
The role of eye tracker in teaching video-assisted thoracoscopic surgery: the differences in visual strategies between novice and expert surgeons in thoracoscopic surgery
Introduction
Nowadays, more than 90% of surgeries conducted in the thoracic department are implement under thoracoscope (1). The associated changes in surgical techniques represent a significant challenge in educating young doctors. Compared to traditional surgery, the challenges of thoracoscopic surgery include two-dimensional spaciousness, hand coordination, the “Fulcrum” effect, and the lack of deep tactile feedback (2). Moreover, the feedback from the instrumentation is weak due to the long surgical instruments used. These challenges necessitate young doctors to practice for a long time before they become proficient. There is now increasing importance placed on visual feedback information in thoracoscopic surgery. Besides, in the surgery training, most of assessment are based on subjective judgement of surgeons. An objective evaluation instrument is lacking, which is associated with a decrease in the efficiency of the assessment of surgical learning and the blurred understandings of anatomical landmarks by young doctors (3).
Eye tracking technology is extensively used in scientific research across multiple disciplines. According to the survey conducted by Carter and Luke, in recent years, it reveals that there are nearly 32.75% eye movement studies have been implemented in the field of medicine and health care, approximately 17.86% in neuroscience (4). Eye tracking technology was applied to radiological image perception as early as the 1960s, and it has been used to identify the latent cognitive mechanisms of operation in doctors (5). The feature of eye tracking technology is that it can help researchers analyze the cognition of person by recording eye movement in specific scenes, so that they can understand how person use their knowledge and skills (6). Therefore, eye tracking may provide an innovative tool for quantifying and accelerating the learning rate of doctors, which can objectively and vividly feedback the learning process of knowledge. Studies which tracked eye movements in a virtual reality endoscopic surgery training exercise found that the gaze point of experienced doctors concentrated upon the surgical target, whereas novice doctors spent most of time checking the location of instruments so that their gaze point switched back and forth between instruments and the target (7,8). Wilson et al. used head-mounted eye trackers and found that the difference in gaze time between instruments and the target was less than 10% in novice surgeons, and indeed, the gaze time in the key area was very limited (9). Chetwood et al. used a Tobii tabletop eye tracker to demonstrated that in laparoscopic surgery, when the expert’s fixation point was transferred to the display screen, less time was required to complete the task, the accuracy rate was improved, and the reaction rate was accelerated (10). However, the use of head-mounted eye trackers is limited, as it is restrictive on the surgeon’s visual field and virtual reality systems are expensive.
In addition, while some simulators afford the opportunity to practice outside, these tend to lack significance in terms of anatomical structure and operational details in the thorax, and thus, novice thoracic surgeons must still watch surgical videos to improve their proficiency. Recently, eye tracking technology has been used to evaluate surgical skills (7). Some researchers have shown that students who underwent gaze training performed better than novices who underwent discovery learning (11). Fruitful research has been carried out and shows that eye tracking technology can be applied in the validated surgical assessment system owing to the good feature of analysis-objectivity and human visual system, such as the Objective Structured Assessment of Technical Skills (OSATS) (12).
At present, the use of eye tracking technology in China has been limited to reading, web design, driving in traffic, sports training, pilot training, and the like. This report explored novel ways of using eye tracking technology to enhance the efficiency of learning. Specifically, the study investigated whether following the expert surgeon’s eye movement trajectory during a surgical video would improve learning by novice surgeons. Developing effective methods to expedite the learning curve of novice thoracic surgeons will help integrate medical resources and optimize access to medical facilities. We present the following article in accordance with the MDAR reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2145/rc).
Methods
This study was performed at the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College and School of Languages and Communication Studies, Beijing Jiaotong University in June 2021. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (No. 2022020714364402). Beijing Jiaotong University and Beijing Chao-Yang Hospital were informed and agreed with this study. The study protocol is set out in Figure 1. Expert surgeons (who conduct more than 300 operations annually) and novice surgeons (postgraduate year 1–2) were recruited from the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College and Beijing Institute of Respiratory Medicine and Beijing Chao-Yang Hospital, Capital Medical University. Participation in the study was voluntary. A total of 52 thoracic surgeons (46 male and 6 female) participated in the study. Informed consent was taken from all the participants.
