
Association between bilirubin and nonalcoholic fatty liver disease in the non-obese Chinese population: a cross-sectional study
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a spectrum of fatty liver disease that is not caused by excessive alcohol consumption, viral infections, autoimmunity, drugs, or genetics. NAFLD is a common cause of chronic liver diseases worldwide, is associated with metabolic disorders such as diabetes mellitus, obesity, hyperlipidemia, and hypertension (1), and has recently attracted the name of metabolic associated fatty liver disease (MAFLD) (2). With its significant clinical importance and high prevalence of 20–30% in western countries and 15–30% in China (3), NAFLD has become a global public health problem (4).
Although it is closely associated with obesity, and the prevalence of NAFLD among obese individuals is higher than that among lean individuals, the condition is still common among non-obese individuals and its prevalence in this group is increasing (5). A previous study has shown that 8–19% of NAFLD patients in Asia are not obese, a phenomenon known as “non-obese NAFLD” or “lean NAFLD” (6). A population-based study in the United States found those with lean NAFLD [body mass index (BMI) <25 kg/m2] accounted for 17.3% of the entire NAFLD cohort (7). And among the non-obese Chinese population, the prevalence is 7.3% (8). Compared with obese patients with NAFLD, lean patients with the condition are often asymptomatic, making diagnosis difficult and rendering patients at greater risk of developing severe liver diseases and nonalcoholic steatohepatitis (NASH) in the future (9). NAFLD in non-obese participants calls for prompt recognition and early management.
The major risk factors for NAFLD are obesity, dyslipidemia, diabetes mellitus, insulin resistance, metabolic syndrome (10,11). Although the etiology of NAFLD remains unknown, oxidative stress has been suggested as a possible pathogenic mechanism (12). Research has indicated that feeding azo compounds generating free radicals to rats leads to the accumulation of fat in the liver (13). In addition, the accumulation of liver fat can be suppressed by taking in antioxidants scavenging free radicals (14). Bilirubin, the metabolic end product of heme catabolism, is an important antioxidant cytoprotective agent in physiological conditions and plays an important role in preventing oxidative stress (15), as it can effectively scavenge and suppress hydrogen peroxide free radicals, inhibiting serum low-density lipoprotein cholesterol (LDL-C) peroxidation (16). A growing number of studies have suggested high bilirubin levels are inversely correlated with insulin resistance and the prevalence of cardiovascular diseases and diabetes mellitus (17-19). Therefore, it can be inferred that high serum bilirubin levels may reduce oxidative stress, inflammation, and is inversely associated with NAFLD. A cross-sectional study shows that serum bilirubin levels are inversely associated with NAFLD (20). However, another study suggests that bilirubin levels is not associated with fatty liver (21). Most of the previous studies are not based on population, and the sample size is relatively small. So far, the correlation between serum bilirubin and NAFLD remains unclear, requiring further investigation. In addition, the epidemiological data on bilirubin NAFLD are mainly from Europe and the United States. However, Chinese people have a lower BMI than those in western countries but a similar prevalence of NAFLD, suggesting the metabolic profiles of non-obese Chinese adults may be different from those of their western counterparts (22). Therefore, we conducted a large cross-sectional study aimed at investigating the association between serum bilirubin and NAFLD in non-obese Chinese adults. The results of this study will potentially advance for the early diagnosis and prevention of NAFLD in non-obese population. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1187/rc).
Methods
Study participants
This study was an ancillary study of the Wuwei Cohort, which is a population-based cohort for the study of gastric cancer in China involving 23,346 participants aged 35–70 years living in Wuwei using a cluster sampling method. The cohort completed the epidemiological investigation at baseline, and among them 21,345 participants underwent gastroscopies, 14,747 took laboratory tests (23), and 15,855 participants volunteered to receive free abdominal ultrasonography. A further 4,952 non-obese (BMI <25 kg/m2) subjects had complete biochemical profiles. With the exclusion of 52 patients with viral hepatitis B, 4,900 subjects were eventually included in our cross-sectional study.
The Ethics Committee of the First Hospital of Lanzhou University approved of this study (approval No. LDYYLL2012001) and this study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and all participants gave written informed consent.
