A novel clinical dynamic stereopsis assessment based on autostereoscopic display system
Introduction
Stereopsis is the perceptual ability to accurately judge the three-dimensional (3D) spatial positions of objects. It relies on precise coordination of the visual pathway, including binocular stimulus, fusion function, and visual perception by brain neural networks (1). A reduced level of stereopsis negatively impacts an individual’s ability to complete daily tasks (2). Therefore, stereopsis assessment plays an integral role in the ophthalmic examination. Furthermore, it is important to assess stereo acuity both statically and dynamically (3,4).
Clinical stereopsis testing involves 2 methods. One method uses static stimuli with a given static parallax (a depth cue that can be perceived by binoculars); the other uses dynamic stimuli, which include the movement or depth change of an object. Deficient performance in the observation of depth and motion could represent an impairment in stereopsis (5). A classical dynamic stereopsis program was generated by random-dot stereograms and kinematographs (6). In our previous study, this computer-programmed software for random-dot stereopsis measurements was displayed on a 13.3-inch color monitor with a 1.6-GHz dual-core Intel Core i5, 256 GB (MacBook Air®; Apple, Cupertino, CA, USA) using JAVA programming language (7). Stereopsis can also be assessed by measuring the depth change rate function in response to dynamic random-dot stimuli (8). In 2015, Allen et al. (9) developed a novel approach in which the investigators tested stereopsis by the change detection based on parallax and the interocular velocity difference. Although methods to assess dynamic stereopsis have been constantly updated, instruments typically require glasses (red-blue or polarized) to allow binocular viewing of separate colored or polarized images, which could generate uncomfortable and unnatural visual experiences for the patient (10,11). Furthermore, the accuracy of stereopsis examination is influenced by several instrumental parameters such as luminance, crosstalk, and spectrum (12,13). Improving the testing instruments’ hardware is one way to optimize stereoscopic measurements.
In recent years, near-eye 3D displays have experienced rapid growth and shown great promise in a variety of applications, such as entertainment, education, and health care (14). Presenting separate images with parallax in front of the viewer’s eyes without additional auxiliary equipment is the classical principle of computer stereoscopy (10). In our previous studies, we developed an interactive, autostereoscopic screening tool based on a directional backlight technology and evaluated its feasibility for visual function assessments (15). In this study, we combined the autostereoscopic display system based on directional backlight technology and dynamic stereopsis assessment. The research hypothesis was that the autostereoscopic display system can better display dynamic clues for clinical dynamic stereopsis assessment and has the accuracy equivalent to the conventional dynamic random-dot stereopsis measuring instrument. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-21-6700/rc).
Methods
The autostereoscopic dynamic stereopsis assessment device
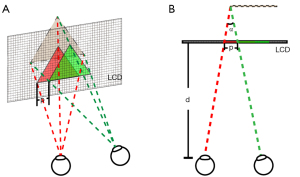
The autostereoscopic dynamic stereopsis assessment device was based on the directional backlight technology, which presented the left or right eye parallax image in separate periods on a liquid crystal display (LCD) (16,17). This 24-inch LCD panel had a resolution of 1,920*1,080 pixels and a refresh rate of 120 Hz. Since human eyes cannot distinguish intervals less than 30 Hz, both the left and right eyes could view different images at the same time with this device, and a stereo viewing effect was formed in the brain (Figure 1A).

There are three patterns in this autostereoscopic dynamic stereopsis assessment device including motion-only, depth-only, and motion-depth. The test picture consisted of black (0, 0, 0) dots and white (255, 255, 255) dots (red-green-blue relative intensity format). The test target of each pattern was a block composed of 60×50 pixels with a movement speed of 10 fps (frames per second), therefore each eye saw a change in location every 1/10 of a second.
In addition, an intelligent eye-tracking camera in the device tracked human eyes to provide an accurate directional projection of light (Figure 1B) (18,19). Mobile phones were connected via Bluetooth or wirelessly and used as the operating terminal for participants to complete the tests.