Equipment
The experiment equipment consisted of the entire setup of the Tobii Pro Lab from Beijing Jiaotong University’s School of Languages and Communication Studies. After attaching a portable eye tracker on the computer and calibrating it according to the manufacturer’s handbook, gaze data was collected using TobiiProFusion. The sample rate was 120 Hz, and the screen resolution was 1,920×1,080 pixels. After exporting the data in CSV format (Tobii Pro Lab 1.181), analysis was performed using the R version 4.1.3 (https://www.r-project.org). All eye tracker data of participants were qualified and further analyzed according to the research purpose.
Materials
A video showing the single-port thoracoscopic dissection of the mediastinal 2/4 lymph nodes (Video 1), lasting 16 minutes, was chosen. Two expert surgeons mark the key areas in different video segments once it had been segmented.
Procedure
There were two phases to this research. The first phase primarily compared the differences in how expert surgeons and novice surgeons watched the videos. The surgical video was then marked with expert surgeons’ eye movements based on the differences. In second phase, the novice surgeons were divided into two groups. The marked operation video was shown to group A, whereas the unmarked surgery video was shown to group B. After watching the video, the novices were given the same questionnaire. The groups were compared to determine whether watching the video labeled with the expert surgeons’ eye movement trajectory had a discernible effect on learning efficacy.
Eye tracking indicators
The indicators being commonly used contain three main types: saccade-based metrics, fixation-based metrics and event-based metrics. Saccade-based metrics contains saccade distance, saccade amplitude, regression count, and others, which can reflect contents obtaining and cognitive processing. Fixation-based metrics includes various basic indicators such as average fixation duration, fixation count, first fixation duration, which can be used to calculate fixation frequency, percentage of time fixating, fixation per image, reflecting attention in different locations, learning efficiency and cognitive processing difficulty. Event-based metrics were set to analyze a specific event during a trial or interval. Areas of interest (AOIs), times of interest (TOI) and heat map are most frequently In this study, four representative indicators were analyzed. The total duration of fixation reflects the efficiency of subjects in extracting effective information from video. The longer the total duration of fixation, the more difficult it is for surgeons to extract information and the greater the cognitive load. The time to entry saccade (saccade latency) and the number of saccades reflect the surgeons’ search process for key information. The peak velocity of saccade reflects the subjects’ strategy of watching video. The higher the peak, the faster the surgeon scan when watching the video.
Statistical analysis
Independent-sample t-tests were conducted to analyze the differences between the experts and novices in terms of overlap and the indexes of eye movement in the same area of interest (AOI). Repeated-measures analysis of variance (ANOVA) was used to analyze the indexes of eye movement in two separate AOI, with experience as the between-subjects factor (expert vs. novice) and AOI as the within-subjects factor (two separate areas). Results are presented as mean ± standard deviation (SD) unless otherwise stated. A P value <0.05 was considered statistically significant.
Results
The eye movement data of 16 thoracic surgeons (8 junior and 8 senior surgeons) watching the same surgical video was successfully recorded. The overlap among expert surgeons was 67.8% [n=8, standard deviation (SD) =1.3%] compared to 51.4% in novice surgeons (n=8, SD =2.7%). Figure 2A,2B show the gaze separation visualization for the expert group and the novice group, respectively. Figure 2C shows that the overlap of the expert group was significantly higher than that of the novice group, indicating that experienced thoracic surgeons were more focused on key target areas.

To facilitate the analysis of eye movement data, the 16-minute video was separated into 8 segments according to the different areas and steps in the operation. Two expert surgeons marked the AOIs in each video clip.
The total duration of fixation
Figure 3A shows a representative screenshot of the video clip. The blue region is region 1 (AOI-1) and the red region is region 2 (AOI-2). The effect between the two groups was significant [F(1, 16) =5.57, P<0.05], and the average fixation duration of experienced doctors was significantly lower than that of junior doctors (Figure 3B). Meanwhile, seniority and the AOI had no significant effect on experts [F(1, 16) =3.59, P<0.05; Figure 3C]. However, the difference in fixation duration between the two groups when observing AOI-2 was significantly higher than that when observing AOI-1, indicating that the doctors with less experience were less likely to notice the vagus nerve in AOI-2.