Demographic and clinical data
Trained interviewers acquired participants' data through standardized and structured questionnaires with contents involving sociodemographic characteristics (age, sex, education, occupation, marital status, and household income), smoking, drinking, insomnia, hypersomnia, body mass index (BMI), and medical history (hypertension, diabetes). Participants were classified as smokers if they had smoked at least one cigarette per day in the past 6 months or if they had. Those who had consumed at least 1,000 grams of beer, 150 grams of wine, or hard liquor at least once per week during the past year were defined as alcohol consumers. Height, weight and waist circumference were measured by trained staff, and BMI was identified as weight (in kilograms) divided by the square of height (in meters). Blood pressure was tested in compliance with standardized methods.
Diagnostic criteria
The diagnosis of NAFLD was based on the diagnosis and treatment guidelines of the Chinese Liver Disease Association (24), according to which, abdominal ultrasonography findings, medical history, clinical symptoms, and laboratory findings were taken into account. Patients with hepatitis, other liver diseases, or with excessive alcohol intake (more than 140 grams per week for men and more than 70 grams per week for women) were screened out. The conventional criterion for obesity in Asia is BMI ≥25 kg/m2, and Asian NAFLD patients with BMI below 25 kg/m2 are often described as having “lean” or “non-obese” NAFLD (6).
Ultrasonographic examinations
A Mindray DC-8 ultrasound system (Mindray, Shenzhen, China) and 3.5 MHz probe were used, and ultrasound operators were blinded to the diagnosis. Diagnosis of fatty liver was based on the following ultrasound criteria: attenuated depths, blurring blood vessels, scattered and amplified echoes, and kidney or spleen echoes (25).
Biochemical tests
Blood samples of those who fasted the previous night were obtained for analysis of biochemical variables including total bilirubin (TBIL), direct bilirubin (DBIL), indirect bilirubin (IBIL), alanine aminotransferase (ALT), aspartate aminotransferase (AST), triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), renal functions, and blood glucose. Variables were measured with an automated biochemical analyzer (Beckman Coulter AU5831, Brea, CA, USA).
Statistical analyses
Baseline characteristics were summarized using means and standard deviations or medians (interquartile ranges) for continuous data, or percentages for categorical data, respectively. Comparisons were performed using Student’s t-test, Mann-Whitney U test, or χ2 test where appropriate. Tertiles were adopted to group serum bilirubin. Logistic regression models were adopted to calculate the association between bilirubin and NAFLD, three models were generated with odds ratios (OR) per SD and 95% confidence intervals (95% CI) in the following stages: (I) Model 1 was constructed without adjusting. (II) A second model was created after adjusting age, sex, education, income, occupation, smoking, medical histories of hypertension and diabetes mellitus, BMI, and waist circumference. (III) Model 3 was constructed after additionally adjusting for ALT, AST, TC, TG, HDL-C, LDL-C, and blood glucose. All statistical analyses were performed using Stata software (version 15.0), and a two-tailed P value <0.05 was considered to indicate statistical significance.
Results
A total of 4,900 non-obese subjects (BMI <25 kg/m2) were included in this study, 408 subjects (203 men) of whom were diagnosed with NAFLD, with a mean age of 51.73±7.69 years. In Table 1, the clinical characteristics of study subjects with and without NAFLD are compared. As expected, compared with the controls, NAFLD patients were older with higher BMI, larger waist circumference, higher systolic and diastolic blood pressure (P<0.001), and inferior educational attainments (P=0.001). Subjects with NAFLD also had higher serum ALT, TC, TG, LDL-C, and glucose levels (P<0.001), but lower HDL-C (P<0.001) levels than controls. Non-obese NAFLD patients had lower DBIL than controls without NAFLD [2.50 (1.80–3.25) vs. 2.60 (1.90–3.50), P=0.004] but no significant differences in IBIL and TBIL levels of the two groups was seen (both P>0.05).
