The evolution of surgical telementoring: current applications and future directions
Introduction
Despite remarkable advances in surgical techniques and technology in recent decades, disparities in access to necessary surgical care have dramatically increased. Consistent with other global health care challenges, developing countries and rural regions carry the bulk of the burden. Currently, 5 billion people do not have access to safe and affordable basic surgical care, with an estimated 143 million additional surgical procedures needed annually in developing countries to provide life saving treatment and prevent disability (1). Developing effective solutions in order to meet this need are imperative to mitigate the increased mortality and morbidity that individuals requiring surgical care face in these regions. The ability to receive surgical care is dependent on two factors, the accessibility of surgical centers and the availability of qualified healthcare professionals to deliver that care. However, current models have proven to be inadequate in meeting the increasing demand for specialized surgical care. In addition to necessary investments to facilities and underlying infrastructure, innovations in surgical education may play a crucial role in ameliorating the world-wide shortage of surgeons, while diminishing gaps in knowledge, and ultimately increase access to care. One of the most promising strategies to achieve these goals derives from an advanced application of telemedicine, known as surgical telementoring.
Surgical telementoring involves the use of information technology to provide real-time guidance and technical assistance in performing surgical procedures from an expert physician in a different geographical location. Similar to traditional mentoring, it plays a dual role of educating and providing care at the same time. However, it obviates many of the logistic obstacles associated with traditional mentoring, such as distance, time constraints, and cost. Previous studies have demonstrated no difference in knowledge and skill acquisition when comparing telementoring and onsite mentoring of novice surgeons (2-4). Studies reinforce this strategy and have demonstrated its reliability, efficiency, and cost-effectiveness as an educational tool and model for mentorship (5,6). These reports suggest telementoring to be a suitable replacement to onsite mentors and particularly useful for overcoming geographic barriers to distribute surgical knowledge. In addition to its educational utility, telementoring has the potential to directly impact patient care by providing immediate access to specialized surgical expertise. Numerous reports have suggested that telementoring is a safe and feasible method of providing access to surgical expertise for patients requiring specialized procedures in areas lacking surgeons with significant experience (5-7). Some studies have even suggested that a remote surgeon may successfully guide an onsite surgeon with extremely limited experience for the procedure at hand (8). The applications of telementoring can be expanded across multiple surgical subspecialties and warrant further consideration as a strategy to increase access to surgical expertise and overcome treatment limitations related to geographic disparities.
Centers are becoming increasingly aware of the advantages of surgical telementoring and as a result, a breadth of these experiences have been published in recent years involving countries from around the world. A comprehensive review reported that as of 2010, 433 surgical procedures spanning 11 subspecialties have been documented in the literature (9). This included 12 articles incorporating intercontinental telementoring. Despite this growth, questions remain regarding ideal videoconferencing methods, resolution and latency requirements, security and liability issues, and telementoring in combination with emerging technology. This review discusses the history and progression, current applications, and future directions of surgical telementoring as a means to distribute advanced surgical expertise.
Emergence of surgical telementoring
The rise of telecommunications following the invention of the telephone in 1876 has had a great influence on medicine, allowing for communication over long distances and even leading to the development of an entire new branch of medicine, telemedicine. Telemedicine is a global term for the exchange of medical information from one location to another via telecommunication. One of the first references of telemedicine in the literature appeared in 1950 in an article that described the transmission of radiologic images a distance of 24 miles, from Westchester to Philadelphia, Pennsylvania via telephone (10). The first documented report of medical uses of video communication in the United States occurred in 1959 at the University of Nebraska where clinicians used two-way interactive television as an education tool to transmit information to students (11). This concept was then translated to the clinical setting to assist in the care of patients in remote locations in Nebraska. Throughout the following decade, applications of telemedicine continued to expand and reports of its use included psychiatric group therapy, radiotelemetry, electrocardiography (ECG) rhythm transmissions from first responders, and ship to shore and transoceanic transmission of radiographs and ECG rhythms (12-16). Also in the 1960s, the first video conference demonstration of open heart surgery was transmitted oversees via satellite (17). However, high transmission costs initially hindered proliferation and use of this technology. It was not until the late 1980s when improved technologies and lower costs began to renew interest and encourage further expansion (18).
