusion and identifies a subset of early stage patients with high risk of death and recurrence
The findings suggested that deletion of 4q and 4p are the only independent adverse risk factors for both OS and RFS. Genes encoding chemoattractant for major cytotoxic CD8+T cells and NK cells, CXCL9, CXCL10 and CXCL11 all located on 4q.21. We found that CXCL9 (P=0.029), CXCL10 (P=0.059) and CXCL11 (P=0.017) mRNA expression were all significantly downregulated in ccRCC tumors with 4q deletion (Figure 2A,B,C). CIBERSORT analysis revealed that CD8+ T cell infiltration (P=0.002) and NK cell infiltration (P=0.051) decreased in ccRCC tumors with loss of 4q (Figure 2D,E). These findings suggested that 4q deletion led to immune exclusion via downregulation of CXCL9, CXCL10 and CXCL11.
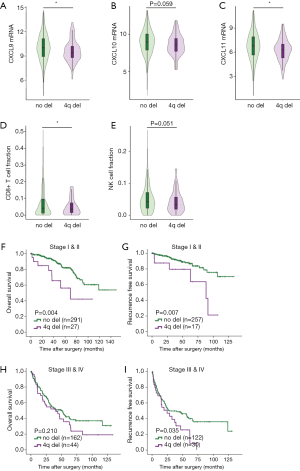
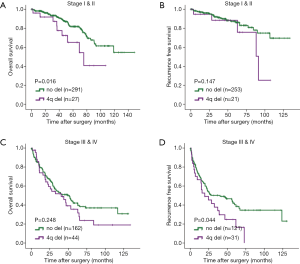
There are clear clinical needs for identifying early stage patients with high risk of metastasis and late stage patients who might benefit from adjuvant TKI treatment, so we further explored the prognostic value of 4q and 4p in different stages of ccRCC patients. Analysis of Kaplan-Meier log-rank test revealed that deletion of 4q associated with both worse OS (P=0.004) and RFS (P=0.007) in early stage (I & II) ccRCC patients (Figure 2F,G). Among early stage ccRCC patients, multivariate analyses showed that 4q deletion remained an independent risk factor for OS (P=0.018, HR =2.572, 95% CI: 1.173–5.639) and RFS (P=0.043, HR =2.634, 95% CI: 1.033–6.721) when factoring in tumor grade and stage. Thus, loss of 4q was a promising biomarker that could identify a subset of early stage ccRCC patients with a high risk of death and recurrence. Besides, in stage III & IV patients, 4q loss indicated a shorter RFS (Figure 2H,I). Stage I & II patients with 4p deletion had shorter OS (Figure S1A,B) while stage III & IV with 4p deletion had worse RFS (Figure S1C,D).
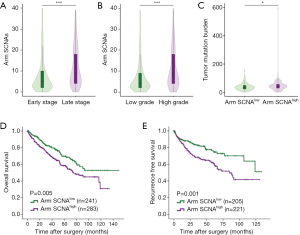
High level of arm copy number alterations associates with worse survival and higher tumor mutation burden
Number of arm SCNAs was split at median. Tumor with six or more arm SCNAs was considered arm SCNAhigh while tumors with less than six arm SCNAs was considered arm SCNAlow. We analyzed the correlations between clinicopathological characteristics and arm SCNA level. Tumors of people over 65 years old (P=0.028) and males (P=0.036) tended to harbor high arm SCNA level. High arm SCNA level also associated with higher tumor stage (P<0.001) and grade (P<0.001) (Table S1). Late stage and high grade ccRCC had more copy number alterations compared with early stage (P<0.001) and low grade (P<0.001) tumors, respectively (Figure 3A,B). In ccRCC, tumor mutation burdens are more abundant in arm SCNAhigh tumors (P=0.028), in contrast to a previous study showing that there are more SCNAs in tumors with low mutation burden (18) (Figure 3C). Kaplan-Meier analysis showed that arm SCNAlow patients had significantly prolonged OS (P=0.005) and RFS (P=0.001) compared with arm SCNAhigh patients (Figure 3D,E).

