
Efficacy of Yun-type pelvic floor optimal training therapy and PFMT on middle aged women with mild to moderate overactive bladder: a randomized controlled trial
Introduction
Overactive bladder (OAB) is a symptom syndrome of urinary urgency, and presents as urinary frequency and nocturia without infection or other pathological features, irrespective of urgency incontinence status (1,2). Nowadays, the prevalence of OAB ranges from 12–22% in Europe and 16–17% in the USA, and can vary by age, survey methodology, and diagnosis definition (3-5). Although the prevalence of OAB is similar in men and women, the prevalence of various symptoms within the OAB complex in men and women differ, owing to anatomical and physiological differences in the lower urinary tract (6,7). The symptoms of OAB are highly bothersome to patients and have an adverse impact on sleep, mental health, work productivity, and quality of life (8-10). At present, the first-line treatment approach for OAB is conservative, as recommended by the International Continence Society and the American Urology Association. The strategies of the conservative approach for OAB patients are determined by individual necessities and symptom characteristics in clinical practice (11,12). Pelvic floor muscle training (PFMT), through voluntary contraction of the muscles to shut the urethra and thereby raise urethral pressure, can inhibit the urinary reflex, control urgency, and prevent the loss of urine during detrusor contraction (13). However, PFMT can be boring and monotonous, which can cause poor compliance and modest improvement of OAB symptoms (14). Therefore, it is of great significance to establish a new safe and effective training method for functional reconstruction of pelvic floor for patients with OAB. To find a safe, effective, low follow-up rate and well tolerated new training of crotch and pelvic floor function reconstruction has become a new direction of our professional exploration. This study integrates professional and scientific pelvic floor muscle training into dance and aerobics. This method is optimized and supplemented on the basis of Yun-type training with completely independent intellectual property rights (Huzuo-2016-A-00627419), which has been mature applied in clinical practice. In this randomized, crossover trial, we reported the treatment effectiveness of Yun-type training versus PFMT for middle-aged women with mild to moderate OAB. We present the following article in accordance with the CONSORT reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3357/rc).
Methods
Trial design and oversight
This study was a randomized, crossover, single-center clinical trial. Patients at Shanghai Fifth People’s Hospital of Fudan University were included and randomization was performed for group assignment. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocol of this study was approved by the ethics committee of Shanghai Fifth People’s Hospital of Fudan University [No. (2018)Lunshen174]. Signed informed consent forms were obtained from all included patients.
Trial population
A total of 150 middle-aged women with mild to moderate OAB from Shanghai Fifth People’s Hospital of Fudan University were included in this study. Patients were included if they met the following inclusion criteria: (I) married women aged 30–45 years, irrespective of fertility status; (II) urination diary could be completed for 3 days, irrespective of urge urinary incontinence status, the number of urinations ≥8 times within 24 hours, ≥2 times in a night, and the volume of urination <200 mL/time; (III) the overactive symptom bladder scores (OABSS) ranged from 3–11, and the score of urgency of urination ≥2; (IV) female sexual function index (FSFI) <25; (V) fixed partner; (VI) sex partners did not have male sexual dysfunction; (VII) the duration of disease >3 months; and (VIII) patients did not receive drugs within 3 months. The exclusion criteria of this study were as follows: (I) asexual experience, gynecological inflammation, at lactation or menopause, presence of tumor, and endocrine disease, pelvic floor organ prolapse; (II) stress urinary incontinence or stress urinary incontinence dominant mixed urinary incontinence; (III) urinary infection or chronic inflammation; (IV) history of transurethral and pelvic surgery; (V) patients with diabetes, severe constipation, and dyspepsia; (VI) post-voiding residual (PVR) >50 mL; (VII) The patient has used M3 blockers or other OAB drugs; (VIII) patients could not adhere to Yun-type training or PFMT, and the follow-up data were unavailable.