Dynamic stereopsis stimulus and assessment task
Slightly different left and right images presented by LCD could cause binocular parallax, which generated the effect of stereopsis. The parallax calculation formula was as follows:
where p was the parallax, n was the pixel difference between the 2 eyes images, L was the width of the display screen, and q was the horizontal pixels of the display screen (Figure 2A). The dynamic stereo acuity calculation formula was as follows:
where α was the dynamic stereo acuity and d was the viewing distance between the participant and the screen (Figure 2B). This novel autostereoscopic dynamic stereopsis assessment device could present 4 dynamic stereo acuity levels at 170", 340", 510", and 680".
Theoretically, at least 2 possible methods of generating dynamic stereopsis were available: one mechanism that detected binocular disparity at different times (depth only) and another one that detected interocular velocity differences (motion only) (20). Therefore, 3 patterns were involved in our novel autostereoscopic dynamic stereopsis assessment device: motion-only, depth-only, and motion-depth, from which the depth and motion cues could be included or omitted independently.
Motion-only pattern: the 4 blocks had an equal depth, in which 3 blocks performed the same horizontal displacement movement, while the fourth box performed a Z-shaped movement (Figure 3A).

Depth-only pattern: the 4 blocks executed the same Z-shaped movement, where 3 blocks had the same depth, while the fourth seemed further (Figure 3B).
Motion-depth pattern: the 3 blocks with the same depth executed the same horizontal displacement movement, and the fourth performed a Z-shaped block movement and a different depth (Figure 3C).
Optical parameter measurements
Luminance measurement
All luminance measurements were operated using a calibrated PR655 luminance meter (Photo Research, Inc., Chatsworth, CA, USA). The brightness filtered by red and blue glasses was measured in the conventional instrument. The procedure was repeated in the left and right viewing zones on the autostereoscopic device.
Crosstalk detection
The crosstalk was measured by a calibrated PR655 luminance meter (Photo Research, Inc., USA). The ratio of brightness filtered by blue glasses in red versus blue image mode was the crosstalk of blue glass; the crosstalk of red glass was obtained similarly. In the autostereoscopic device, the crosstalk was the ratio of crosstalk light and main light in the left or right viewing zone.
Spectrum test
Spectrum was assessed using a calibrated spectrograph (USB2000+; Ocean Optics, Shanghai, China). It was measured through the red and blue glasses respectively in the conventional instrument. The same procedure was repeated in the left and right viewing zones on the autostereoscopic device.
Participants
A total of 135 healthy participants at the Zhongshan Ophthalmic Center were recruited in this observational, analytic, cross-sectional study. The criteria of inclusion were as follows: patients with the best-corrected visual acuity of <0.1 logarithms of the minimum angle of resolution (logMAR) measured with the Early Treatment Diabetic Retinopathy Study (EDTRS) chart, and without ongoing or previous history of ocular surgery. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (No. 2016MEKY032). Informed consent was obtained from all participants. This study was registered at clinicaltrials.gov (ID NCT04152122).
Dynamic stereopsis assessment for participants
The specific procedure for the autostereoscopic dynamic stereopsis assessment device began when the participant sat in front of the device and started the software. Eye-tracking cameras identified their eyes and determined whether she/he was in an accurate position (Figure 4A). After entering their basic information, the participant clicked “Start” on a mobile phone connected to the device (Figure 4B). The test then ran automatically in 3 patterns. The participant chose the object that was different from the others and pressed the corresponding button on the phone (Figure 4C). This interactive software could tell the participant whether his/her answer was correct (Figure 4D,4E). The stereo acuity was shown on the mobile phone after the completion of all tests (Figure 4F).

The conventional instrument we chose was a computer-programmed random-dot stereopsis measuring software displayed on a 13.3-inch color monitor with a 1.6-GHz dual-core Intel Core i5, 256 GB (MacBook Air®; Apple, USA) using JAVA programming language. The specific procedure was performed as described in our previous study (7).
Test protocols for the 2 devices were the same. Participants were required to select the correct answer continuously 10 times at 1 stereoscopic level; those participants with 8 correct answers (80%) could be allowed to move to the next level. The examination started at 680" and raised the stereoscopic difficulty from 680" to 170" until the participant was unable to advance further.