Surgical telementoring is a more advanced telemedical application. It differs from traditional methods of telemedicine in that it accomplishes a dual role of educating and providing care at the same time. Its emergence dates back to some of the earliest reported cases using telementoring in the mid 1990s. Moore et al. assessed the feasibility of a telementoring system using a remote surgeon located in a control room (>1,000 feet from operating room) that supervised an inexperienced surgeon in 23 urologic laparoscopic procedures (2). Mentoring was accomplished with real-time video images, two-way audio communication, a robotic arm used to control the videoendoscope, and a telestrator. They reported a 95.6% procedure success rate with no statistical differences in patient outcome, complications, or operative time when compared to live instruction of the primary surgeon. Shortly after, Schulam et al. evaluated a telementoring system using a single T1 line (1.54 mega bits per second) point to point communications link that allowed a remote experienced surgeon to guide a primary laparoscopic surgeon from 3.5 miles away (19). In all cases, the primary surgeon had limited experience with the laparoscopic approach but still had the basic skills required to obtain intraperitoneal access. In total, seven cases were performed successfully without complication. In a similar study, Rosser et al. compared the outcomes of four laparoscopic colonic resections and two laparoscopic Nissen fundoplications performed by surgeons inexperienced with the laparoscopic approach (3). They reported no differences in performances of the surgeons or outcomes of the patients between those that received telementoring guidance and those with mentors in the operating room.
Early successes encouraged further research into telementoring and investigation of its ability to transmit surgical guidance across further (more ambitious) distances. Lee et al. developed a telementoring system using a PC-based unit utilizing a single high-bandwidth public telecommunication line (20). Their system involved video display from either laparoscope or an external mounted camera, two-way audio communication, telestration capabilities, ability to control the visual field by manipulation of a robotic arm holding the laparoscope, and ability to remotely operate the electrocautery device. After successfully implementing this system locally, they expanded its use to distribute surgical guidance internationally from Johns Hopkins Hospital for three cases: two in Bangkok, Thailand and one in Innsbruck, Austria. They reported no complications and an average of a 1 second transmission time delay that they contributed to the large distance and limitations in hardware and bandwidth. Another early example of international telementoring was reported by Camara and Rodriguez, who successfully telementored an endoscopic laser-assisted dacryocystorhinostomy procedure using an integrated systems digital network (ISDN) line to transmit information in real time from Honolulu, Hawaii, more than 5,000 miles to ophthalmologists at the Makati Medical Center in Manila, Philippines (21).
In addition to these early international experiences, the application of long distance surgical telementoring proved to be advantageous by the USS Abraham Lincoln, who created the Battlegroup Telemedicine (BGTM) system in order to connect the Air-Craft Carrier Battleship cruising the Pacific Ocean with locations in California and Maryland (22). The medical and surgical needs in the armed forces brings additional challenges in which telementoring has the potential to aid as a solution. The authors reported that on naval ships at the time, one surgeon may oversee the care of more than 9,000 people. Patients requiring specialized care would necessitate helicopter transport ashore, exposing them to additional risks, treatment delays, and incurring high costs. Under telementoring guidance from land-based surgeons, five laparoscopic inguinal hernia repairs were successfully completed on the USS Abraham Lincoln. The authors further stated that the BGTM system proved invaluable in obtaining timely expertise on a wide variety of surgical and medical problems that would otherwise have required a shore visit.
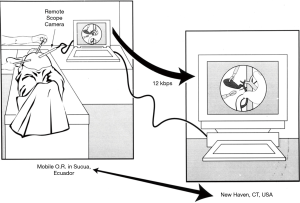
Telemedicine and telementoring continued to prove useful in aiding in the distribution of surgical care to secluded locations, even to locations lacking access to infrastructure and technology required for videoconferencing. In 1998, Rosser et al. applied telementoring to guide a laparoscopic cholecystectomy using significantly lower-bandwidth to support a mobile operating room that provided access to impoverished citizens of rural Ecuador (Figure 1) (5). Although the slow connection speed did create some “pixellation” of the distant images, the telementors were able to properly identify the cystic duct and artery and guide the operating surgeon through the procedure. Telemedicine was further applied in four other cases to conduct preoperative evaluations by surgeons who would later perform their procedures, suggesting its ability to promote maximal efficiency of health care delivery efforts.
Over the next decade, the focus of the literature regarding telementoring primarily focused on its utility to teach different procedures spanning numerous subspecialties and different geographic locations. Advances in technology and the wide availability of videoconferencing technology allowed telementoring to become cost effective and reliable. As a result, its use as a strategy to distribute surgical expertise has expanded with an increasing trend of annual publications (9). Despite variation in procedure and technology among studies, pooled analysis of manuscripts published as of 2010 demonstrated a complication rate of 4.6% further supporting the safety associated with the implementation of surgical telementoring.