Randomization and study agents
Eligible patients were randomly assigned to treatment with Yun-type training or PFMT. Randomization was carried out through a central computerized system using a random number table. This study was designed as a randomized, crossover clinical trial. The intervention group was first given Yun-type training for 6 weeks, then switched to PFMT for 6 weeks after 2 weeks of elution. Patients in the control group were first treated with PFMT for 6 weeks, and changed to the use of Yun-type training for 6 weeks after 2 weeks of elution. Details regarding the Yun-type training are as follows: A 488 double metal waist chain weighing 0.8+0.1 kg is worn on the waist and hips. The class includes a 15-minute crotch warm-up. Do it for 25 minutes in a state of contracting the anus and vagina (the time and rhythm of contracting the anus and vagina is performed according to the order of the head coach). For the last 15 minutes, pelvic floor muscle strengthening and body relaxation exercises are performed with soothing music and legs slightly apart. Slow frequency (30 seconds of anal and vaginal contractions, 10 seconds of relaxation on exhalation) and fast frequency (2 seconds of anal and vaginal contractions, and relaxation on exhalation) separated by 45 reps per session.
Data collection and endpoints
The outcomes were collected and analyzed in a blinded manner by investigators. The following items were collected before treatment, after 6 weeks, and after 14 weeks of interventions: OABSS, urine in daytime, nocturia, urgency, urge urinary incontinence, patient's perception of bladder condition (PPBC), voiding volume (VV), urogenital distress inventory-6 (UDI-6), average flow rate (Qave), maximum flow rate (Qmax), PVR, incontinence impact questionnaire-7 (IIQ-7), C-reactive protein (CRP), FSFI, sexual desire, arousal, damp, climax, pain, satisfaction, pelvic floor muscle tone, type I muscle strength, type II muscle strength, and sex partner satisfaction.
Statistical analysis
Firstly, the normality and homogeneity of variance of the collected data were assessed. Subsequently, the mean and standard deviation were applied to describe data which met the normal distribution, otherwise, the median (interquartile range) was employed. Categorical data are presented as number of events and proportion. The characteristics between the intervention and control groups were assessed by using the t test or rank sum test according to the data distribution. Then, repeated measures analysis of variance (ANOVA) was applied to analyze the changes in investigated indexes between the intervention and control groups at different observation times after applying age and BMI as covariables. All reported inspection levels were 2-sided, and a P value of <0.05 was considered as statistically significant. The IBM Statistical Package for the Social Sciences (SPSS) software for Windows version 19.0 was applied to conduct all analyses in this study.
Results
Patients
In the period from December 2018 to July 2020, a total of 150 middle-aged women with mild to moderate OAB underwent randomization to Yun-type training (n=83) or PFMT (n=67) (Figure 1). Table 1 summarizes the baseline characteristics of the included patients, and most variables were well matched between groups. We noted that BMI (P<0.001), PPBC (P=0.048), damp level (P<0.001), and sex partner satisfaction (P=0.012) showed significant differences between the intervention and control groups. However, there were no significant differences between groups in terms of age, OABSS, urine, nocturia, urgency, UUI, UDI-6, IIQ-7, VV, Qave, Qmax, PVR, CRP, FSFI, sexual desire, arousal, climax, pain, satisfaction, type I muscle strength, type II muscle strength, and pelvic floor muscle tone.
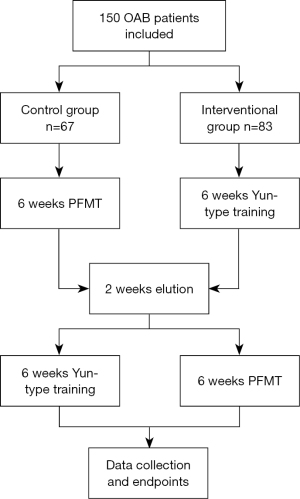
Table 1
| Variable | Control (n=67) | Intervention (n=83) | P value |
