Reconstruction of the medial patellofemoral ligament reconstruction for patients with recurrent patellar dislocation: review of surgical techniques and tips to achieve successful reconstruction
Patellofemoral problems are among the most common causes of knee pain in young and adolescent patients (1). Incidence rates published in the American Journal of Sports Medicine for ages 10–18 were found to be approximately 29 per 100,000 people per year (2). Patellar instability is a non-specific term that includes several sub-diagnoses: each type of instability has a functional or anatomical cause that should be treated according to its specific aetiology (3).
Sub-definitions include:
- Patellofemoral syndrome—pain during extension of the knee;
- Patella mal-tracking—dynamic scroll incongruence between patella and trochlea;
- Patella malalignment—an anatomic incongruence of the patella and trochlea;
- Dysplasia, referring to growth abnormality.
Annual incidence rate of primary patellar dislocations is 43/100,000 (4).
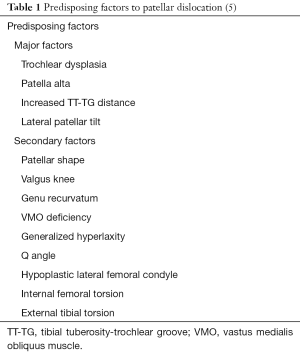
It is important to highlight that medial patellar-femoral ligament (MPFL) rupture is the result of a patella dislocation, not a cause of dislocation, so MPFL-reconstruction alone is not sufficient for a complete recovery. The major risk factors for patellar instability have been clearly highlighted in current literature (Table 1) and include; trochlear dysplasia, patella alta, lateralized tibial tubercle (increased TT-TG distance), patellar laterale tilt (5,6).
A great many surgical techniques have been developed to manage this, but they can be divided in 5 broad groups: free graft fixed in bone canals, free graft fixed with anchors, free graft sutured to periosteum, reconstruction with the central portion of the quadriceps tendon and reconstruction using the semitendinosus tendon maintaining its insertion at the pes anserinus (7).
All these techniques either respect the anatomy of the MPFL or can reproduce the action of the MPFL.
The importance of an anatomically accurate reconstruction has been demonstrated by biomechanical tests using different graft and techniques on cadavers. A study evaluating the MPFL in its natural orientation demonstrates that although the procedures achieved safe fixation of the graft at the femoral attachment, the single-bundle techniques reported failure rates of 11% at the patellar side due to patellar fracture. In addition, the anatomical techniques can better restore the function of the native ligament, minimizing tension errors thanks to the double arms of the graft (8,9).
Positioning of the graft within the right reference points has been demonstrated to be crucial: the proximal third of the medial patella for the patellar insertion, and at a specific point distal to the tubercle of the adductor and posterior to the medial femoral epicondyle for the femur (10).
The correct placement of anatomical insertions of the graft avoids producing extension or flexion deficits of the knee, as well as secondary patella alta.
In a systematic review of 2012 that analyses the complications and failures of the various reconstructions of MPFL, it has been shown that excessive medial tension should be avoided, because this can cause severe chondral damage, worse than external tension (11).
There are some tricks that can be used to optimise the tension of the graft: for instance, the tension of the neo-MPFL should be applied without the tourniquet to prevent faulty tensioning due to the effect of the pneumatic constraint.
Because the reconstructed ligament has a higher strength than the native ligament with a lower elasticity, it does not require excessive tension to be maintained. Rebuilding the MPFL is akin to putting a brake on the knee cap, so there is no need to place it under very high tension in order to avoid errors.
Although the study of Kumahashi et al. has shown that the medial stiffness decreases greatly in the two postoperative years it is important to not place too much emphasis on this. More important than stiffness is the elasticity of the neo MPFL; elasticity of the graft is smaller compared to the native ligament, thus the lateral movement is reduced despite reduced tension than the native MPFL, and this is enough to save the patella from the dislocation.
A good way to reduce medial tension is to fix the graft at 60° of flexion so as to have the patella engaged within the femoral trochlea. This allows the ligament to be fixed under optimal tension, improving the results of the procedure (11).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vavken P, Wimmer MD, Camathias C, et al. Treating patella instability in skeletally immature patients. Arthroscopy 2013;29:1410-22. [Crossref] [PubMed]
- Mehta VM, Inoue M, Nomura E, et al. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc 2007;15:78-81. [Crossref] [PubMed]
- Redziniak DE, Diduch DR, Mihalko WM, et al. Patellar instability. J Bone Joint Surg Am 2009;91:2264-75. [PubMed]
- Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-5. [Crossref] [PubMed]
- Antinolfi P, Bartoli M, Placella G, et al. Acute patellofemoral instability in children and adolescents. Joints 2016;4:47-51. [PubMed]
- Lewallen L, McIntosh A, Dahm D. First-Time Patellofemoral Dislocation: Risk Factors for Recurrent Instability. J Knee Surg 2015;28:303-9. [Crossref] [PubMed]
- Lind M, Jakobsen BW, Lund B, et al. Reconstruction of the medial patellofemoral ligament for treatment of patellar instability. Acta Orthop 2008;79:354-60. [Crossref] [PubMed]
- Placella G, Speziali A, Sebastiani E, et al. Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single-bundle technique. Musculoskelet Surg 2016;100:103-7. [Crossref] [PubMed]
- Hinterwimmer S, Imhoff AB, Minzlaff P, et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc 2013;21:2147-54. [Crossref] [PubMed]
- Placella G, Tei MM, Sebastiani E, et al. Shape and size of the medial patellofemoral ligament for the best surgical reconstruction: a human cadaveric study. Knee Surg Sports Traumatol Arthrosc 2014;22:2327-33. [Crossref] [PubMed]
- Shah JN, Howard JS, Flanigan DC, et al. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 2012;40:1916-23. [Crossref] [PubMed]