Full table
Immunosuppressive immune cells and T cell exhaustion markers enriched in high arm copy number alteration patients
ccRCCs are highly immunogenic tumors. We wondered whether arm SCNA could imparted different features on the tumor microenvironment. CIBERSORT analysis was performed to unveil the immune cell composition in arm SCNAhigh and arm SCNAlow tumors. Treg cells, macrophages and TFH cells significantly enriched in arm SCNAhigh tumors in terms of both absolute cell count and relative cell fraction. On the other hand, NK cells and mast cells were reduced in arm SCNAlow tumors (Figure 4A). To confirm our findings, we evaluated the established metagene value for Treg cells, macrophages and NK cells, which had been well recognized for their pro- or anti-tumor abilities. In accordance with CIBERSORT analysis, gene signature of Treg cells and macrophages were significantly elevated in arm SCNAhigh tumors (Figure 4B,C). NK cells metagene values were down-regulated in arm SCNAhigh tumors (Figure 4D).
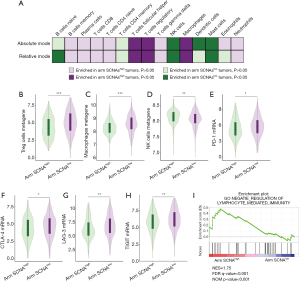
In most malignancies, higher CD8+ T cell infiltration associated with prolonged survival. However, in ccRCC, higher CD8+ T cell infiltration was an adverse risk factor for patient survival (19). We did not observe any changes in CD8+ T cell infiltration. Instead, markers of T cell exhaustion including PD-1, CTLA-4, LAG-3 and TIGIT significantly elevated in arm SCNAhigh tumors (Figure 4E,F,G,H), which indicated that the anti-tumor immunity of CD8+ T cells in arm SCNAhigh tumors were largely offset by immunosuppressive elements in tumor microenvironment. GSEA analyses revealed that lymphocyte mediated immunity was down-regulated in arm SCNAhigh tumors (Figure 4I). Our findings suggested that arm SCNAs were closely associated with immune suppression in ccRCC.
Discussion
To our knowledge, this is the first study to systematically evaluate the prognostic landscape of arm SCNAs and the associations with tumor microenvironment in a large cohort of over 500 ccRCC patients. The most frequent alterations included deletions of 3p, 14q and gain of 5q, in complete accordance with previous studies (20). The von Hippel Lindau (VHL) gene is one of the most important tumor suppressor gene located at 3p25.3 region in ccRCC. There is also a high concordance of other chromosome aberrations such as loss of 6q, 8p, 9q and amplification of 7p, 7q, 12q. In ccRCC, some arm SCNAs were associated with clinicopathological features. Significant associations with late tumor stage or grade were observed for loss of 9p, 9q, 14q, 18p, 21q (12). There was a high rate of chromosomal imbalances with loss of 9q, 15q, 18p, 18q, 22q and gains of 1q, 8q in RCC with sarcomatoid differentiations (21). In this study, we found almost all of these arm SCNAs correlated with worse OS or RFS in univariate analyses except loss of 21q.
According to previous studies that included survival as an end point, deletions of 4p, 8p, 9p, 14q and gain of 8q have been suggested to correlate with poorer survival (11,22-24). Loss of 4p, 9p maintained as independent adverse risk factors when factoring stage and grade with multivariate analyses in our study. Furthermore, we identified that 4q as an independent adverse risk factor for both OS and RFS in ccRCC. It could also stratify a subset of early stage ccRCC patients with a higher risk of death and recurrence. The prognostic value of 4q deletion has not been discovered before, partly because of the limited sample size and inappropriate statistical power in previous studies. Chemokines responsible for CD8+ T cell recruitment including CXCL9, CXCL10 and CXCL11 located on chromosome 4q. Expression analysis reveal that CXCL9, CXCL10 and CXCL11 were downregulated in ccRCC with 4p deletions. CD8+ T cell infiltration significantly deceased in 4q deletion tumors. These findings indicated that loss of 4q contributed to CD8+ T cell exclusion via downregulation of CXCL9, CXCL10 and CXCL11, which led to worse survival in patients with 4q deletions. In contrary to previous reports that gain of 5q and deletion of 3p were associated with better prognosis, we found that no arm SCNA correlated with prolonged survival with statistical significance (11,25).