Current applications
Modern technology has allowed for numerous advances in the utilization of telementoring. Early telementoring systems were limited by low transmission rates, raising concerns of the deleterious effects that a time delay may have on surgical performance (23). Current telecommunication systems allow for dramatically increased transmission speeds, permitting a considerably decreased time delay (24). In addition, the high resolution associated with modern high definition cameras has enhanced the remote surgeon’s ability to zoom and visualize small anatomic details. Interactive additions to telementoring systems such as telestration, laser pointing capabilities, or increased remote control of the visual field have played a role in enriching the teaching capabilities of the remote surgeon. Wearable technology, such as the Google Glass (Google, Mountainview, CA), and methods of augmented reality telementoring have also been implemented and have had some success (25,26). Specially designed telemedical robotic platforms such as the Karl Storz Endoscopy-America, Inc. VisitOR1 (Karl Storz; Tuttlingen, German) and RemotePresence-7 robot (InTouch Health; Santa Barbara, Calif) have been developed and may play a role in further increasing the remote surgeon’s presence in the operating room. These different strategies to perform telementoring have numerous advantages and disadvantages and will be discussed below.
Basic videoconferencing techniques
Several common, free, commercially available software applications exist that allow high-definition videoconferencing over the internet. Of these, SkypeTM (Microsoft, Redmond, WA) is the most common application that has been reported in literature. Previous studies have successfully used it as a method to connect video feeds from the operating room to a telementor in a remote location (27,28). SkypeTM and similar videoconferencing applications represent the most basic method of telementoring. Its benefits include its wide availability, easy usability, and cost-effectiveness. Limitations include its lack of interactive abilities, such as camera control or telestration, thus preventing the remote surgeon’s ability to control the visual field or draw visual aids on the video stream in order to point out anatomic structures to the on-site surgeon. Further, SkypeTM does not establish a secure peer to peer connection and lacks Health Insurance Portability and Accountability Act (HIPAA) compliance (28).
Videoconferencing applications, such as SkypeTM and FaceTime (Apple, Cupertino, CA) can be used on a variety of devices. Advances in video capturing and transmitting capabilities of portable technology, including cellular phones and tablets, have allowed physicians to have readily available potential telementoring devices at all times. Use of these devices precludes any planning or hardware and software preparation and provides physicians with the opportunity to be able to call for help and receive telementoring guidance, as needed, with the device they have on hand at any given moment. However, the literature related to the feasibility of these devices as telementoring tools is extremely limited and questions regarding their efficacy exist as they lack useful capabilities of more advanced telementoring systems. In an effort to evaluate differences between these devices and their efficacy in telementoring, Budrionis et al. conducted a randomized cross over study that streamed video of a laparoscopic procedure to a mentor surgeon through three different devices: a 15.4” laptop computer, touchscreen size 10” tablet computer, and a touchscreen size 5” smartphone (29). Twelve mentor surgeons evaluated the feasibility of these devices to telementor, ultimately showing that stationary and tablet platforms were nearly equally preferred by most of the participants as default telementoring platforms. Also, ability to perceive and identify anatomic structures was decreased on the smartphone when compared to the devices with larger screens, but this difference failed to reach statistical significance. Overall, portable tablet and smartphone technology may play a significant role in modern global telementoring due to convenience, accessibility, and low cost but further research is required in order to demonstrate their efficacy to encourage their use.
Wear-able technology
Google Glass is a wearable computer resembling conventional glasses that includes an integrated display screen, high-definition camera, microphone, bone-conduction sound transducer, and wireless connectivity. It has previously been used on rounds, and in the clinic and operating room to document a variety of conditions (30,31). Picture and video quality have been reported to be high and definitively sufficient to document relevant clinical findings (31). In an effort to assess its safety as a means to capture video to be used in a telementoring session, Hashimoto et al. surveyed 34 surgeons who blindly compared video captured with Google Glass versus an Apple iPhone 5 (Apple, Cupertino, CA) during the open cholecystectomy portion of a Whipple procedure (32). A significantly greater proportion of respondents felt that the Google Glass had poorer video quality (P<0.001) and was inadequate for telementoring as compared to the Apple iPhone 5 (82.4% vs. 26.5%, P<0.0001). However, Datta et al. used Google Glass to stream live intraoperative video from 4 hernia repairs in Paraguay and Brazil, permitting real-time observation and proctoring by mentoring surgeons in the United States and Germany (25). They reported successful image streams but noted that existing wearable technology may require further modifications to capture more difficult or complex operations. Further research is required to determine appropriate indications for using wear-able technology for surgical telementoring.
