Associations between seasonal variation and post-operative complications after total hip arthroplasty
Introduction
Post-operative complications following total hip arthroplasty (THA) are infrequent (1,2), and occur on average in less than 1% to 2% of patients (3,4). However, when major medical or surgical complications occur, such as periprosthetic joint infections, pneumoniae or pulmonary emboli, they may amount to a large morbidity, financial, and time burden to patients and healthcare providers and may result in poor patient outcomes (3-9). Therefore, it is important to understand the risk factors associated with each of these complications, in order to attempt to mitigate them appropriately during peri-operative period.
One hypothesized risk factor for the increased rate of post-operative complications is seasonal variation. An observational cohort study analyzing data from the American College of Surgeons-National Surgical Quality Improvement Program database (ACS-NSQIP) database on overall surgeries noted an 18% increase in post-operative morbidity in the July 1 to August 30 cohort (n=9,941) when compared to the April 15 to June 15 cohort (n=10,313) (P=0.0005). A 41% increase in mortality between patient populations depending on the time of year was also noted (P=0.005) (10). The etiologies for this seasonal variation in outcomes have been attributable to both changes in weather patterns and changes in house-staff. For example, the “July effect” has been proposed to explain this variation, based on the hypothesis that inexperienced staff at the beginning of an academic year can lead to potentially increased rates of complications (11-13). Particularly in orthopedics, Gruskay et al. demonstrated a statistically significant increase in post-operative infection rate in summer (4.1%) vs. spring (2.8%; P=0.03) following spine surgery (13). Furthermore, Durkin et al. confirmed the higher rate of superficial skin infection following spine surgery during the summer, and since their study was performed in a nonteaching hospital, they attributed the increases in the rate of complications during the summer to be related to ecological and/or environmental factors rather than the July effect (14).
Similar findings indicating seasonal variation of complications following elective total hip or knee arthroplasty at a single institution have been reported by Kane et al. (15). In their study analyzing 750 patients over 1-year period, they found an increase in the incidence of infection during summer months. Therefore, the purpose of our paper was to investigate the association between seasonal variation, and the 30-day post-operative complication rates following THA. Specifically, we evaluated a large prospectively collected national database for: (I) the overall complication rates; (II) seasonal variations in incidence; and (III) specific quarter (Q), if any, associations.
Methods
Data source
The ACS-NSQIP was used to identify patients who underwent primary, elective THA (16). NSQIP is a leading validated, risk-adjusted, outcomes-based program that aggregates peri-operative data (preoperative co-morbidities, intra-operative variables, 30-day post-operative complications) for patients undergoing major surgeries (17,18). A main purpose of this database is to provide surgeons, hospitals, and healthcare systems verified data in order to help save costs, reduce complications, and improve overall patient outcomes. Metrics such as complications, comorbidities, patient demographics, and Current Procedural Terminology (CPT) codes are collected for hundreds of thousands of patients from all across the country from the pre-operative through 30-day post-operative window. The data entered in the database is collected and verified by a surgical clinical reviewer (19). As this data is publically available and contains de-identified patient data, the Institutional Review Board determined this study to be exempt.
CPT code
CPT codes are a universally used system in order to classify and identify medical, surgical, and laboratory procedures or services performed by physicians. Three categories of CPT codes exist: category 1, 2, and 3. Category 1 codes are used to identify procedures or services directly performed by the physician. Category 2 CPT code are supplemental tracking codes and are often used optionally. Category 3 CPT codes are designated to new and developing technology, procedures, and services (20). Specifically, in this study, we used category 1 CPT code 27130.
Study population
We included all patients who underwent THA from January 1st, 2011 to December 31st, 2015 who had been designated within NSQIP using CPT code 27130. A total of 102,692 patients were identified, and appropriate patient demographics were collected and collated including age, gender, race, reported American Society of Anesthesiologists (ASA) classification (21,22), body mass index, smoking status, independent functional status, anesthesia type, comorbidities (congestive heart failure, chronic obstructive pulmonary disease, diabetes, dialysis, disseminated cancer, bleeding disorder, corticosteroid use, weight loss, and ascites) (Table 1). There were a total of 45,956 (45%) men and 56,736 (55%) women who had a mean age of 65 years (range, 18–89 years).