Table 1
| Variables | Non-NAFLD | NAFLD | P value |
|---|---|---|---|
| N | 4,492 | 408 | |
| Age (years) | 49.96±7.94 | 51.73±7.69 | <0.001 |
| Male | 2,051 (45.66) | 203 (49.75) | 0.112 |
| Education | 0.001 | ||
| Illiteracy | 726 (16.16) | 91 (22.30) | |
| Primary school | 1,638 (36.46) | 152 (37.25) | |
| High school | 2,117 (47.13) | 162 (39.71) | |
| College degree or above | 11 (0.24) | 3 (0.74) | |
| Occupation (% farmer) | 4,221 (93.97) | 372 (91.18) | 0.026 |
| Incomea (RMB, Yuan) | 20,000 (10,000–30,000) | 20,000 (10,000–30,000) | 0.052 |
| Body mass index (kg/m2) | 22.26±1.80 | 23.30±1.39 | <0.001 |
| Waist circumference (cm) | 81.63±7.55 | 84.82±7.37 | <0.001 |
| SBP (mmHg) | 120.23±13.86 | 126.37±14.32 | <0.001 |
| DBP (mmHg) | 75.96±9.27 | 78.29±10.12 | <0.001 |
| Smoking | 0.087 | ||
| No | 3,028 (67.60) | 280 (68.80) | |
| Currentb | 1,329 (29.67) | 109 (26.78) | |
| Past | 122 (2.72) | 18 (4.42) | |
| Alcoholc | 166 (3.70) | 15 (3.68) | 0.984 |
| Insomnia | 0.388 | ||
| No | 3,902 (86.87) | 363 (88.97) | |
| Mild | 447 (9.95) | 36 (8.82) | |
| Moderate | 130 (2.89) | 7 (1.72) | |
| Severe | 13 (0.29) | 2 (0.49) | |
| Hypersomnia | 0.636 | ||
| No | 1,535 (34.17) | 141 (34.56) | |
| Mild | 2,914 (64.87) | 265 (64.95) | |
| Moderate | 43 (0.96) | 2 (0.49) | |
| History | |||
| Hypertension | 441 (9.82) | 87 (21.32) | <0.001 |
| Diabetes | 85 (1.89) | 34 (8.33) | <0.001 |
| ALT (U/L) | 23.00 (17.00–34.00) | 28.00 (19.00–41.00) | <0.001 |
| AST (U/L) | 29.00 (25.00–37.00) | 29.50 (24.00–37.00) | 0.809 |
| TBIL (μmol/L) | 11.20 (8.70–14.90) | 11.20 (8.70–14.50) | 0.893 |
| DBIL (μmol/L) | 2.60 (1.90–3.50) | 2.50 (1.80–3.25) | 0.004 |
| IBIL (μmol/L) | 8.70 (6.60–11.50) | 9.05 (6.70–11.45) | 0.417 |
| TC (mmol/L) | 4.51 (3.93–5.17) | 4.92 (4.25–5.65) | <0.001 |
| TG (mmol/L) | 1.30 (0.96–1.81) | 1.90 (1.33–2.80) | <0.001 |
| HDL-C (mmol/L) | 1.17 (1.01–1.36) | 1.09 (0.92–1.29) | <0.001 |
| LDL-C (mmol/L) | 2.72 (2.29–3.22) | 2.97 (2.48–3.47) | <0.001 |
| Blood glucose (mmol/L) | 4.78 (4.38–5.21) | 5.14 (4.62–5.68) | <0.001 |
Data are presented as n (%) or mean standard deviation (SD). a, increase annual family income (RMB, Yuan). b, current smokers were defined as those who smoked at least one cigarette per day in the past 6 months. c, drinkers were defined as those who drank at least 1,000 g of beer, 150 g of wine or hard liquor at least once per week during the past year. NAFLD, nonalcoholic fatty liver disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; AST, aspartate aminotransferase; ALT, alanine aminotransferase; TBIL, total bilirubin; DBIL, direct bilirubin; IBIL, indirect bilirubin; TC, total cholesterol; TG, total triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Multivariate logistic regression model analysis was applied to determine the association between serum bilirubin levels and NAFLD. As shown in Table 2, in Model 1, where no adjustments of parameters were made, compared with tertiles of the lowest DBIL level, the OR (95% CIs) of subjects with the highest DBIL tertiles for NAFLD are 0.85 (0.75–0.96), P trend =0.0097. In addition, the association still exists after adjustments of possible confounders (Model 2), including age, gender, education background, income, occupation, smoking, medical histories of hypertension and diabetes mellitus, BMI, and waist circumference (OR: 0.83, 95% CI: 0.73–0.95, P trend =0.0074). However, when AST, ALT, TC, TG, HDL-C, LDL-C, and glucose were adjusted (Model 3), serum DBIL levels were no longer associated with the NAFLD risk (OR: 0.96, 95% CI: 0.83–1.11, P trend =0.6022). After adjusting confounding factors, multivariate analysis showed serum IBIL (OR: 1.02, 95% CI: 0.89–1.17, P trend =0.7756), and TBIL (OR: 1.00, 95% CI: 0.87–1.15, P trend =0.991) levels were not associated with NAFLD in the non-obese population. We also performed stratified analyses according to age, gender, and medical histories of hypertension and diabetes mellitus (Tables S1-S8), and regardless of these parameters, no significant association between bilirubin (TBIL, DBIL, IBIL) and NAFLD was observed after the adjustment of confounders in any of the models.