Robotic telementoring platforms
The development of specialized robotic platforms for telementoring have allowed the remote surgeon to maintain greater control of their experience in the operating room. To date, several robotic platforms have been implemented as methods of telementoring. The VisitOR1 from Karl Storz Endoscopy-America, Inc. is a telementoring robot that has been documented in the literature as an effective means of telementoring (Figure 2) (28,33). It is a Food and Drug Administration cleared Class II medical device, that connects to the remote surgeon’s laptop providing the mentoring surgeon with internal views via direct connection to endoscopic images and external views of the operation captured from built in high definition cameras. It allows the remote surgeon to control the external view camera and it provides telestration and laser pointing abilities. Additionally, it is HIPAA-compliant and has a 256-bit, military-grade encryption (33). Demonstrating another example of a telerobotic platform, Ereso et al. used a remote consultation platform consisting of a high definition pan-and-tilt camera with a custom miniature laser pointer controlled by a computer mouse (8). The authors stated benefits including its overall ease of use, surgeons’ familiarity with the use of a computer mouse, high maneuverability of the visual field, and optical zoom allowing the remote surgical subspecialist the ability to visualize anatomical structures in fine detail.

The RemotePresence-7 (RP-7) robot from InTouch Health, Inc. has also been used as a means of telementoring while additionally establishing an increased remote presence in the operating room by the remote surgeon (Figure 3) (34,35). The RP-7 allows an individual to roam, see, hear, talk, and interact with an environment from a remote location using a joystick and specially configured laptop to control robot movement and camera views. It is also equipped with infrared sensors that detect when a robot is nearing an object to prevent collisions. Agarwal et al. utilized the RP-7 as a telementoring strategy and reported that in addition to providing more conventional telementoring techniques, its small footprint and human-like dimensions, maneuverability, versatility, and ease of use, give it “a feeling of just another human being in the operating room” (35). Despite the advantages robotic platforms may provide, their limitations are primarily related to their relatively high cost which raises questions about the cost/benefit ratio of these strategies as compared to simpler telementoring methods, particularly for low and middle income countries.
Augmented reality
Augmented reality is defined as the integration of digital information with the user’s environment in real time. Augmented reality as an addition to telementoring has the added benefit of overlaying mentor guidance directly onto the trainee’s view of the operating field. Vera et al. developed and evaluated an augmented reality platform in order to assess its value in training laparoscopic skills (36). Their augmented reality platform allowed the mentor to directly provide visual guidance to the laparoscopy monitor that the student would use to visualize the operating field. They found that the students trained using the augmented reality platform had significantly faster skill acquisition as compared to students trained with traditional mentoring. Similarly, Andersen et al. developed a System for Telementoring and Augmented Reality (STAR) that provided visual instruction to a monitor that the students used to visualize their operating field in order to evaluate its effectiveness in training tasks including a port placement and abdominal incision (26). The participants using STAR had decreased errors and focus shifts but took longer to complete the tasks as compared to those with traditional mentoring. Although the data related to augmented reality and telementoring is limited to a small number of experimental studies, this early data suggests that augmented reality may provide certain benefits as a teaching aid.
Future directions
As the technology required to implement surgical telementoring is currently readily available to many physicians, the advancement of telementoring is now dependent on several other hurdles limiting its expansion. For example, licensure issues exist due to the fact that telementoring often occurs across organizational borders. Financial models have yet to be determined regarding telepresence in surgery and questions exist regarding who will pay for the associated costs. Furthermore, the distribution of liability of on-site surgeon and mentor remains unclear, and disclosure to patients is subject to scrutiny as well. The issue of patient privacy is also a significant concern for the clinical implementation of telementoring and secure HIPPA compliant transmission methods must be appropriately utilized. All of these issues need to be addressed before surgical telementoring can become a routinely used educational tool.