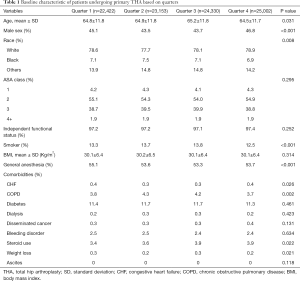
Full table
30-day post-operative complications
Using this patient population of interest, we assessed the incidence rates for the following 30-day post-operative complications: readmission, reoperation, mortality, superficial surgical site infection, deep surgical infection, dehiscence, deep vein thrombosis (DVT), pulmonary embolism (PE), pneumonia, urinary tract infection (UTI), renal failure, re-intubation, ventilator use for greater than 48 hours, renal insufficiency, stroke, cardiac arrest, myocardial infarction, transfusion, sepsis, and septic shock for each quarter of the year (Table 2). Quarter 1 (Q1) was defined from January 1st to March 31st, quarter 2 (Q2) from April 1st to June 30th, quarter 3 (Q3) from July 1st to September 30th, and quarter 4 (Q4) from October 1st to December 31st.
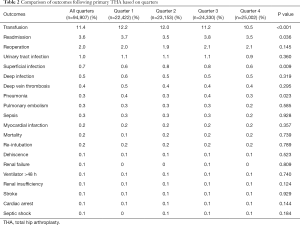
Full table
Data analysis
The overall number of THA patients from each quarter of the year was determined and aggregated across the 5 years of interest (2011 to 2015), and used to determine the relative occurrence of complications. To identify potential statistical significance between categorical variables, chi-squared tests were performed. Analysis of variance (ANOVA) tests were analogously conducted to identify potential statistical significance among continuous variables. Univariate regression analysis was performed to compare the 30-day post-operative complications of primary THA between the different quarters (Q2 vs. Q1, Q3 vs. Q1, Q4 vs. Q1) using appropriate P values (Table 3). Multivariate regression was analogously performed to adjust for potential confounding bias (Table 4). All the baseline variables which showed a difference between THA and total knee arthroplasty (TKA) at a significance level of P<0.01 were included in the multivariate analysis. Odds ratios (OR, odds of having particular complication during particular quarter relative to overall incidence rate) and 95% confidence intervals (CI) were calculated for different outcomes to identify any statistically significant changes in the incidence rates of associated 30-day post-operative complications between the different quarters. The level of significance for all analysis was set at P<0.05. Statistical analysis was performed using R software (version 3.1.3, Vienna, Austria).
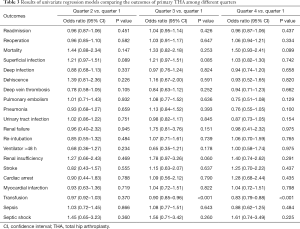
Full table
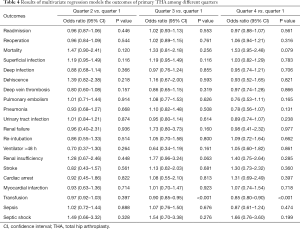
Full table
Results
THA complication rates
The overall complication rate in this cohort was 1.09%. Upon tabulation of the different post-operative THA complication incidence rates sorted by quarters (Table 2), 16 out of 20 outcomes had <1% incidence rate, 3 had between a 1% and 5% incidence rate, and 1 outcome had a complication rate greater than 5% (bleeding transfusion). Overall, the 30-day post-operative complication rates were as follows: transfusion (11.4%), readmission (3.6%), reoperation (2.0%), UTI (1.0%), superficial surgical site infection (0.7%), deep surgical infection (0.5%), DVT (0.4%), pneumonia (0.3%), PE (0.3%), sepsis (0.3%), myocardial infarction (0.2%), mortality (0.2%), re-intubation (0.2%), dehiscence (0.1%), renal failure (0.1%), ventilator use for greater than 48 hours (0.1%), renal insufficiency (0.1%), stroke (0.1%), cardiac arrest (0.1%), and septic shock (0.1%).