|---|---|---|---|
| Age (years) | 37.00 (33.00, 42.00) | 37.00 (32.00, 42.00) | 0.914 |
| BMI (kg/m2) | 38.00 (34.00, 42.00) | 30.20 (29.10, 31.90) | <0.001 |
| OABSS | 6.00 (4.00, 8.00) | 5.00 (4.00, 7.00) | 0.627 |
| Urine in daytime | 0.882 | ||
| 0 | 24 (35.82) | 27 (32.53) | |
| 1 | 32 (47.76) | 43 (51.81) | |
| 2 | 11 (16.42) | 13 (15.66) | |
| Nocturia | 0.615 | ||
| 0 | 9 (13.43) | 13 (15.66) | |
| 1 | 29 (43.28) | 38 (45.78) | |
| 2 | 23 (34.33) | 21 (25.30) | |
| 3 | 6 (8.96) | 11 (13.25) | |
| Urgency | 0.420 | ||
| 2 | 31 (46.27) | 49 (59.04) | |
| 3 | 23 (34.33) | 21 (25.30) | |
| 4 | 12 (17.91) | 11 (13.25) | |
| 5 | 1 (1.49) | 2 (2.41) | |
| UUI | 0.411 | ||
| 0 | 20 (29.85) | 19 (22.89) | |
| 1 | 22 (32.84) | 37 (44.58) | |
| 2 | 18 (26.87) | 22 (26.51) | |
| 3 | 7 (10.45) | 5 (6.02) | |
| PPBC | 0.048 | ||
| 2 | 0 (0.00) | 8 (9.64) | |
| 3 | 12 (17.91) | 15 (18.07) | |
| 4 | 30 (44.78) | 27 (32.53) | |
| 5 | 25 (37.31) | 33 (39.76) | |
| IIQ-7 | 50.00 (45.00, 60.00) | 55.00 (45.00, 60.00) | 0.834 |
| UDI-6 | 40.00 (35.00, 50.00) | 35.00 (30.00, 50.00) | 0.124 |
| Qave | 10.00 (9.00, 10.00) | 10.00 (8.00, 12.00) | 0.913 |
| Qmax | 20.00 (17.00, 21.00) | 21.00 (18.00, 23.00) | 0.054 |
| VV | 215.00 (200.00, 225.00) | 210.00 (180.00, 250.00) | 0.646 |
| PVR | 14.00 (8.00, 20.00) | 12.00 (8.00, 20.00) | 0.698 |
| CRP | 2.10 (1.80, 3.60) | 3.00 (1.40, 4.10) | 0.875 |
| FSFI | 23.00 (21.40, 24.20) | 22.00 (20.20, 23.40) | 0.061 |
| Sexual desire | 3.60 (3.60, 4.20) | 4.00 (2.80, 4.00) | 0.106 |
| Arousal | 4.20 (3.60, 4.20) | 3.80 (3.20, 4.40) | 0.332 |
| Damp | 3.60 (3.00, 4.20) | 3.00 (2.40, 4.00) | <0.001 |
| Pain | 4.00 (3.60, 4.40) | 4.00 (3.60, 4.40) | 0.798 |
| Climax | 3.60 (2.80, 3.60) | 3.20 (2.80, 3.60) | 0.881 |
| Satisfaction | 3.80 (3.60, 4.40) | 4.20 (3.40, 4.20) | 0.490 |
| Type I muscle strength | 20.80 (19.10, 22.40) | 20.90 (18.20, 24.30) | 0.654 |
| Type II muscle strength | 25.30 (24.10, 26.50) | 25.50 (23.20, 28.10) | 0.391 |
| Pelvic floor muscle tone | 9.70 (8.00, 10.60) | 8.90 (7.10, 11.40) | 0.578 |
| Sex partner satisfaction | 4.00 (3.00, 6.00) | 3.00 (3.00, 4.00) | 0.012 |
Data are shown as n (%) or median (interquartile range). OABSS, overactive bladder symptoms; UUI, urge urinary incontinence; VV, voiding volume; UDI-6, urogenital distress inventory-6; PPBC, patient’s perception of bladder condition; IIQ-7, incontinence impact questionnaire-7; Qave, average flow rate; CRP, C-reactive protein; Qmax, maximum flow rate; PVR, postvoid residual urine volume; FSFI, female sexual function index.
Investigated outcomes
In Table 2, patients in the intervention group showed significant improvements in OABSS (P<31 0.001), urine (P<0.001), nocturia (P<0.001), urgency (P<0.001), UUI (P<0.001), PPBC (P<0.001), UDI-6 (P<0.001), IIQ-7 (P<0.001), VV (P<0.001), Qmax (P < 0.001), FSFI (P<0.001), sexual desire (P<0.001), arousal (P<0.001), climax (P<0.001), pain (P=0.017), satisfaction (P<0.001), type I muscle strength (P<0.001), type II muscle strength (P<0.001), pelvic floor muscle tone (P<0.001), and sex partner satisfaction (P<0.001) after 6 weeks follow-up compared with those in the control group. After 2 weeks of elution, we noted that Yun-type training resulted in significant improvements in OABSS (P<0.001), urine (P<0.001), urgency (P<0.001), UUI (P<0.001), PPBC (P<0.001), UDI-6 (P<0.001), IIQ-7 (P<0.001), VV (P<0.001), Qave (P=0.003), FSFI (P<0.001), sexual desire (P<0.001), arousal (P<0.001), pain (P<0.001), satisfaction (P<0.001), type I muscle strength (P<0.001), type II muscle strength (P<0.001), pelvic floor muscle tone (P<0.001), and sex partner satisfaction (P<0.001) after 14 weeks follow-up compared with the PFMT group. However, there were no significant differences between Yun-type training and PFMT in terms of the levels of PVR, CRP, and damp.