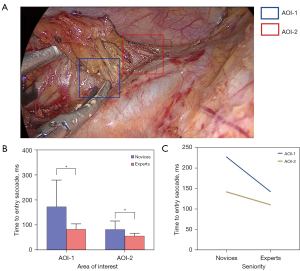
The time to entry saccade (saccade latency)
In the screenshot of the video clip shown in Figure 4A, the blue area is AOI-1 and the red area is AOI-2. The main effect between groups was significant [F(1, 16) =17.48, P<0.05], and the average saccade incubation period of expert doctors was significantly lower than that of novice doctors (Figure 4B). Meanwhile, the interactive effect between groups and the different areas was also significant [F(1, 16) =5.19, P<0.05; Figure 4C]. In AOI-1, both novice and expert doctors had longer saccade incubation periods than in AOI-2. However, the difference in the time to entry saccade between the two groups was significantly higher when AOI-1 was observed compared to the difference in fixation duration when AOI-2 was observed, indicating that the doctors with less experience were less likely to understand the operation in the AOI-1 region in the video.
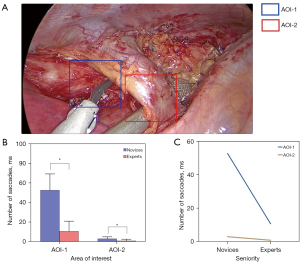
The number of saccades
In the screenshot of the video clip shown in Figure 5A, the blue area is AOI-1 and the red area is AOI-2. The main effect between groups was significant [F(1, 16) =96.45, P<0.05], and the number of saccades of expert doctors was significantly less than that of novice doctors (Figure 5B). Meanwhile, the interaction between groups and different regions was also significant [F(1, 16) =43.32, P<0.05; Figure 5C].
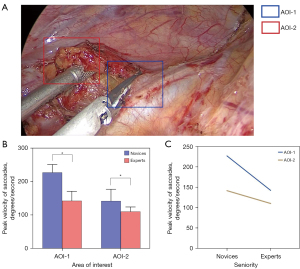
The peak velocity of saccade
In the screenshot of the video clip shown in Figure 6A, the blue area is AOI-1 and the red area is AOI-2. The main effect between groups was significant [F(1, 16) =34.30, P<0.05], and the peak velocity of saccade of expert doctors was significantly lower than that in novice doctors (Figure 6B). Meanwhile, the interaction between groups and different regions was also significant [F(1, 16) =7.02, P<0.05; Figure 6C].
External blinded review of performance
To determine whether the eye movement trajectory of an expert thoracic surgeon is helpful to the surgical video learning of novices, we invited an expert thoracic surgeon to watch a complete video of the left upper lung lobotomy and lymph node dissection and recorded the eye movement trajectory of the surgeon. Subsequently, 36 doctors with low experience were recruited, and their understanding of the surgical procedures involved in left upper lung lobotomy with lymph node dissection was assessed using a questionnaire. The 36 doctors were then divided into two groups according to the distribution of the assessment scores, so that the baseline of the questionnaire assessment of the two groups was consistent. Subsequently, one group of doctors watched the original surgical video (group A) and the other group (group B) watched the surgical video that showed the senior thoracic surgeon’s eye movements. After watching the video, doctors in the two groups were assessed by questionnaire again (the post-test). The results showed that doctors in group B scored significantly higher than those in group A (mean ± SD, 79.6±2.59 vs. 83.2±2.22, P=0.007), especially in the item of Knowledge of Special Procedures and Operational Precautions.
Discussion
In this research, eye movement analysis demonstrated significant differences in the gaze patterns between novices and experts while watching surgical videos. Novice doctors lacked the ability to search for details and often tended to deviate from the key areas of the surgery. Subsequently, an external blinded review demonstrated that novices who watched the surgical video containing marked eye movements of expert physicians had significantly improved understanding of the surgery and were more likely to notice specific surgical details compared to novices who watch the original surgical video.
Previously, eye tracking technology was mainly used for medical diagnosing, therapy and disclosing medical experts’ visual patterns (13). For helping children use vision more effectively, researchers try to use eye tracking technology to assessment of the vision quality in case of children with vision impairments. Besides, eye tracking based training is useful for rehabilitation. Disclosing visual patterns is one of most important applications of eye tracking technology in medicine, and such researches are related to many areas, especially medical education. Indeed, distinguishing visual patterns of novices and experts are the main purpose for using eye tracking technology in our study.