Tumors with high arm SCNA level harbored higher tumor mutation burden, elevated infiltrations of macrophages and Treg cells. Treg cells and tumor associated macrophages contributed substantially to the suppression of antitumor T cell responses as they frequently accumulate in the tumor microenvironment (26). On the contrary, there were fewer NK cells and mast cells in arm SCNAhigh tumors. NK cells are considered important anti-cancer effector cells, as they can kill neoplastic cells presenting the MHC class I molecule (9). Mast cells could boost anti-tumor immunity and associate with prolonged survival in ccRCC as well (27). Markers and pathways referring to immune evasion were also upregulated in tumors with more arm SCNAs. Arm SCNA level correlated with markers of immune evasion and immunosuppressive immune cell infiltration, consistent with a mechanism related to gene dosage imbalance instead of functions of certain genes. Our findings suggested that arm SCNAs were closely associated with immune suppression in ccRCC. The altered tumor microenvironment conferred by 4q loss might also suggested a potential link between 4q loss and immunotherapy treatment response for metastatic renal cell carcinoma. Genomic instability and immune evasion in arm SCNAhigh tumors may contribute to the shortened survival in patients with high arm SCNA level.
However, some major limitations remained. This is a retrospective study without external validation. Cohort specific biases including patient ethnicity/race and clinical practice at the institution could affect our conclusions. These results will need to be further validated and confirmed in prospective randomized clinical trials.
Conclusions
In conclusion, we demonstrated the prognostic landscape of each arm SCNA in ccRCC and identified 4q deletion as independent adverse risk factors for both OS and RFS. Early stage ccRCC patients with 4q deletion had higher risk of death and recurrence. Loss of 4q contributed to cytotoxic cells exclusion via down regulation of CXCL9, CXCL10 and CXCL11. Higher arm SCNA burden correlated with worse survival and a more immunosuppressive tumor microenvironment.
Acknowledgments
Funding: This study was funded by grants from National Natural Science Foundation of China (81702496, 81702497, 81702805 and 81772696). All these study sponsors have no roles in the study design, in the collection, analysis, and in the interpretation of data.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Clinical Research Ethics Committee of Zhongshan Hospital, Fudan University with the approval number B2015-030.
References
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Cohen HT, McGovern FJ. Renal-cell carcinoma. N Engl J Med 2005;353:2477-90. [Crossref] [PubMed]
- Meskawi M, Sun M, Trinh QD, et al. A review of integrated staging systems for renal cell carcinoma. Eur Urol 2012;62:303-14. [Crossref] [PubMed]
- Motzer RJ, Ravaud A, Patard JJ, et al. Adjuvant Sunitinib for High-risk Renal Cell Carcinoma After Nephrectomy: Subgroup Analyses and Updated Overall Survival Results. Eur Urol 2018;73:62-8. [Crossref] [PubMed]
- Cahill DP, Kinzler KW, Vogelstein B, et al. Genetic instability and darwinian selection in tumours. Trends Cell Biol 1999;9:M57-60. [Crossref] [PubMed]
- Friedlander ML, Hedley DW, Taylor IW. Clinical and biological significance of aneuploidy in human tumours. J Clin Pathol 1984;37:961-74. [Crossref] [PubMed]