Table 2
| Variables | Groups | Baseline | 6 weeks | 14 weeks | P value | ||
|---|---|---|---|---|---|---|---|
| Time | Group | Time × group | |||||
| OABSS | Control | 6.12 (2.64) | 4.49 (2.22) | 1.87 (1.38) | 0.815 | 0.469 | <0.001 |
| Intervention | 5.95 (2.52) | 2.13 (1.49) | 4.18 (1.62) | ||||
| P value | 0.693 | <0.001 | <0.001 | ||||
| Urine | Control | 0.81 (0.70) | 0.67 (0.56) | 0.18 (0.39) | 0.699 | 0.425 | <0.001 |
| Intervention | 0.83 (0.68) | 0.36 (0.48) | 0.77 (0.61) | ||||
| P value | 0.823 | <0.001 | <0.001 | ||||
| Nocturia | Control | 1.39 (0.83) | 1.36 (0.81) | 0.79 (0.59) | 0.984 | 0.177 | <0.001 |
| Intervention | 1.36 (0.90) | 0.61 (0.64) | 0.82 (0.57) | ||||
| P value | 0.853 | <0.001 | 0.766 | ||||
| Urgency | Control | 2.75 (0.80) | 1.70 (0.67) | 0.69 (0.58) | 0.641 | 0.248 | <0.001 |
| Intervention | 2.59 (0.81) | 0.86 (0.84) | 1.78 (0.72) | ||||
| P value | 0.242 | <0.001 | <0.001 | ||||
| UUI | Control | 1.18 (0.98) | 0.76 (0.76) | 0.21 (0.41) | 0.788 | 0.107 | <0.001 |
| Intervention | 1.16 (0.85) | 0.30 (0.49) | 0.81 (0.71) | ||||
| P value | 0.881 | <0.001 | <0.001 | ||||
| PPBC | Control | 4.19 (0.72) | 3.19 (0.74) | 1.79 (0.75) | 0.125 | 0.846 | <0.001 |
| Intervention | 4.02 (0.99) | 2.10 (0.55) | 3.08 (0.57) | ||||
| P value | 0.241 | <0.001 | <0.001 | ||||
| UDI-6 | Control | 41.19 (8.79) | 26.37 (10.35) | 14.45 (7.95) | 0.236 | 0.153 | <0.001 |
| Intervention | 39.17 (9.38) | 16.51 (7.99) | 20.51 (7.99) | ||||
| P value | 0.179 | <0.001 | <0.001 | ||||
| IIQ-7 | Control | 52.13 (9.41) | 37.13 (9.41) | 17.51 (8.75) | <0.001 | 0.936 | <0.001 |
| Intervention | 52.90 (10.90) | 17.90 (10.90) | 32.90 (10.90) | ||||
| P value | 0.649 | <0.001 | <0.001 | ||||
| VV | Control | 214.25 (23.36) | 223.51 (22.98) | 276.49 (33.97) | 0.644 | 0.663 | <0.001 |
| Intervention | 213.19 (41.65) | 275.90 (37.60) | 235.90 (37.60) | ||||
| P value | 0.853 | <0.001 | <0.001 | ||||
| Qave | Control | 9.82 (1.36) | 10.54 (1.76) | 11.24 (1.97) | 0.525 | 0.284 | 0.056 |
| Intervention | 10.13 (2.18) | 10.43 (2.51) | 10.17 (2.32) | ||||
| P value | 0.309 | 0.776 | 0.003 | ||||
| Qmax | Control | 19.78 (2.88) | 21.43 (3.88) | 21.60 (3.16) | 0.203 | <0.001 | <0.001 |
| Intervention | 20.36 (3.63) | 26.57 (2.87) | 25.57 (2.82) | ||||
| P value | 0.284 | <0.001 | <0.001 | ||||
| PVR | Control | 14.43 (8.71) | 14.81 (7.50) | 14.79 (7.62) | 0.54 | 0.297 | 0.397 |
| Intervention | 14.00 (8.19) | 13.78 (6.38) | 15.46 (6.32) | ||||
| P value | 0.755 | 0.368 | 0.559 | ||||
| CRP | Control | 2.77 (1.53) | 2.68 (1.45) | 2.72 (1.34) | 0.544 | 0.67 | 0.404 |
| Intervention | 2.79 (1.52) | 2.80 (1.51) | 2.82 (2.28) | ||||