Clinical repeatability evaluation
Ten randomly selected participants were enrolled in dynamic stereopsis assessments twice (with intervals of 24 hours) with the autostereoscopic device by a single examiner. The repeatability was evaluated by comparing the 2 testing results.
Clinical accuracy assessment
All 135 participants were enrolled to compare the screening accuracy between the autostereoscopic dynamic stereopsis assessment device and the conventional dynamic random-dot stereopsis measuring instrument. Each participant was asked to complete measurements on both devices in random order. A 10-minute washout period was included between the measurements.
Clinical acceptability judgment
The acceptance was evaluated by a 5-point grading questionnaire among the 135 participants. The higher the score, the higher the degree of favor, where 0 point meant “refuse it”, 1 points meant “do not refuse it”, 2 points meant “kind of like it”, 3 points meant “pretty much like it” and 4 points meant “love it”.
Clinical asthenopia rating
The asthenopia was also evaluated by a 5-point grading questionnaire among the 135 participants. The higher the score, the higher the degree of fatigue, where 0 point meant “no fatigue”, 1 points meant “mild fatigue”, 2 points meant “sub-moderate fatigue”, 3 points meant “moderate fatigue”, and 4 points meant “severe fatigue”.
Clinical efficiency calculation
The testing time spent in the process between the novel clinical dynamic stereopsis assessment based on an autostereoscopic display system and the conventional dynamic random-dot stereopsis measuring instrument was assessed for work efficiency among the 135 participants. The less time spent, the more efficient the device.
Statistical analysis
All statistical analyses were performed with the software SPSS 22.0 (IBM Corp., Armonk, NY, USA). The Shapiro-Wilk test was used to examine the distribution of the data. When the data met a normal distribution (such as efficiency, acceptability, and asthenopia), a paired t-test was performed to evaluate the differences between the 2 measurements. If the data did not meet a normal distribution (such as a dynamic stereoscopic score), a paired Wilcoxon test was performed to evaluate repeatability and accuracy between novel versus conventional devices. The test level was set as a =0.05, and P<0.05 demonstrated statistical significance. Cases with missing data were excluded from the analyses.
Results
The optical parameter comparison between the autostereoscopic device and the conventional instrument
We focused on comparing luminance, crosstalk, and the spectrum between the autostereoscopic dynamic stereopsis assessment device based on a directional backlight technology system and the conventional dynamic random-dot stereopsis measuring instrument under the same environment.
Luminance measurement
The autostereoscopic device projected a luminance of 139 cd/m2 to the left eye and 140 cd/m2 to the right eye. In the conventional instrument, the luminance dropped to 3.72 and 4.32 cd/m2, respectively (Table 1).
Table 1
| Optical parameter | Autostereoscopic dynamic stereopsis assessment device | Conventional dynamic random-dot stereopsis measuring instrument |
|---|---|---|
| Luminance for left eye (cd/m2) | 139 | 3.72 |
| Luminance for right eye (cd/m2) | 140 | 4.32 |
| Crosstalk for left eye | 4.50% | 27.8% |
| Crosstalk for right eye | 4.50% | 10.0% |
cd/m2, candela/m2.
Crosstalk detection
The crosstalk felt by both eyes was 4.50% in the autostereoscopic device; in the conventional instrument, the crosstalk felt by the left eye was 27.8% and the crosstalk felt by the right eye was 10.0% (Table 1).
Spectrum test
The wavelength of the spectrum revealed no changes in the color distribution in the absence of filtering glasses with the autostereoscopic device (Figure 5A). With the conventional instrument, participants were only sensitive to the light at around 450 nm for one eye and around 625 nm for the other eye, which could lead to chromatic aberration in binocular vision (Figure 5B).

The clinical evaluation between the autostereoscopic device and the conventional instrument
The clinical evaluation included a total of 135 healthy participants (103 females and 32 males) whose average age was 28.2±5.27 years (range: 18.0 to 45.0 years). The logMAR visual acuity of the participants, measured with the EDTRS chart was 0.04±0.02.
