
Attitude and behavior of clinical nurse towards self-health care: a cross-sectional survey
Introduction
Nurses are a vital workforce for the health of the population and also a challenging occupation which requires physical endurance, emotional intelligence, and mental clarity. Hospital nursing entails several work-related physical and psychosocial health risk factors. Some of these factors cannot be avoided completely, such as lifting patients, shift working, and working with infectious patients and their body fluids. Nurses’ job demands may lead to health problems such as low back pain, skin problems and mental health problems. Nurses must strive to balance the demands of the workplace and their personal lives to maintain their own health, physically and psychologically (1,2).
Studies reported that nurses were at high risk of work-related musculoskeletal disorders with prevalence rates for neck, shoulder or lower back disorders for nurses (3). Needle stick and other sharp injuries are also a concern, with two thirds of all reported sharps injuries occurring in nurses. While many infections can be transmitted through a sharps injury, hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV) are the most consequential. Apart from infectious risks, 4.0–4.6% of all health care workers, including nurses, were allergic to latex, resulting in conditions such as dermatitis, asthma and rhinoconjunctivitis (4,5). Nurses are also vulnerable to depression given that work stress precipitates depression in working women and men (2,6).
Researches usually focus on the risk factors affecting the health of nurses other than on the particular behavior pattern of nursing professional workers when the injuries and diseases happen. Most of these risk factors are unavoidable, while the behavior pattern of nursing professional can be modulated and changed via education and dialogue.
When it comes to behavior pattern of nursing profession, self-prescribing may be a matter of concern for several reasons. Firstly, self-treatment can lead to delayed diagnosis and treatment, even worsening of the illness because of lack of objectivity and professional distance (7). Secondly, many diseases need follow-up apart from medication, particularly for mental illness and chronic diseases which is the major suffer in health workers. Thirdly, self-prescribing may be an indicator that the health worker is neglecting his or her own health (8-10).
Methods
A questionnaire was sent out to all 620 nurses in department of surgery in PUMCH and the resultant final version of the survey is appended (see questionnaire, Supplementary content, which illustrates the questionnaire employed in this study). It consisted of 28 items which asked about the use of medical services and medications when they were ill, demographic information as well as specialty, educational background, clinical experience, and attitude to the disease as well. Three rounds of online questionnaire were done between December 2016 and February 2017. This work was approved by Peking Union Medical College Hospital Ethics committee (ID: S-K 752), and all the subjects had signed the informed consent forms.
The data were analyzed using descriptive statistics and comparison of proportions. The primary outcome measures were (I) whether respondents consulted doctor when he or she suffered last illness, (II) whether respondents follow trust their physician and (III) what is the attitude to the occupation stress. The chi-square test was employed to test for the significance of the difference between group proportions. A P value <0.05 was considered statistically significant. IBM SPSS 20.0 (Statistical Package for the Social Sciences software, version 20.0) was used for data analysis.
Results
Demographic data
Four hundred and seventy-seven subjects had responded to the questionnaire online in auto-administrated form (a 76.9% response rate). Only 12 of the respondents were male. The majority of the respondents were younger than 40 years old (83.02%). The survey indicated that 44.44% (N=212) of respondents did not consult physician. Instead, they self-managed their illness, with 60.38% (N=128) of non-consulters taking some medications, 34.91% (N=74) doing nothing and 2.83% (N=6) doing other things like investigations, seeking physiotherapy or consulting alternative health practitioners. Table 1 shows the distribution and statistically significant characteristics of nurse respondents who consulted medical practitioner. Education background (P=0.027) and income (P=0.010) were found to be the main factor affecting whether a doctor was consulted.

Full table
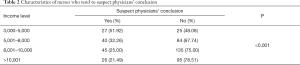
Characteristics of nurses who tend to suspect physicians’ conclusion
Income was the only factor that found with significance in suspecting physicians’ conclusion. There were 51.92% of nurses tending to suspect the physicians’ conclusion in the lower income group (less than 5,000 RMB), while only 21.49% (N=26, more than 10,000 RMB) in higher income (P<0.001, Table 2). What make this more serious is that there were 59.62% nurses would show a passive health-seeking behavior, not seek for help from specialist physician, because of the lower income (Q22).
Full table
However, income is a social factor which depends on many other influencing factors including education background, working experience, and working department. Though we did find income was related to education background, the difference was not significant when directly comparing the proportion of nurses tending to suspect physician’s conclusion in groups of different degrees.