Correlation between seasonal variation and THA complication rates
There was no statistical significance difference among 19 of the 20 complication rates between the different quarters. Transfusion was the only complication with a statistically significant difference (P value <0.001) between the different quarters. It was also the only complication with a complication rate above 10% for all seasons (Q1 =12.2%, Q2 =12.0%, Q3 =11.2%, Q4 =10.5%).
Individual quarter comparison
Comparison of post-operative complication rates of THA between individual different quarters (Q2 vs. Q1, Q3 vs. Q1, Q4 vs. Q1) (Table 3) performed revealed no statistical significant difference for the majority of outcomes examined; only transfusion was different. The rates of blood transfusion were highest in Q1 and lowest in Q4. Multivariate regression analysis yielded similar results to that of univariate regression analysis (Table 4). Patients in Q3 (OR, 0.90; 95% CI, 0.85–0.95; P<0.001) and Q4 (OR, 0.85; 95% CI, 0.80–0.90; P<0.001) were at lower risk of transfusion.
Discussion
Quarterly or seasonal changes in staffing and weather patterns can influence the outcomes of procedures depending on the time of the year in which the surgery was performed. However, quarterly variations in the incidence of 30-day complications after THA have not been well-established. Therefore, the present study identified 102,682 THA surgeries listed in ACS-NSQIP database and evaluated the incidence of 30-day complications. We found no statistically significant differences in the incidence rates of 30-day complications after THA surgery between the different seasons. The only exception was blood transfusion, which had the highest rate in Q1 and the lowest in Q4. It is important to note that among blood transfusions, the mean complication rate was 11.5%+/−1.0%, and the statistical significance identified may have been the result of the large power of the test (n=102,682 surgeries) rather than an intrinsic seasonal variation in post-operative THA complication rates.
There are some limitations to our study. Our results are limited by the accuracy of reported data on the NSQIP database, although inter-rater disagreement is approximately 2%, suggesting reliable use of this data (23). Our data is limited to the 30-day complications of post-operative THA surgery as reported by NSQIP. However, the use of 102,682 patients provides a large sample size that allows us to find associations. NSQIP includes surgeries performed in over 700 hospitals all across North America, some of which are in regions that have more pronounced temperature fluctuations throughout the year than others. However, while the range of temperature during a season might vary by region, the timeframe, or quarter, defining that season remains constant throughout the country. Nevertheless, since the ACS-NSQIP does not allow for regional narrowing, future studies using a database which allows for narrowing based on geographic location and comparison of the seasonal variations and THA complications should be conducted now that this nationwide study has been performed. Although we adjusted for a number of baseline variables, some potential confounding variables may not have been included in the study. However, as most complications did not show a difference, including other variables in the multivariate model is unlikely to have changed our results.
The lack of association between seasonal variation and rate of 30-day post-operative complications after THA variation for the majority of complications examined (19 out of 20) suggests that elective THA surgery does have to be scheduled around specific times of the year. Furthermore, our findings are aligned with the study by Bohl et al., that showed the inexistence of a “July effect” (hypothetical increase in morbidity thought to be associated with the training of new residents during the first portion of the academic year) in their analysis of the NSQIP database among 21,434 patients who underwent primary THA and TKA. They found no association of an interaction term for academic quarter and resident involvement with “serious adverse events” (P=0.656) or “any adverse events” (P=0.578) (24).
Conclusions
Our results indicate that overall there is no correlation between seasonal variation and 30-day complication rates following THA surgery. The exception to our findings was the occurrence of bleeding transfusions, whereby later months (Q3 and Q4, July to December) had statistically significant increases in transfusion rates required relative to Q1 (January, February, March). The authors cannot currently provide any particular reason as to why a correlation exists between transfusion and time of year. Nevertheless, based on these findings, in addition to standard of care, if a hospital wanted to decrease transfusion rates, there could be a more focused monitoring of patient’s pre-operative factors such as hemoglobin, as well as an intra-operative focus on coagulation. As the explanation for these findings remains unclear, further exploration into this correlation would make for an excellent future study. The findings from this study suggest that elective THA surgery can be scheduled during any specific time of the year without affecting the 30-day post-operative complications. This information is helpful in counselling patients while scheduling THAs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: As this data is publically available and contains de-identified patient data, the Institutional Review Board determined this study to be exempt.