| P value | 0.938 | 0.624 | 0.749 | ||||
| FSFI | Control | 22.56 (1.85) | 25.27 (1.85) | 29.38 (1.49) | <0.001 | 0.007 | <0.001 |
| Intervention | 21.88 (2.33) | 28.24 (2.34) | 24.89 (2.27) | ||||
| P value | 0.053 | <0.001 | <0.001 | ||||
| Sexual desire | Control | 3.75 (0.44) | 4.37 (0.79) | 5.43 (0.45) | 0.042 | <0.001 | <0.001 |
| Intervention | 3.56 (0.80) | 5.36 (0.72) | 3.20 (0.82) | ||||
| P value | 0.087 | <0.001 | <0.001 | ||||
| Arousal | Control | 3.87 (0.62) | 4.54 (0.62) | 5.57 (0.67) | <0.001 | 0.179 | <0.001 |
| Intervention | 3.81 (0.98) | 5.27 (0.87) | 4.86 (0.87) | ||||
| P value | 0.625 | <0.001 | <0.001 | ||||
| Damp | Control | 3.70 (0.62) | 4.01 (0.71) | 3.97 (0.68) | 0.246 | 0.017 | 0.164 |
| Intervention | 3.28 (0.75) | 3.87 (0.70) | 3.77 (0.66) | ||||
| P value | <0.001 | 0.205 | 0.071 | ||||
| Climax | Control | 3.35 (0.58) | 3.69 (0.53) | 4.23 (0.60) | 0.557 | 0.107 | <0.001 |
| Intervention | 3.24 (0.56) | 4.22 (0.65) | 4.13 (0.58) | ||||
| P value | 0.258 | <0.001 | 0.299 | ||||
| Pain | Control | 3.97 (0.57) | 4.16 (0.53) | 4.72 (0.63) | 0.327 | 0.14 | <0.001 |
| Intervention | 4.02 (0.45) | 4.35 (0.42) | 4.26 (0.46) | ||||
| P value | 0.559 | 0.017 | <0.001 | ||||
| Satisfaction | Control | 3.92 (0.65) | 4.49 (0.50) | 5.46 (0.31) | 0.244 | 0.798 | <0.001 |
| Intervention | 3.98 (0.53) | 5.16 (0.39) | 4.67 (0.38) | ||||
| P value | 0.557 | <0.001 | <0.001 | ||||
| Type I muscle strength | Control | 20.84 (1.93) | 23.07 (1.81) | 31.91 (1.85) | <0.001 | 0.047 | <0.001 |
| Intervention | 21.38 (3.40) | 29.30 (3.13) | 23.48 (3.40) | ||||
| P value | 0.248 | <0.001 | <0.001 | ||||
| Type II muscle strength | Control | 25.28 (1.80) | 28.94 (1.78) | 37.04 (1.76) | <0.001 | 0.834 | <0.001 |
| Intervention | 25.70 (3.41) | 34.57 (3.22) | 29.60 (3.41) | ||||
| P value | 0.367 | <0.001 | <0.001 | ||||
| Pelvic floor muscle tone | Control | 9.40 (2.14) | 6.68 (1.82) | 4.16 (1.56) | <0.001 | 0.751 | <0.001 |
| Intervention | 9.10 (2.38) | 4.75 (1.39) | 6.42 (2.10) | ||||
| P value | 0.418 | <0.001 | <0.001 | ||||
| Sex partner satisfaction | Control | 4.07 (1.68) | 5.72 (1.71) | 7.46 (1.02) | 0.086 | 0.011 | <0.001 |
| Intervention | 3.24 (0.92) | 7.10 (0.95) | 5.76 (1.63) | ||||
| P value | <0.001 | <0.001 | <0.001 | ||||
Data are shown as mean (SD). OABSS, overactive bladder symptoms; UUI, urge urinary incontinence; VV, voiding volume; PPBC, patient’s perception of bladder condition; IIQ-7, incontinence impact questionnaire-7; UDI-6, urogenital distress inventory-6; Qave, average flow rate; CRP, C-reactive protein; Qmax, maximum flow rate; PVR, postvoid residual urine volume; FSFI, female sexual function index.