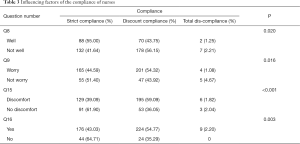
Factors influence the compliance of nurses
The main influencing factors to this behavior were the attitude items. Those who self-evaluated with well physical condition show higher strict compliance (55.00% vs. 41.64%), lower discount-compliance (43.75% vs. 56.15%), and lower total ignorance (1.25% vs. 2.21%), compared with those who self-evaluated not well (P=0.020, Q8). Nurses with anxiety about their health including worrying about being ill were less likely to ignore the doctor’s advice (P=0.016, Q9).
It is interesting that those who were suffering from some discomfort showed a lower strict compliance (39.09% vs. 61.90%), and a higher discount-compliance (59.09% vs. 36.05%) than those not felt uncomfortable (P<0.001, Q15). It is the same with the nurses who thought working stress would impact one’s health complied less strictly with physicians’ advise (43.03% vs. 64.71%), and more discount-compliance (54.77% vs. 35.29%) (P=0.003, Q16) (Table 3).
Full table
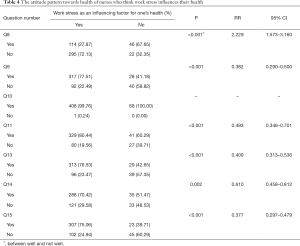
Attitude pattern towards health of nurses who think work stress influences their health
All respondents except one considered it was with equal importance between psychological and physical health. This is consistent with the result that the respondents who thought the work stress was the influencing factor to the health were more likely to feedback a poor health status (72.13% vs. 32.35%, Q8), worry about their health (77.51% vs. 41.18%, Q9), fear to suffer from a disease (80.44% vs. 60.29%, Q11; 70.42% vs. 51.47%, Q14), and complain about suffering from pain or discomfort (76.53% vs. 42.65%, Q13; 75.06% vs. 39.71%, Q15) (Table 4).
Full table
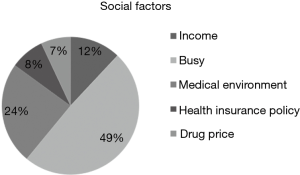
Social factors influence one’s health-seeking behavior
There were 69.39%, 24.74%, and 4.19% of respondents had their last physical examination within 1, 1–3, and longer than 3 years, respectively. Meanwhile, 1.68% respondents never went for physical examination. Forty-nine percent of the respondents considered the busy work or schedule was the reason of one’s skipping of the physical examination or doing nothing at last illness; 24% thought the medical environment contributed to this. In contrast, only 15% of respondents owed this behavior to the economic factors, including the health insurance policy and drug price. Interestingly, only 12% of them chose income as an influencing factor to their health-seeking behavior (Figure 1).
Discussion
This is a rare study to investigate the attitude and behavior of nurses to psychological and physical health. We found that nearly half of the respondents did not consult physician for last illness, either physically or emotionally. Instead, they self-managed their illness, with 60.38% of non-consulters taking some medications. The choice of asking respondents to recall when they were last ill was deliberately set. We hoped to encourage respondents to take both mental and emotional conditions into consideration when answering the question. This undifferentiated wording does prevent us from specifically assessing the correctness of the respondent’s management decision. We are unable to judge whether it was an appropriate consultation when nurses seek medical attention the last time, they were ill. We can only observe that the patient’s perceived illness was that they felt they needed to see a doctor. Similarly, for nurses who chose to self-prescribing, their perception of being ill did not warrant seeing a doctor but ill enough to take prescription medication.
Nurses are a different population from the public, but they still get ill and perception of illness varies from individual to individual. Being trained nurses, with the knowledge and resources to take care of themselves they can and do self-prescribing as self-managed when being ill. The nurses could play an important role in supplementary prescribing to fill the gaps left by lack of doctors. However, the safety of prescribing is worrying because nurses tend to receive insufficient training. It is acceptable and preferable to self-treat for minor illness, but when it comes to chronic disease self-treat should be avoided for it can result in worsening the illness (11,12).
The people with anxiety about one’s health, in another word worrying about being ill, showed less likely to ignore the doctor’s advice. Those who self-evaluated with well physical condition showed higher strict compliance and lower discount-compliance or total ignorance. It is interesting that those who were suffering from some discomfort showed a lower strict compliance than those who did not feel uncomfortable. It is the same with the nurses who thought working stress could impact one’s health would comply strictly with physicians’ advice and discount-compliance. The patient’s belief on their illness will affect their compliance, which has a great impact on the treatment effect of the disease, leading to insufficient treatment effect for the patient, especially for the patients with chronic diseases such as hypertension (13,14).