Clinical repeatability evaluation
Ten participants were selected to undergo a repeatability test. The stereo acuities from the first and the second tests were 170" in 3 patterns (Figure 6A-6C).

Clinical accuracy assessment
The stereo acuities (MD) measured with the autostereoscopic device and the conventional instrument were 170" (0.00") and 170" (0.00"), respectively. The difference was not statistically significant (Z =−1.000; P=0.317). As for the motion-only pattern (M), the stereo acuities were 170" (0.00") with the autostereoscopic device and 170" (0.00") with the conventional instrument (Z =−0.447; P=0.656). In the depth-only mode, stereo acuities were 170" (0.00") with the conventional instrument and 170" (0.00") with the conventional instrument. Again, the test results had no significant difference between the 2 devices (Z =−0.846; P=0.400) (Figure 7A-7C).

Clinical acceptability judgment
The autostereoscopic device had an acceptability score of 3.36±0.93 points, indicating that most subjects were in favor of this device. The conventional instrument only had a score of 2.02±0.59 points, meaning that this type of instrument was only acceptable for most subjects. The difference was statistically significant (P<0.001), indicating that the novel device was more popular than the conventional device (Figure 7D).
Clinical asthenopia rating
Asthenopia was evaluated based on the questionnaire. The score of the novel device was 0.27±0.46 points, and the conventional instrument was 0.73±0.66 points (P<0.001). This result suggested that the autostereoscopic device did not induce considerable visual fatigue (Figure 7E).
Clinical efficiency calculation
The testing times were 166±58.9 s for the autostereoscopic device and 298±116 s for the conventional instrument (P<0.001) (Figure 7F).
Discussion
In this study, we compared the optical parameters and clinical indexes between the novel clinical dynamic stereopsis assessment based on an autostereoscopic display system and a conventional dynamic random-dot stereopsis measuring instrument. The findings showed that the autostereoscopic device had excellent functions in both physical condition and clinical performance, suggesting the potential for future screening applications and popularization.
Optical parameters including luminance, crosstalk, and spectrum of screening equipment have a huge impact on displaying dynamic clues for clinical dynamic stereopsis assessment (12,13). Existing research shows that stereopsis is diminished over a range of illumination from photopic to scotopic light (21). In our study, the luminance of the autostereoscopic device was clearly within the photopic range, which was classified as good interior lighting (250 cd/m2) (22). However, when participants wore filter glasses, the perceived luminance dropped dramatically, with a 97.33% decrease in the left eye and a 96.91% decrease in the right eye, which caused a loss of stereopsis effects. An early study by Mueller and Lloyd (23) reported that the threshold of stereopsis decreased with changes in the field luminance from 1 cd/m2 to the lowest values (3×10-4 cd/m2). Many investigators now believe that stereopsis mainly depends on the level of illumination. Reduced luminance produces a temporal low-pass of neural response, resulting in secondary amplitude reduction and delay, which are particularly disruptive for stereopsis (24). The autostereoscopic device did not suffer a luminance decrease as the conventional instruments did, which demonstrated that the autostereoscopic device had a better ability for dynamic stereopsis assessment.
Screen performance of devices were compared: crosstalk de-camouflages test images. High levels of crosstalk cause a loss of fidelity in stereoscopic images. Therefore, it is crucial to maintain lower crosstalk in the stereo acuity assessment (25,26). Previous research revealed that 45° tilting of the head by participants wearing filter glasses resulted in 100% crosstalk in a random-dot stereopsis test (27). Degradation of stereopsis test accuracy by crosstalk may be associated with a violation of the fundamental principle of the stereo acuity assessment. Therefore, the examinations must exclude monocular cues (e.g., texture gradient, relative size) that would enable participants to perform correctly in the absence of stereo acuity. Crosstalk de-camouflages test images that should be detected only via stereopsis (28,29). In our study, the crosstalk of the new autostereoscopic device was significantly lower than that of the conventional instruments, suggesting that test results with the new approach would be more realistic.