References
- Pivec R, Johnson AJ, Mears SC, et al. Hip arthroplasty. Lancet 2012;380:1768-77. [Crossref] [PubMed]
- Hunt LP, Ben-Shlomo Y, Clark EM, et al. 90-day mortality after 409 096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 2013;382:1097-104. [Crossref] [PubMed]
- Zhan C, Kaczmarek R, Loyo-Berrios N, et al. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am 2007;89:526-33. [PubMed]
- SooHoo NF, Farng E, Chambers L, et al. Comparison of Complication Rates Between Hemiarthroplasty and Total Hip Arthroplasty for Intracapsular Hip Fractures. Orthopedics 2013;36:e384-9. [Crossref] [PubMed]
- Mont MA, Jones LC, Rajadhyaksha AD, et al. Risk factors for pulmonary emboli after total hip or knee arthroplasty. Clin Orthop Relat Res 2004.154-63. [Crossref] [PubMed]
- Chughtai M, Gwam CU, Mohamed N, et al. The Epidemiology and Risk Factors for Postoperative Pneumonia. J Clin Med Res 2017;9:466-75. [Crossref] [PubMed]
- Perfetti DC, Boylan MR, Naziri Q, et al. Have Periprosthetic Hip Infection Rates Plateaued? J Arthroplasty 2017;32:2244-7. [Crossref] [PubMed]
- Gwam CU, Mistry JB, Mohamed NS, et al. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty 2017;32:2088-92. [Crossref] [PubMed]
- Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 2003;85-A:27-32. [Crossref] [PubMed]
- Englesbe MJ, Pelletier SJ, Magee JC, et al. Seasonal variation in surgical outcomes as measured by the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg 2007;246:456-62; discussion 463-5. [Crossref] [PubMed]
- Bakaeen FG, Huh J, LeMaire SA, et al. The July Effect: Impact of the Beginning of the Academic Cycle on Cardiac Surgical Outcomes in a Cohort of 70,616 Patients. Ann Thorac Surg 2009;88:70-5. [Crossref] [PubMed]
- Phillips DP, Barker GE. A July Spike in Fatal Medication Errors: A Possible Effect of New Medical Residents. J Gen Intern Med 2010;25:774-9. [Crossref] [PubMed]
- Gruskay J, Smith J, Kepler CK, et al. The seasonality of postoperative infection in spine surgery. J Neurosurg Spine 2013;18:57-62. [Crossref] [PubMed]
- Durkin MJ, Dicks KV, Baker AW, et al. Postoperative infection in spine surgery: does the month matter? J Neurosurg Spine 2015;23:128-34. [Crossref] [PubMed]
- Kane P, Chen C, Post Z, et al. Seasonality of Infection Rates After Total Joint Arthroplasty. Orthopedics 2014;37:e182-6. [Crossref] [PubMed]
- Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 1998;228:491-507. [Crossref] [PubMed]
- ACS NSQIP Participant Use Data File. Available online: https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use
- Khuri SF, Henderson WG, DePalma RG, et al. The NSQIP: a new frontier in surgery. Surgery 2005;138:837-43. [Crossref] [PubMed]
- Complete Data for Complete Understanding: the ACS NSQIP Advantage. Available online: https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqipoverview1012.ashx
- AAPC. Current Procedural Terminology (CPT) Codes. Available online: https://www.aapc.com/resources/medical-coding/cpt.aspx
- Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 1978;49:239-43. [Crossref] [PubMed]
- Wolters U, Wolf T, Stutzer H, et al. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth 1996;77:217-22. [Crossref] [PubMed]
- Shiloach M, Frencher SK, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6-16. [Crossref] [PubMed]
- Bohl DD, Fu MC, Golinvaux NS, et al. The “July Effect” in Primary Total Hip and Knee Arthroplasty: Analysis of 21,434 Cases From the ACS-NSQIP Database. J Arthroplasty 2014;29:1332-8. [Crossref] [PubMed]