What’s more, respondents who thought the work stress was the influencing factor to the health were more likely to feedback a poor health status, worry about their health, fear to suffer from a disease, and complain about suffering from pain or discomfort. We can speculate that the work stress can cause physiological anxiety which can be explained for stress symptoms. What we should do is to guide nurses to manage the working stress correctly and properly, which comes from the intense work load and the reactivity to it (15,16).
Single center and cross-sectional design are the prominent weakness in our study. We do hope to call for multiple centers such as hospitals in urban or rural, special or comprehensive hospitals in the future. Besides, nurses from different departments, especially intense occupation stress department such as ICU and emergency department, should be included or specifically analyzed. About 83.02% of respondents are younger than 40 years old, which may result in selection bias. The relationship between behavior and gender needed to explore and verify because only 12 (2.52%) of the respondents are male nurses. More large range survey and study is wanted in the future.
Conclusions
This study provides some preliminary information about the attitude and health seeking behavior of nurses in PUMCH. The findings that about half of nurses self-treat, with a large proportion self-prescribing, and do not comply with the doctor’s advice suggest that hospital nurses is a population with personal health care practices which warrant a closer look.
Supplementary
Questionnaire survey
Survey on disease attitude and health-seeking behavior in nursing population
Question 1 . Your gender
Male
Female
Question 2 . Your marriage status
Married
Single
Divorced
Widowed
Question 3 . Your age
20–29
30–39
40–49
50–59
Question 4 . Your education background
Medical technical degree
College degree
Bachelor degree
Master and other higher degree
Question 5 . Your income standard (Rmb/m)
3,000–5,000
5,001–8,000
8,001–10,000
>10,001
Question 6 . Year of working experience (including intern /year)
1–5
6–10
11–15
16–20
>20
Question 7 . Your working department (Please choose ONE only)
Inpatient
Outpatient
Emergency
ICU
Surgery
Supply room
Others Please specify____________________
Question 8 . Your physical condition during your service? (Please choose ONE only)
Good
Ordinary
Not good
Bad
Question 9 . Do you worry about your health condition?
Yes
No
Question 10 . Do you think that psychological health is with less importance than physical health?
Yes
No
Question 11 . Are you anxious that you may be suffering from a disease?
Yes
No
Question 12 . In what degree you believe you were suffering from a disease? (Please choose ONE only)
0~10%
10~20%
20~50%
50~80%
80% or more
Question 13 . Have you been bothered by the pain of any body parts?
Yes
No
Question 14 . When you witness or learn about one disease from a book or a colleague, in your workplace, will you worry that you would suffer from the disease?
Yes
No
Question 15 . Have you been bothered by any physical discomfort?
Yes
No
Question 16 . Do you think your work stress is an influencing factor on your physical and psychological condition?
Yes
No
Question 17 . Do you think that nursing work is more likely to have a negative impact on health than doctor’s work?
Yes
No
Question 18 . Your last physical examination /health check-up time? (Please choose ONE only)
Within 1 year
1~3 years
>3 years
Never
Question 19 . The main reason for your skipping of physical examination recently? (Please choose ONE only)
Busy
Physical examination is not necessary
Fear of malignancy-related positive examination results
Others Please specify____________________
Question 20 . How do you deal with it when you feel uncomfortable? (Please choose ONE only)
Treat myself with experience and buy medicine myself
Endure the pain, do nothing, go through it
Consult my doctor colleague
Seek for medical treatment
Question 21 . What factors will affect your medical treatment? (Can choose more than one)
Income
How busy
Medical environment
Health insurance policy
The price of drugs
Question 22 . Did you seek for the specialist physician during your last illness including physical and psychological illness?
Yes (to Question 25)
No (to Question 23)
Question 23 . If you did not go to specialist physician, how did you treat with it? (Please choose ONE only)
Nothing
Taking drugs therapy (to Question 24)
Others Please specify____________________
Question 24 . What type of dugs did you administrate? (Please choose ONE only)
Prescription drugs
Non-prescription drugs
Both
Question 25 . When did you consulted with a professional physician last time? (Consultation means any time, any occasion to seek help from a professional physician) (Please choose ONE only)
Within 1 week
Within 1 month
Within 1 year
More than 1 year
Question 26 . In what way did you consult your professional physician last time? (Please choose ONE only)
Outpatient registration
Consult my doctor colleague by chance in work place
Consult by telephone/SMS and other methods
Others Please specify____________________
Question 27 . When a professional doctor told you that you do not have to worry about your physical and psychological condition, do you think it is hard to believe?