Table 2
| Variables | Model 1a | Model 2b | Model 3c | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||
| TBIL (μmol/L) | |||||||||||
| ≤9.5 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | |||||
| 9.6–13.6 | 1.14 | 0.90, 1.46 | 0.2803 | 1.09 | 0.85, 1.40 | 0.5002 | 1.16 | 0.90, 1.51 | 0.255 | ||
| ≥13.7 | 0.94 | 0.73, 1.22 | 0.6604 | 0.88 | 0.67, 1.15 | 0.3478 | 1 | 0.75, 1.32 | 0.9833 | ||
| P for trend | 0.97 | 0.86, 1.10 | 0.6861 | 0.94 | 0.83, 1.07 | 0.3644 | 1 | 0.87, 1.15 | 0.991 | ||
| DBIL (μmol/L) | |||||||||||
| ≤2.2 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | |||||
| 2.2–3.2 | 0.93 | 0.74, 1.18 | 0.5567 | 0.93 | 0.73, 1.19 | 0.5544 | 1.04 | 0.80, 1.34 | 0.7705 | ||
| ≥3.3 | 0.71 | 0.54, 0.91 | 0.0083 | 0.68 | 0.52, 0.90 | 0.0062 | 0.92 | 0.69, 1.22 | 0.5538 | ||
| P for trend | 0.85 | 0.75, 0.96 | 0.0097 | 0.83 | 0.73, 0.95 | 0.0074 | 0.96 | 0.83, 1.11 | 0.6022 | ||
| IBIL (μmol/L) | |||||||||||
| ≤7.3 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | 1 | 1.00, 1.00 | |||||
| 7.4–10.5 | 1.19 | 0.93, 1.52 | 0.1704 | 1.15 | 0.89, 1.48 | 0.2839 | 1.18 | 0.91, 1.54 | 0.2185 | ||
| ≥10.6 | 1.06 | 0.82, 1.37 | 0.6411 | 1 | 0.77, 1.31 | 0.9735 | 1.04 | 0.79, 1.37 | 0.7804 | ||
| P for trend | 1.03 | 0.91, 1.17 | 0.6306 | 1 | 0.88, 1.14 | 0.9632 | 1.02 | 0.89, 1.17 | 0.7756 | ||
a, Model 1 was constructed without adjusting. b, Model 2 were created after adjusting age, sex, education, income, occupation, smoking, medical histories of hypertension and diabetes mellitus, BMI, and waist circumference. c, Model 3 was constructed after additionally adjusting for ALT, AST, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and blood glucose. The OR for the control group was taken as 1, and each group was compared with the control group. NAFLD, nonalcoholic fatty liver disease; TBIL, total bilirubin; DBIL, direct bilirubin; IBIL, indirect bilirubin.
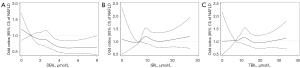
Figure 1 shows the ORs for NAFLD patients calculated based on serum bilirubin levels. This shows a downward trend in the DBIL level of NAFLD patients as it drops sharply at first and then slowly, with the curve beginning to flatten from the point of 4.5 µmol/mL (Figure 1A). However, for IBIL and TBIL, no obvious association is observed (Figure 1B,1C, respectively).
Discussion
In this study, we explored the association between serum bilirubin levels and NAFLD in non-obese Chinese adults and found they had lower serum DBIL levels than controls without NAFLD. However, after adjusting many other potential confounding factors such as BMI, blood glucose, and lipids, no correlation between serum bilirubin levels and NAFLD prevalence was discovered. These findings suggest serum bilirubin levels are unlikely to be associated with the risk of NAFLD in non-obese subjects.