Discussion
Currently, PFMT is already regarded as the first choice for the prevention and treatment of OAB by the International Urine Control Association, while patient compliance is relatively poor owing to the boring and monotonous nature of PFMT. On the basis of original PFMT, the current study compared the effectiveness of Yun-type training with PFMT on OAB symptoms, sexual function, and sex partner satisfaction for middle-aged women with mild to moderate OAB. This study found that Yun-type training was significantly associated with improvements in OABSS, urine, urgency, UUI, PPBC, UDI-6, IIQ-7, VV, FSFI, sexual desire, arousal, pain, satisfaction, pelvic floor muscle tone, type I muscle strength, type II muscle strength, and sex partner satisfaction compared with PFMT. Moreover, Yun-type training could significantly improve nocturia, Qmax, and climax for middle-aged women with mild to moderate OAB. PFMT could inhibit the training of the pelvic floor reflex and cause detrusor contraction (13). PFMT has already proven to be a better intervention strategy for OAB management, while the effectiveness of PFMT can be affected by patience, empirical guidance, and the maintenance of patient compliance. The duration of follow-up in our study was relatively short, and the compliance of patients was better than expected, while patient compliance may be affected by long-term treatment. A prior study conducted by Cochrane found that PFMT could yield beneficial effects for urinary incontinence, which could be explained by the fact that PFMT could inhibit pathological detrusor contraction by interfering with the urethral/detrusor reflex and increase pelvic floor muscle strength for better impulse control (15,16).
Although the mechanism for the effect of PFMT on OAB symptoms is unclear, we speculate that frequent urination is caused by a lack of training and decreased bladder compliance, which could be corrected by progressively increasing the interval between urinations, resulting in increased urine output and bladder functional capacity. Retraining these patients to fail within normal intervals will restore compliance as volume increases and may contribute to improved symptoms (17-19). A study conducted by Jarvis et al. found that PFMT was superior to drug therapy management for detrusor instability (20). However, the superior effects of PFMT over drug therapies gradually disappeared after 6 months (21). Therefore, the training regimen should not only require the patient to contract and relax the pelvic floor muscles for a certain period but should also set specific goals for the duration of contractions, and instructions should be applied to increase the intervals.
The results of this study showed that compared with traditional PFMT, Yun-type training could improve OAB symptoms, FSFI, and sex partner satisfaction. Yun-type training combines more fashionable elements and improves the boredom of simple PFMT through the combination of waist, abdomen, hip, and leg training. The hip training in Yun-type training can cause the contraction of pelvic floor muscles and inhibit the overactivity of the detrusor muscle. The contraction of the pelvic floor muscle group and urethral external sphincter can adjust the urethral internal sphincter. Crotch training in Yun-type training can improve FSFI and spousal satisfaction by improving crotch flexibility and vaginal control. The rhythm of the sound emitted by the waist chain during implementation of Yun-type training and the dancing can echo each other, then the training intensity can also be enhanced by the effect of gravity of the waist chain. Therefore, we speculate that the superior sexual function resulting from Yun-type training can be explained by the fact that it can contract deep and superficial muscle layers, resulting in increased vaginal wall pressure and blood flow, which further improves FSFI and sex partner satisfaction.
The study has several limitations. Firstly, the current study was a single-center study, and the results of this study should be cautiously recommended. Secondly, the characteristics of patients only included age and BMI, while medical history and background exercise regimens were not recorded, which could introduce potential biases and impact the treatment effects between Yun-type training and PFMT. Thirdly, stratified analyses according to patient characteristics for investigated outcomes were not conducted. Additionally, this analysis were based on the short-term intervention study of OAB treatment, and the long-term effects between Yun-type training and PFMT should be observed for middle-aged women with mild to moderate OAB.
The current study found that the use of Yun-type training could yield beneficial effects on OAB symptoms, sexual function, and sex partner satisfaction for middle-aged women with mild to moderate OAB. These results should be verified by further large-scale randomized controlled trials, and the long-term effects of Yun-type training on various stages of OAB should be evaluated.