Yes
No
Question 28 . Do you have good compliance with your doctor’s advice (including health advice, medication)? (Please choose ONE only)
Strict compliance
Follow a part of advice
Completely do not follow, because I have my own judgments
——Thank you for participating in our survey——
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This work was approved by Peking Union Medical College Hospital Ethics committee (ID: S-K 752), and all the subjects had signed the informed consent forms.
References
- Ketelaar SM, Nieuwenhuijsen K, Frings-Dresen MH, et al. Exploring novice nurses' needs regarding their work-related health: a qualitative study. Int Arch Occup Environ Health 2015;88:953-62. [Crossref] [PubMed]
- Welsh D. Predictors of depressive symptoms in female medical-surgical hospital nurses. Issues Ment Health Nurs 2009;30:320-6. [Crossref] [PubMed]
- Reed LF, Battistutta D, Young J, et al. Prevalence and risk factors for foot and ankle musculoskeletal disorders experienced by nurses. BMC Musculoskelet Disord 2014;15:196. [Crossref] [PubMed]
- Tarlo SM, Arif AA, Delclos GL, et al. Opportunities and obstacles in translating evidence to policy in occupational asthma. Ann Epidemiol 2018;28:392-400. [Crossref] [PubMed]
- White GE, Mazurek JM, Moorman JE. Asthma in health care workers: 2008 and 2010 Behavioral Risk Factor Surveillance System Asthma Call-back Survey. J Occup Environ Med 2013;55:1463-8. [Crossref] [PubMed]
- Perry L, Lamont S, Brunero S, et al. The mental health of nurses in acute teaching hospital settings: a cross-sectional survey. BMC Nurs 2015;14:15. [Crossref] [PubMed]
- Chiu YL, Kao S, Lin HC, et al. Healthcare Service Utilization for Practicing Physicians: A Population-Based Study. PLoS One 2016;11:e0130690. [Crossref] [PubMed]
- Drennan VM, Grant RL, Harris R. Trends over time in prescribing by English primary care nurses: a secondary analysis of a national prescription database. BMC Health Serv Res 2014;14:54. [Crossref] [PubMed]
- Topor G, Grosu IA, Ghiciuc CM, et al. Awareness about antibiotic resistance in a self-medication user group from Eastern Romania: a pilot study. PeerJ 2017;5:e3803. [Crossref] [PubMed]
- Saleem Z, Saeed H, Ahmad M, et al. Antibiotic Self-Prescribing Trends, Experiences and Attitudes in Upper Respiratory Tract Infection among Pharmacy and Non-Pharmacy Students: A Study from Lahore. PLoS One 2016;11:e0149929. [Crossref] [PubMed]
- Nazareth I, Murray E. Promoting self care for minor illness. BMJ 2010;340:c2913. [Crossref] [PubMed]
- Jamshed SQ, Wong PS, Yi HC, et al. Self-medication practices among female students of higher educational institutions in Selangor, Malaysia: A quantitative insight. J Pharm Bioallied Sci 2016;8:217-22. [Crossref] [PubMed]
- Simon GE, Peterson D, Hubbard R. Is treatment adherence consistent across time, across different treatments and across diagnoses? Gen Hosp Psychiatry 2013;35:195-201. [Crossref] [PubMed]
- Sheehan DV, Keene MS, Eaddy M, et al. Differences in medication adherence and healthcare resource utilization patterns: older versus newer antidepressant agents in patients with depression and/or anxiety disorders. CNS Drugs 2008;22:963-73. [Crossref] [PubMed]
- Puntil C, York J, Limandri B, et al. Competency-based training for PMH nurse generalists: inpatient intervention and prevention of suicide. J Am Psychiatr Nurses Assoc 2013;19:205-10. [Crossref] [PubMed]
- Lygnugaryte-Griksiene A, Leskauskas D, Jasinskas N, et al. Factors influencing the suicide intervention skills of emergency medical services providers. Med Educ Online 2017;22:1291869. [Crossref] [PubMed]