Additionally, despite numerous studies demonstrating the utility and safety of telementoring, the literature is limited by small sample sizes, variation in telementoring platforms, procedure, and the experience of the onsite surgeon. These limitations provide some confusion regarding the optimal use of telementoring. Future studies evaluating clinical and educational outcomes with large sample sizes that span numerous procedures may be necessary to validate its utility and appropriate indications for use. The skill set and experience of the onsite surgeon likely has a large impact on the success the telementored procedure. However, some studies have began investigating its potential to be used in “worst-case scenarios”, in which the mentored onsite healthcare professionals have very limited experience or training in the procedure they are required to perform (8,37). Future studies are needed in order to determine the feasibility of telementoring in guiding inexperienced healthcare professionals. Determining a minimum set of qualifications and skillsets is another factor that may better define the best application of telementoring and its future success.
As discussed in this review, numerous emerging technologies have been developed that may facilitate the advancement of telementoring as an educational tool. Early studies have suggested that new devices such as augmented reality, wearable technology, and telerobotic platforms may enhance the telementoring experience (25,26,35). The full utility of these approaches as well as the cost/benefit ratio have yet to be determined and need to be further investigated. The main benefit of telementoring is that it has to potential to distribute specialized surgical knowledge and guidance through a relatively convenient and low cost method as compared to traditional mentoring. In order to fit this mold, emerging technologies must maintain an appropriate cost/benefit ratio and demonstrate an educational or clinical benefits as compared to current telementoring methodologies to justify their implementation. The development of platforms that optimize patient outcomes and the educational value of telementoring, while maintaining appropriate cost-effectiveness, carry great potential to mitigate the shortage of surgeons around the world.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Int J Obstet Anesth 2016;25:75-8. [Crossref] [PubMed]
- Moore RG, Adams JB, Partin AW, et al. Telementoring of laparoscopic procedures: initial clinical experience. Surg Endosc 1996;10:107-10. [Crossref] [PubMed]
- Rosser JC, Wood M, Payne JH, et al. Telementoring. A practical option in surgical training. Surg Endosc 1997;11:852-5. [Crossref] [PubMed]
- Challacombe B, Kandaswamy R, Dasgupta P, et al. Telementoring facilitates independent hand-assisted laparoscopic living donor nephrectomy. Transplant Proc 2005;37:613-6. [Crossref] [PubMed]
- Rosser JC Jr, Bell RL, Harnett B, et al. Use of mobile low-bandwith telemedical techniques for extreme telemedicine applications. J Am Coll Surg 1999;189:397-404. [Crossref] [PubMed]
- Singh S, Sharma V, Patel P, et al. Telementoring: an Overview and Our Preliminary Experience in the Setting Up of a Cost-effective Telementoring Facility. Indian J Surg 2016;78:70-3. [Crossref] [PubMed]
- Sebajang H, Trudeau P, Dougall A, et al. Telementoring: an important enabling tool for the community surgeon. Surg Innov 2005;12:327-31. [Crossref] [PubMed]
- Ereso AQ, Garcia P, Tseng E, et al. Live transference of surgical subspecialty skills using telerobotic proctoring to remote general surgeons. J Am Coll Surg 2010;211:400-11. [Crossref] [PubMed]
- Augestad KM, Bellika JG, Budrionis A, et al. Surgical telementoring in knowledge translation--clinical outcomes and educational benefits: a comprehensive review. Surg Innov 2013;20:273-81. [Crossref] [PubMed]
- Gershon-Cohen J, Cooley AG. Telognosis. Radiology 1950;55:582-7. [Crossref] [PubMed]
- Benschoter RA, Garetz C, Smith P. The Use of Closed Circuit TV and Videotape in the Training of Social Group Workers. Social Work Education Reporter 1967;15:18-20.
- Wittson CL, Benschoter R. Two-way television: helping the Medical Center reach out. Am J Psychiatry 1972;129:624-7. [Crossref] [PubMed]
- Jutras A. Teleroentgen diagnosis by means of video-tape recording. Am J Roentgenol Radium Ther Nucl Med 1959;82:1099-102. [PubMed]
- Nagel EL, Hirschman JC, Mayer PW, et al. Telemetry of physiologic data: an aid to fire-rescue personnel in a metropolitan area. South Med J 1968;61:598-601. [Crossref] [PubMed]
- Monnier AJ, Wright IS, Lenegre J, et al. Ship-to-shore radio transmission of electrocardiograms and X-ray images. JAMA 1965;193:1060-1. [Crossref] [PubMed]
- Hirschman JC, Baker TJ, Schiff AF. Transoceanic radio transmission of electrocardiograms. Dis Chest 1967;52:186-90. [Crossref] [PubMed]
- DeBakey ME. Telemedicine has now come of age. Telemed J 1995;1:3-4. [Crossref]
- 2, Evolution and Current Applications of Telemedicine. Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine; Field MJ, editors. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington (DC): National Academies Press (US); 1996.