NAFLD is a major liver disease closely related to obesity. However, a previous study has indicated its prevalence among the non-obese population is as high as around 15% (5). The global prevalence of non-obese NAFLD is increasing substantially, and although these patients are often asymptomatic, they may develop all the histopathological features of NASH, such as steatosis, lobular inflammation, hepatocyte ballooning, and/or fibrosis (26). Furthermore, despite having relatively low body weight, nearly 20% of the non-obese population have unhealthy metabolic conditions (27). Non-obese patients with NAFLD have similar complications and comorbidities as obese patients with the condition, such as type 2 diabetes, cardiovascular diseases, and hepatocellular carcinoma (26,28). Therefore, the identification of risk factors for NAFLD among non-obese people is of great help in screening high-risk groups and has important clinical implications for the prevention and management of the condition. While the pathophysiology and risk factors for NAFLD in non-obese individuals are not fully known, they appear to be closely associated with insulin resistance, atherosclerotic dyslipidemia, and altered body compositions, with some patients having susceptibility gene polymorphisms (29). The lifestyles and genetic profiles of Chinese people are different from those of western people, and with the increasing prevalence of NAFLD among the non-obese population, it is of vital importance to assess risk factors for this group in China.
Total circulating serum bilirubin, the final product of heme catabolism, has two forms, IBIL and DBIL, and is oxidation resistant and cytoprotective (30). However, there is a little evidence to prove an association between serum bilirubin levels and NAFLD. While most studies have indicated that low serum bilirubin levels are associated with high risks of NAFLD, Kwak et al. (20) have discovered that serum bilirubin levels are inversely associated with its prevalence, independent of known metabolic risk factors. However, in their study, the adjustments of key confounders that might have affected the results, such as TC, HDL-C, LDL-C, and glucose, were neglected. In a prospective study of middle-aged workers in South Korea, the results revealed the higher the serum DBIL level, the lower the risk of NAFLD, and the two were significantly associated with each other even when various metabolic parameters were adjusted. However, neither serum TBIL nor IBIL levels were significantly associated with the incidence of NAFLD (31). In a study of children with biopsy-proven NAFLD, Puri et al. (32) found 67% of subjects had evidence of NASH, and multivariate analysis indicated high bilirubin levels were inversely associated with the prevalence of histologically diagnosed NASH. In a Chinese study of middle-aged and elderly populations, DBIL was also seen to be inversely associated with the risk of NAFLD, while TBIL and IBIL had no significant association (33).
Several other studies have supported our findings. Recently, two different studies conducted in China (34) and the Netherlands (35) to assess the association between TBIL and the risk of new-onset NAFLD and to investigate the causal nature of the association using Mendelian randomization, and the multivariate analysis indicated rising TBIL levels were not causally associated with NAFLD. In a retrospective cross-sectional study of 1,672 participants aged 5–18 conducted by Bellarosa et al. (21), the result suggested bilirubin was not associated with fatty liver and could not help to resist NAFLD when an individual is considerably obese.
The strengths of our study lie in the large sample size and the adoption of the cluster sampling approach, with detailed information on the demographics, lifestyle, medical and occupational history of each subject, along with their abdominal ultrasonography results and biochemical marker measurements. However, this study also has some limitations. First, the diagnosis of NAFLD is based on ultrasonography, which may not be sensitive enough to detect mild steatosis and cannot replace the gold standard of liver biopsy. Second, the subjects included in the cohort study are from the Chinese Wuwei population, so, the findings may not fully apply to people in general or other ethnic groups. Third, this is a cross-sectional study, and its results should be validated in a large-scale prospective study.