At present, most operations in thoracic surgery involve thoracoscopy. Therefore, especially for young thoracic surgeons, it is necessary to learn anatomical details and surgical operation skills by watching surgical videos. We selected a video of a lymph node dissection in 2/4 groups as the stimulus material to compare the fixation patterns between novices and experts. The expert group who are familiar with this mode of surgery, showed a high gaze overlap. However, due to the lack of unified surgical strategies, the gaze overlap was low among novices, and this provided an objective evaluation method for assessing the efficacy of learning in novice doctors. The reasons for the difference in visual strategies between novice and expert surgeons are mainly as follows: (I) novices are not familiar with the main points of anatomy and the whole process of surgery, so they need to spend more time searching for the key steps of surgery; (II) for lacking operation experience in surgical instruments, novice doctors have to spend more attention to observe the skills in using these instruments. In the future, eye tracking technology may be applied to the actual surgical operation to evaluate the performance of different levels of doctors. The eye movement trajectory of experts may be used during operations by novice doctors to further improve their efficiency. Thus, this technique can not only be used as an effective monitoring method, but may also represent a potential auxiliary method to improve the efficiency of learning.
Analysis of the eye movement data revealed that the total fixation time of novice doctors was significantly longer than that of expert doctors under time and task constraints. Harvey et al. (14) showed that low-experience surgeons had significantly shorter total gaze duration compared to high-experience surgeons when dissecting and separating specific areas. The latter study also suggested that the lack of experience in a particular procedure might lead to distraction and shortened fixation. We believe that the less the surgeon knows about the operation, the greater the demand for attention load, so novice surgeons need to spend more energy to watch and understand the surgical. In addition, the eye gaze of the same doctor when watching the video of the operation and during the actual operation may differ (12), and this may give rise to different results.
Saccade latency reflects the time from the presentation of the stimulus to the beginning of the first saccade, and the longer the latency period, the more difficult it is for the video viewer to process the AOI. In Figure 4, it was evident that the novice thoracic surgeons were less familiar with the procedure of vagus nerve recognition and preservation than the expert thoracic surgeons. Especially in critical areas of surgery, less senior physicians must pay more attention to identifying nerves that need to be preserved. The number of saccade and peak velocity of saccades reflect the ability of the doctor’s search process and saccade speed. Expert surgeons can focus directly on the targeted areas and thus, have fewer number of saccades and lower peak velocity of saccades. Novice surgeons spend more time in unrelated areas, suggesting that they have not yet established a fixed approach to surgery. However, the interactive effect showed that novice doctors and expert doctors had similar eye movement trajectory when they focused on the two different regions, indicating that novice doctors also had certain cognitive ability for the operation.
The visual fixation strategies of experienced thoracic surgeons reflected the interaction and efficient integration of goal-task-oriented and stimulus-driven intent. When watching surgical videos, experienced thoracic surgeons presented efficient attention control strategies oriented to key anatomical structures. Although the novice group showed a key region-oriented attentional control strategy, the fixation trajectory was relatively scattered and thus, the efficiency of the search requires improvement in the key areas. Meanwhile, the ability to distinguish important anatomical structures from non-important anatomical structures requires strengthening. Indeed, novice thoracic surgeons may passively focus on key areas while watching surgical videos marked with the eye movement trajectory of expert doctors, thereby achieving a detailed comprehension of the anatomical structures and areas to avoid. However, there is still great challenge to combine eye tracking with high-fidelity clinical simulations. To achieve this, we must break out of two technical limitations: lighter wearable eye tracker with higher accuracy and more intelligent sensor. Some studies have integrated both eye tracking and augmented reality technology into clinical simulations (15-17). Through this approach, doctors can have a more realistic training experience. Lu et al. designed a surgical training platform, which is a convergence of multiple technologies, consisting of an Augmented Reality (AR) device, eye-tracker and a system named Surgical Simulation Research Lab. On this platform, trainees can practice in a more efficient way by being guided through text or image instruction (15).
Moreover, based on existing studies (18,19), considering eye tracking as the primary sensor modality for emotion detection is one of up-to-date hot topic in the area of eye movement field. Yang et al. found that there has a strong correlation between facial emotion recognition and eye movement features (18). Combined with deep learning technology, they designed a prediction model for children’s speech communication disorders screening. Ding et al. used a combination of eye tracking, galvanic skin response measurement and electroencephalography technology to build a classification model for major depression disorder diagnosis (19). Here, the eye movement metrics was mainly applied for emotional expression detecting. However, the related researches are mainly founded in psychology field, it has not been applied in surgery yet. We expect more studies exploring the eye tracking technology’s emotion detecting features concerning surgeries or any other medical problems.
Conclusions
This study demonstrated significant differences in the eye fixation patterns and search strategies between novice and expert surgeons when watching videos of thoracoscopic surgery. Novice thoracic surgeons can significantly improve their learning efficiency and expedite their learning curve by watching surgical videos marked with expert eye movement trajectories. In the future, eye tracking is expected to be used in thoracoscopic surgery to assist young doctors in real-time.