The binocular chromatic aberration caused by filter glasses can also cause serious problems in stereo acuity assessment (30). Conventionally, the right eye observes test images through a red filter which appears red, while the left eye observes the images through a blue filter which appears blue. Although chromatic information could assist in stereopsis (31,32), previous studies have suggested that similarity, rather than difference, of color would extend the range of perceived stereopsis (33). The anti-correlations in color contrast degrades stereopsis (34). Kingdom et al. (35) concluded that it was unnecessary to pre-filter the image into separate color maps before the image underwent stereopsis processing for the visual system. Reports also tend to agree that visual features are somehow given a “label” based on their chromaticities and that stereoscopic matches with the same label are favored over those without (33,36). The conventional instruments had an obsolete chromatic stereopsis mechanism with limited stereo acuity (37). In contrast, the novel autostereoscopic device had a high color restoration degree that presented the dynamic stereopsis as closer to the actual state, which enabled more accurate dynamic assessments of stereopsis.
In the previous research, there was a dynamic stereoscopic measurement based on an autostereoscopic device called Nintendo’s 3DS (38). Compared with our device, there are slight differences in the technical principles of dynamic stereoscopic presentation. The Nintendo’s 3DS is a parallax-barrier autostereoscopic device with no detection floor of high-grade stereo. But would degrade in half the resolution and brightness of the dynamic image received by each eye. Our device is based on directional backlight technology. It ensures that each eye receives the full resolution and brightness of the dynamic image, which could better display dynamic clues for clinical dynamic stereopsis assessment.
Clinically, our autostereoscopic device demonstrated excellent accuracy and repeatability in a three-pattern evaluation. Moreover, according to the stereo acuity distribution comparison, 26 of 135 healthy participants with an abnormal range of stereo were recruited in this study. For this group of people, the accuracy of the device remained stable at a high level. Therefore, we could conclude that this autostereoscopic device had satisfactory precision in both normal stereo acuity and reduced stereo acuity, which was satisfied the requirements of dynamic stereopsis variability in the population assessment.
In terms of subjective evaluations, the autostereoscopic device had a lower fatigue score. We believe that this is mainly due to the advantages of optical parameters compared to conventional instruments. The brighter luminance, lower crosstalk, and higher color restoration degree of directional backlight technology provide separate images to each eye which allows visual representation to be closer to the human senses (39), offering a better stereopsis performance and lessening visual fatigue.
Furthermore, under the same testing protocol, besides higher acceptance and efficiency, the conventional instrument had a sizeable standard deviation of testing time (SD =116 s), indicating that there were substantial differences in adaptation of this examination among participants. In contrast, the autostereoscopic device had a lower standard deviation (SD =58.9 s), suggesting that participants could better understand and master the examination process. We assume that this difference would be mainly caused by the optimization of a user-friendly screening interface. The autostereoscopic device is equipped with interactive software and an eye-tracking camera. Participants can complete the assessments independently without the examiner's guidance. This not only saves time but adds more fun to the examination procedure, thus increasing efficiency and acceptance.
The novel clinical dynamic stereopsis assessment based on an autostereoscopic display system with excellent optical parameters, such as brighter luminance, lower crosstalk, and higher color restoration degree, could better display dynamic clues for clinical dynamic stereopsis assessment while maintaining equal accuracy as the conventional dynamic random-dot stereopsis measuring instrument does. Moreover, the novel assessment is of higher patient acceptance and lesser visual fatigue compared with the conventional assessment.
As for the limitations of this study, we believe that the optical parameters, such as resolution, could be further optimized to improve the screening ability such as presenting finer grade stereo and narrower spaced options. A thinner and lighter device that is portable can improve the dynamic stereopsis assessment experience either.
Conclusions
The novel clinical dynamic stereopsis assessment based on an autostereoscopic display system with brighter luminance, lower crosstalk, and higher color restoration contributes to the accurate presentation of dynamic stereopsis. Furthermore, its high-quality image and user-friendly interface enable the production of accurate screening results in all 3 dynamic stereopsis assessment task conditions with a higher level of acceptance and reduced visual fatigue. We believe that the autostereoscopic device, with excellent functions in both physical condition and clinical performance, has the potential for future screening applications and popularization.