Acknowledgments
Funding: The study was funded by the Shanghai Key Medical Specialty Program (Grant No. ZK2019A03).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3357/rc
Trial Protocol: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3357/tp
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-3357/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-3357/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocol of this study was approved by the ethics committee of Shanghai Fifth People’s Hospital of Fudan University [No. (2018)Lunshen174]. Signed informed consent forms were obtained from all included patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003;61:37-49. [Crossref] [PubMed]
- Turell W, Howson A, MacDiarmid SA, et al. Taking OAB seriously: A qualitative evaluation of primary care education on overactive bladder syndrome management. Int J Clin Pract 2020;74:e13604. [Crossref] [PubMed]
- Lee WL, Chang CP, Wang PH. Overactive bladder syndrome in nulliparous women. J Chin Med Assoc 2021;84:809-10. [Crossref] [PubMed]
- Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006;50:1306-14; discussion 1314-5. [Crossref] [PubMed]
- Mckellar K, Bellin E, Schoenbaum E, et al. Prevalence, risk factors, and treatment for overactive bladder in a racially diverse population. Urology 2019;126:70-5. [Crossref] [PubMed]
- Araklitis G, Baines G, da Silva AS, et al. Recent advances in managing overactive bladder. F1000Res 2020 Sep 11;9:F1000 Faculty Rev-1125.
- Peyronnet B, Mironska E, Chapple C, et al. A Comprehensive Review of Overactive Bladder Pathophysiology: On the Way to Tailored Treatment. Eur Urol 2019;75:988-1000. [Crossref] [PubMed]
- Hutchinson A, Nesbitt A, Joshi A, et al. Overactive bladder syndrome: Management and treatment options. Aust J Gen Pract 2020;49:593-8. [Crossref] [PubMed]
- Huang TX, Lo TS, Tseng HJ, et al. Correlation between overactive bladder and detrusor overactivity: a retrospective study. Int Urogynecol J 2022; Epub ahead of print. [Crossref] [PubMed]
- Michel MC. Where will the next generation of medical treatments for overactive bladder syndrome come from? Int J Urol 2020;27:289-94. [Crossref] [PubMed]
- Lin XD, Lin N, Ke ZB, et al. Effects of overactive bladder syndrome on female sexual function. Medicine (Baltimore) 2021;100:e25761. [Crossref] [PubMed]
- Wang Y, Shi C, Wang Y, et al. The Correlation between Severity of Overactive Bladder Symptoms with Female Sexual Dysfunction and Sexual Satisfaction of Partners. Urol Int 2021;105:124-30. [Crossref] [PubMed]
- Shawer S, Khunda A, Waring GJ, et al. Impact of intravesical onabotulinumtoxinA (Botox) on sexual function in patients with overactive bladder syndrome: a systematic review and meta-analysis. Int Urogynecol J 2022;33:235-43. [Crossref] [PubMed]
- Gross J, Vetter JM, Lai HH. Clustering of patients with overactive bladder syndrome. BMC Urol 2021;21:41. [Crossref] [PubMed]
- Deeks ED. Mirabegron: A Review in Overactive Bladder Syndrome. Drugs 2018;78:833-844. [Crossref] [PubMed]
- Bykoviene L, Kubilius R, Aniuliene R, et al. Pelvic Floor Muscle Training With Or Without Tibial Nerve Stimulation and Lifestyle Changes Have Comparable Effects on The Overactive Bladder. A Randomized Clinical Trial. Urol J 2018;15:186-92. [PubMed]
- Phé V, Gamé X. Non-neurogenic overactive bladder. Prog Urol 2020;30:865. [PubMed]
- Hsiao SM, Wu PC, Chang TC, et al. Urodynamic and Bladder Diary Factors Predict Overactive Bladder-wet in Women: A Comparison With Overactive Bladder-dry. Int Neurourol J 2019;23:69-74. [Crossref] [PubMed]
- Burgio KL, Locher JL, Goode PS, et al. Behavioral vs drug treatment for urge urinary incontinence in older women: a randomized controlled trial. JAMA 1998;280:1995-2000. [Crossref] [PubMed]
- Jarvis GJ. A controlled trial of bladder drill and drug therapy in the management of detrusor instability. Br J Urol 1981;53:565-6. [Crossref] [PubMed]
- Athanasiou S, Pitsouni E, Grigoriadis T, et al. Mirabegron in female patients with overactive bladder syndrome: What's new? A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 2020;251:73-82. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)