- Schulam PG, Docimo SG, Saleh W, et al. Telesurgical mentoring. Initial clinical experience. Surg Endosc 1997;11:1001-5. [Crossref] [PubMed]
- Lee BR, Bishoff JT, Janetschek G, et al. A novel method of surgical instruction: international telementoring. World J Urol 1998;16:367-70. [Crossref] [PubMed]
- Camara JG, Rodriguez RE. Real-time telementoring in ophthalmology. Telemed J 1998;4:375-7. [Crossref] [PubMed]
- Cubano M, Poulose BK, Talamini MA, et al. Long distance telementoring. A novel tool for laparoscopy aboard the USS Abraham Lincoln. Surg Endosc 1999;13:673-8. [Crossref] [PubMed]
- Fabrizio MD, Lee BR, Chan DY, et al. Effect of time delay on surgical performance during telesurgical manipulation. J Endourol 2000;14:133-8. [Crossref] [PubMed]
- Antoniou SA, Antoniou GA, Franzen J, et al. A comprehensive review of telementoring applications in laparoscopic general surgery. Surg Endosc 2012;26:2111-6. [Crossref] [PubMed]
- Datta N, MacQueen IT, Schroeder AD, et al. Wearable Technology for Global Surgical Teleproctoring. J Surg Educ 2015;72:1290-5. [Crossref] [PubMed]
- Andersen D, Popescu V, Cabrera ME, et al. Medical telementoring using an augmented reality transparent display. Surgery 2016;159:1646-53. [Crossref] [PubMed]
- Miller JA, Kwon DS, Dkeidek A, et al. Safe introduction of a new surgical technique: remote telementoring for posterior retroperitoneoscopic adrenalectomy. ANZ J Surg 2012;82:813-6. [Crossref] [PubMed]
- Ponsky TA, Bobanga ID, Schwachter M, et al. Transcontinental telementoring with pediatric surgeons: proof of concept and technical considerations. J Laparoendosc Adv Surg Tech A 2014;24:892-6. [Crossref] [PubMed]
- Budrionis A, Hartvigsen G, Lindsetmo RO, et al. What device should be used for telementoring? Randomized controlled trial. Int J Med Inform 2015;84:715-23. [Crossref] [PubMed]
- Mitrasinovic S, Camacho E, Trivedi N, et al. Clinical and surgical applications of smart glasses. Technol Health Care 2015;23:381-401. [Crossref] [PubMed]
- Muensterer OJ, Lacher M, Zoeller C, et al. Google Glass in pediatric surgery: an exploratory study. Int J Surg 2014;12:281-9. [Crossref] [PubMed]
- Hashimoto DA, Phitayakorn R, Fernandez-del Castillo C, et al. A blinded assessment of video quality in wearable technology for telementoring in open surgery: the Google Glass experience. Surg Endosc 2016;30:372-8. [Crossref] [PubMed]
- Ponsky TA, Schwachter M, Parry J, et al. Telementoring: the surgical tool of the future. Eur J Pediatr Surg 2014;24:287-94. [Crossref] [PubMed]
- Rothenberg SS, Yoder S, Kay S, et al. Initial experience with surgical telementoring in pediatric laparoscopic surgery using remote presence technology. J Laparoendosc Adv Surg Tech A 2009;19 Suppl 1:S219-22. [Crossref] [PubMed]
- Agarwal R, Levinson AW, Allaf M, et al. The RoboConsultant: telementoring and remote presence in the operating room during minimally invasive urologic surgeries using a novel mobile robotic interface. Urology 2007;70:970-4. [Crossref] [PubMed]
- Vera AM, Russo M, Mohsin A, et al. Augmented reality telementoring (ART) platform: a randomized controlled trial to assess the efficacy of a new surgical education technology. Surg Endosc 2014;28:3467-72. [Crossref] [PubMed]
- Kirkpatrick AW, Tien H, LaPorta AT, et al. The marriage of surgical simulation and telementoring for damage-control surgical training of operational first responders: A pilot study. J Trauma Acute Care Surg 2015;79:741-7. [Crossref] [PubMed]