Acknowledgments
The authors would like to express their gratitude to English Language Editors: C. Mullens and J. Jones for the expert linguistic services provided.
Funding: This study was supported partially by a grant from the Key Area Research and Development Program of Guangdong Province (No. 2019B010152001 to JY), and partially by a grant from the Science and Technology Program of Guangzhou (No. 202103000043 to JY).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-21-6700/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-21-6700/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-21-6700/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (No. 2016MEKY032), and informed consent was taken from all participants. This study was registered at clinicaltrials.gov (ID NCT04152122).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xiang A, Hang C, Wu X, et al. Detection of Static and Dynamic Stereopsis after Femtosecond Laser Small Incision Lenticule Extraction for High Myopia. J Ophthalmol 2021;2021:6667263. [Crossref] [PubMed]
- O'Connor AR, Tidbury LP. Stereopsis: are we assessing it in enough depth? Clin Exp Optom 2018;101:485-94. [Crossref] [PubMed]
- Matsuo T, Negayama R, Sakata H, et al. Correlation between depth perception by three-rods test and stereoacuity by distance Randot Stereotest. Strabismus 2014;22:133-7. [Crossref] [PubMed]
- Tidbury LP, Brooks KR, O'Connor AR, et al. A Systematic Comparison of Static and Dynamic Cues for Depth Perception. Invest Ophthalmol Vis Sci 2016;57:3545-53. [Crossref] [PubMed]
- Read JC. Stereo vision and strabismus. Eye (Lond) 2015;29:214-24. [Crossref] [PubMed]
- Maeda M, Sato M, Ohmura T, et al. Binocular depth-from-motion in infantile and late-onset esotropia patients with poor stereopsis. Invest Ophthalmol Vis Sci 1999;40:3031-6. [PubMed]
- Zhong J, Deng D, Chen Z, et al. A novel dynamic random-dot stereopsis assessment to measure stereopsis in intermittent exotropia. Ann Transl Med 2021;9:308. [Crossref] [PubMed]
- Hess RF, Mansouri B, Thompson B, et al. Latent stereopsis for motion in depth in strabismic amblyopia. Invest Ophthalmol Vis Sci 2009;50:5006-16. [Crossref] [PubMed]
- Allen B, Haun AM, Hanley T, et al. Optimal Combination of the Binocular Cues to 3D Motion. Invest Ophthalmol Vis Sci 2015;56:7589-96. [Crossref] [PubMed]
- Geng J. Three-dimensional display technologies. Adv Opt Photonics 2013;5:456-535. [Crossref] [PubMed]
- Kingdom FA, Simmons DR. Stereoacuity and colour contrast. Vision Res 1996;36:1311-9. [Crossref] [PubMed]
- Amigo G. Variation of stereoscopic acuity with observation distance. J Opt Soc Am 1963;53:630-5. [Crossref] [PubMed]
- Schor C, Heckmann T. Interocular differences in contrast and spatial frequency: effects on stereopsis and fusion. Vision Res 1989;29:837-47. [Crossref] [PubMed]
- Cui W, Gao L. Optical mapping near-eye three-dimensional display with correct focus cues. Opt Lett 2017;42:2475-8. [Crossref] [PubMed]
- Li X, Zhong J, Wang Y, et al. Rapid, accurate, multifunctional and self-assisted vision assessment and screening with interactive desktop autostereoscopy. Ann Transl Med 2021;9:23. [Crossref] [PubMed]
- Li X, Ding J, Zhang H, et al. Adaptive glasses-free 3D display with extended continuous viewing volume by dynamically configured directional backlight. OSA Continuum 2020;3:1555-67. [Crossref]
- He J, Zhang Q, Wang J, et al. Investigation on quantitative uniformity evaluation for directional backlight auto-stereoscopic displays. Opt Express 2018;26:9398-408. [Crossref] [PubMed]