- Moch H, Presti JC Jr, Sauter G, et al. Genetic aberrations detected by comparative genomic hybridization are associated with clinical outcome in renal cell carcinoma. Cancer Res 1996;56:27-30. [PubMed]
- Palucka AK, Coussens LM. The Basis of Oncoimmunology. Cell 2016;164:1233-47. [Crossref] [PubMed]
- Davoli T, Uno H, Wooten EC, et al. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. Science 2017. [Crossref] [PubMed]
- Klatte T, Rao PN, de Martino M, et al. Cytogenetic profile predicts prognosis of patients with clear cell renal cell carcinoma. J Clin Oncol 2009;27:746-53. [Crossref] [PubMed]
- Chen M, Ye Y, Yang H, et al. Genome-wide profiling of chromosomal alterations in renal cell carcinoma using high-density single nucleotide polymorphism arrays. Int J Cancer 2009;125:2342-8. [Crossref] [PubMed]
- Liu J, Lichtenberg T, Hoadley KA, et al. An Integrated TCGA Pan-Cancer Clinical Data Resource to Drive High-Quality Survival Outcome Analytics. Cell 2018;173:400-16.e11. [Crossref] [PubMed]
- Gentles AJ, Newman AM, Liu CL, et al. The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat Med 2015;21:938-45. [Crossref] [PubMed]
- Newman AM, Liu CL, Green MR, et al. Robust enumeration of cell subsets from tissue expression profiles. Nat Methods 2015;12:453-7. [Crossref] [PubMed]
- Bindea G, Mlecnik B, Tosolini M, et al. Spatiotemporal dynamics of intratumoral immune cells reveal the immune landscape in human cancer. Immunity 2013;39:782-95. [Crossref] [PubMed]
- Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci U S A 2005;102:15545-50. [Crossref] [PubMed]
- Ciriello G, Miller ML, Aksoy BA, et al. Emerging landscape of oncogenic signatures across human cancers. Nat Genet 2013;45:1127-33. [Crossref] [PubMed]
- Fridman WH, Zitvogel L, Sautes-Fridman C, et al. The immune contexture in cancer prognosis and treatment. Nat Rev Clin Oncol 2017;14:717-34. [Crossref] [PubMed]
- Moore LE, Jaeger E, Nickerson ML, et al. Genomic copy number alterations in clear cell renal carcinoma: associations with case characteristics and mechanisms of VHL gene inactivation. Oncogenesis 2012;1:e14. [Crossref] [PubMed]
- Ito T, Pei J, Dulaimi E, et al. Genomic Copy Number Alterations in Renal Cell Carcinoma with Sarcomatoid Features. J Urol 2016;195:852-8. [Crossref] [PubMed]
- Klatte T, Kroeger N, Rampersaud EN, et al. Gain of chromosome 8q is associated with metastases and poor survival of patients with clear cell renal cell carcinoma. Cancer 2012;118:5777-82. [Crossref] [PubMed]
- Elfving P, Mandahl N, Lundgren R, et al. Prognostic implications of cytogenetic findings in kidney cancer. Br J Urol 1997;80:698-706. [Crossref] [PubMed]
- La Rochelle J, Klatte T, Dastane A, et al. Chromosome 9p deletions identify an aggressive phenotype of clear cell renal cell carcinoma. Cancer 2010;116:4696-702. [Crossref] [PubMed]
- Gunawan B, Huber W, Holtrup M, et al. Prognostic impacts of cytogenetic findings in clear cell renal cell carcinoma: gain of 5q31-qter predicts a distinct clinical phenotype with favorable prognosis. Cancer Res 2001;61:7731-8. [PubMed]
- Speiser DE, Ho PC, Verdeil G. Regulatory circuits of T cell function in cancer. Nat Rev Immunol 2016;16:599-611. [Crossref] [PubMed]
- Fu H, Zhu Y, Wang Y, et al. Tumor Infiltrating Mast Cells (TIMs) Confers a Marked Survival Advantage in Nonmetastatic Clear-Cell Renal Cell Carcinoma. Ann Surg Oncol 2017;24:1435-42. [Crossref] [PubMed]