Acknowledgments
Funding: This work was supported by the Beijing Chao-Yang Hospital Golden Seeds Foundation (No. CYJZ202130).
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2145/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2145/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2145/coif). All authors report that this work was supported by the Beijing Chao-Yang Hospital Golden Seeds Foundation (No. CYJZ202130). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (No. 2022020714364402). Informed consent was taken from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gao S, Li N, Wang S, et al. Lung Cancer in People’s Republic of China. J Thorac Oncol 2020;15:1567-76. [Crossref] [PubMed]
- Hogle NJ, Chang L, Strong VE, et al. Validation of laparoscopic surgical skills training outside the operating room: a long road. Surg Endosc 2009;23:1476-82. [Crossref] [PubMed]
- Merali N, Veeramootoo D, Singh S. Eye-Tracking Technology in Surgical Training. J Invest Surg 2019;32:587-93. [Crossref] [PubMed]
- Carter BT, Luke SG. Best practices in eye tracking research. Int J Psychophysiol 2020;155:49-62. [Crossref] [PubMed]
- Law B, Atkins MS, Lomax AJ, et al. Eye trackers in a virtual laparoscopic training environment. Stud Health Technol Inform 2003;94:184-6. [PubMed]
- Kok EM, Jarodzka H. Before your very eyes: the value and limitations of eye tracking in medical education. Med Educ 2017;51:114-22. [Crossref] [PubMed]
- Richstone L, Schwartz MJ, Seideman C, et al. Eye metrics as an objective assessment of surgical skill. Ann Surg 2010;252:177-82. [Crossref] [PubMed]
- Tien T, Pucher PH, Sodergren MH, et al. Eye tracking for skills assessment and training: a systematic review. J Surg Res 2014;191:169-78. [Crossref] [PubMed]
- Wilson MR, McGrath JS, Vine SJ, et al. Perceptual impairment and psychomotor control in virtual laparoscopic surgery. Surg Endosc 2011;25:2268-74. [Crossref] [PubMed]
- Chetwood AS, Kwok KW, Sun LW, et al. Collaborative eye tracking: a potential training tool in laparoscopic surgery. Surg Endosc 2012;26:2003-9. [Crossref] [PubMed]
- Wilson MR, Vine SJ, Bright E, et al. Gaze training enhances laparoscopic technical skill acquisition and multi-tasking performance: a randomized, controlled study. Surg Endosc 2011;25:3731-9. [Crossref] [PubMed]
- Khan RS, Tien G, Atkins MS, et al. Analysis of eye gaze: do novice surgeons look at the same location as expert surgeons during a laparoscopic operation? Surg Endosc 2012;26:3536-40. [Crossref] [PubMed]
- Harezlak K, Kasprowski P. Application of eye tracking in medicine: A survey, research issues and challenges. Comput Med Imaging Graph 2018;65:176-90. [Crossref] [PubMed]
- Harvey A, Vickers JN, Snelgrove R, et al. Expert surgeon’s quiet eye and slowing down: expertise differences in performance and quiet eye duration during identification and dissection of the recurrent laryngeal nerve. Am J Surg 2014;207:187-93. [Crossref] [PubMed]
- Lu S, Sanchez Perdomo YP, et al. Integrating Eye-Tracking to Augmented Reality System for Surgical Training. J Med Syst 2020;44:192. [Crossref] [PubMed]
- Desvergez A, Winer A, Gouyon JB, et al. An observational study using eye tracking to assess resident and senior anesthetists' situation awareness and visual perception in postpartum hemorrhage high fidelity simulation. PLoS One 2019;14:e0221515. [Crossref] [PubMed]
- Tanoubi I, Tourangeau M, Sodoké K, et al. Comparing the Visual Perception According to the Performance Using the Eye-Tracking Technology in High-Fidelity Simulation Settings. Behav Sci (Basel) 2021;11:31. [Crossref] [PubMed]
- Yang J, Chen Z, Qiu G, et al. Exploring the relationship between children’s facial emotion processing characteristics and speech communication ability using deep learning on eye tracking and speech performance measures. Comput Speech Lang 2022;76. [Crossref]
- Ding X, Yue X, Zheng R, et al. Classifying major depression patients and healthy controls using EEG, eye tracking and galvanic skin response data. J Affect Disord 2019;251:156-61. [Crossref] [PubMed]
(English Language Editor: J. Teoh)