- Wang J, Liang H, Fan H, et al. High-quality autostereoscopic display with spatial and sequential hybrid control. Appl Opt 2013;52:8549-53. [Crossref] [PubMed]
- Chen M, Li X, Zhang H, et al. Quantitative measurement and reduction of flicker in directional backlight autostereoscopic displays - ScienceDirect. Opt Commun 2020;458:124714. [Crossref]
- Serrano-Pedraza I, Clarke MP, Read JC. Single vision during an ocular deviation in intermittent exotropia. Ophthalmic Physiol Opt 2011;31:45-55. [Crossref] [PubMed]
- Livingstone MS, Hubel DH. Stereopsis and positional acuity under dark adaptation. Vision Res 1994;34:799-802. [Crossref] [PubMed]
- Geib T, Baumann C. Effect of luminance and contrast on stereoscopic acuity. Graefes Arch Clin Exp Ophthalmol 1990;228:310-5. [Crossref] [PubMed]
- Mueller CG, Lloyd VV. Stereoscopic Acuity for Various Levels of Illumination. Proc Natl Acad Sci U S A 1948;34:223-7. [Crossref] [PubMed]
- Reynaud A, Zhou J, Hess RF. Stereopsis and mean luminance. J Vis 2013;13:1. [Crossref] [PubMed]
- Woods AJ. How are crosstalk and ghosting defined in the stereoscopic literature? Stereoscopic Displays & Applications XXII 2012.
- Huang KC, Yuan JC, Tsai CH, et al. How crosstalk affects stereopsis in stereoscopic displays. Stereoscopic Displays & Applications 2003.
- Cormack LK, Stevenson SB, Landers DD. Interactions of spatial frequency and unequal monocular contrasts in stereopsis. Perception 1997;26:1121-36. [Crossref] [PubMed]
- Serrano-Pedraza I, Vancleef K, Read JC. Avoiding monocular artifacts in clinical stereotests presented on column-interleaved digital stereoscopic displays. J Vis 2016;16:13. [Crossref] [PubMed]
- Baker DH, Kaestner M, Gouws AD. Measurement of crosstalk in stereoscopic display systems used for vision research. J Vis 2016;16:14. [Crossref] [PubMed]
- Zhao L, Zhang Y, Wu H, et al. The difference in distance stereo acuity was measured with different separating methods. Ann Transl Med 2020;8:468. [Crossref] [PubMed]
- Jordan JR, Bovik AC. Using chromatic information in edge-based stereo correspondence. CVGIP: Image Understanding 1991;54:98-118. [Crossref]
- Jordan JR 3rd, Bovik AC. Using chromatic information in dense stereo correspondence. Pattern Recognit 1992;25:367-83. [Crossref]
- Jordan JR 3rd, Geisler WS, Bovik AC. Color is a source of information in the stereo correspondence process. Vision Res 1990;30:1955-70. [Crossref] [PubMed]
- Simmons DR, Kingdom FA. Interactions between chromatic- and luminance-contrast-sensitive stereopsis mechanisms. Vision Res 2002;42:1535-45. [Crossref] [PubMed]
- Kingdom FA, Li HC, MacAulay EJ. The role of chromatic contrast and luminance polarity in stereoscopic segmentation. Vision Res 2001;41:375-83. [Crossref] [PubMed]
- Kovaćs I, Julesz B. Depth, motion, and static-flow perception at metaisoluminant color contrast. Proc Natl Acad Sci U S A 1992;89:10390-4. [Crossref] [PubMed]
- Kingdom FA, Simmons DR, Rainville S. On the apparent collapse of stereopsis in random-dot-stereograms at isoluminance. Vision Res 1999;39:2127-41. [Crossref] [PubMed]
- Brown S, Rue C, Smith K, et al. Extraordinary Dynamic Near Vision in Champion Shotgun Shooters: PDI Check Evaluation of Stereo and Color without Floor Effect. Clin Ophthalmol 2021;15:575-81. [Crossref] [PubMed]
- Chen HW, Yeh SL. Effects of Blue Light on Dynamic Vision. Front Psychol 2019;10:497. [Crossref] [PubMed]