Conclusions
Our study shows that after adjustments of various potential confounders, there is no independent association between serum bilirubin levels and NAFLD in non-obese individuals. In the future, the causal relationship between bilirubin and NAFLD will be explored further through well-designed prospective studies and randomized controlled trials.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (No. 71964021); National Key R&D Program of China (Nos. 2016YFC1302201 and 2017YFC0908302); and the Fundamental Research Funds for the Central Universities (Nos. lzujbky-2021-ct17, lzujbky-2021-kb35).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1187/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-1187/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-1187/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Ethics Committee of the First Hospital of Lanzhou University approved of this study (approval No. LDYYLL2012001) and this study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and all participants gave written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84. [Crossref] [PubMed]
- Eslam M, Sanyal AJ, George J, et al. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020;158:1999-2014.e1. [Crossref] [PubMed]
- Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol 2013;10:686-90. [Crossref] [PubMed]
- Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol 2019;70:531-44. [Crossref] [PubMed]
- Shi Y, Wang Q, Sun Y, et al. The Prevalence of Lean/Nonobese Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. J Clin Gastroenterol 2020;54:378-87. [Crossref] [PubMed]
- Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol 2017;67:862-73. [Crossref] [PubMed]
- Younossi ZM, Stepanova M, Negro F, et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine (Baltimore) 2012;91:319-27. [Crossref] [PubMed]
- Xu C, Yu C, Ma H, et al. Prevalence and risk factors for the development of nonalcoholic fatty liver disease in a nonobese Chinese population: the Zhejiang Zhenhai Study. Am J Gastroenterol 2013;108:1299-304. [Crossref] [PubMed]
- Hagström H, Nasr P, Ekstedt M, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: A long-term follow-up study. Hepatol Commun 2018;2:48-57. [Crossref] [PubMed]
- Ong JP, Younossi ZM. Epidemiology and natural history of NAFLD and NASH. Clin Liver Dis 2007;11:1-16. vii. [Crossref] [PubMed]
- Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003;37:917-23. [Crossref] [PubMed]
- Hendrikx T, Binder CJ. Oxidation-Specific Epitopes in Non-Alcoholic Fatty Liver Disease. Front Endocrinol (Lausanne) 2020;11:607011. [Crossref] [PubMed]
- Shimasaki H, Saypil WH, Ueta N. Free radical-induced liver injury. II. Effects of intraperitoneally administered 2,2'-azobis(2-amidinopropane) dihydrochloride on the fatty acid profiles of hepatic triacylglycerol and phospholipids. Free Radic Res Commun 1991;14:247-52. [Crossref] [PubMed]
- Terao K, Niki E. Damage to biological tissues induced by radical initiator 2,2'-azobis(2-amidinopropane) dihydrochloride and its inhibition by chain-breaking antioxidants. J Free Radic Biol Med 1986;2:193-201. [Crossref] [PubMed]
- Baranano DE, Rao M, Ferris CD, et al. Biliverdin reductase: a major physiologic cytoprotectant. Proc Natl Acad Sci U S A 2002;99:16093-8. [Crossref] [PubMed]
- Neuzil J, Stocker R. Free and albumin-bound bilirubin are efficient co-antioxidants for alpha-tocopherol, inhibiting plasma and low density lipoprotein lipid peroxidation. J Biol Chem 1994;269:16712-9. [Crossref] [PubMed]
- Guzek M, Jakubowski Z, Bandosz P, et al. Inverse association of serum bilirubin with metabolic syndrome and insulin resistance in Polish population. Przegl Epidemiol 2012;66:495-501. [PubMed]
- Kunutsor SK, Bakker SJ, Gansevoort RT, et al. Circulating total bilirubin and risk of incident cardiovascular disease in the general population. Arterioscler Thromb Vasc Biol 2015;35:716-24. [Crossref] [PubMed]
- Kwon YJ, Lee YJ, Park BJ, et al. Total serum bilirubin and 8-year incident type 2 diabetes mellitus: The Korean Genome and Epidemiology Study. Diabetes Metab 2018;44:346-53. [Crossref] [PubMed]
- Kwak MS, Kim D, Chung GE, et al. Serum bilirubin levels are inversely associated with nonalcoholic fatty liver disease. Clin Mol Hepatol 2012;18:383-90. [Crossref] [PubMed]
- Bellarosa C, Bedogni G, Bianco A, et al. Association of Serum Bilirubin Level with Metabolic Syndrome and Non-Alcoholic Fatty Liver Disease: A Cross-Sectional Study of 1672 Obese Children. J Clin Med 2021;10:2812. [Crossref] [PubMed]
- Kim HJ, Kim HJ, Lee KE, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med 2004;164:2169-75. [Crossref] [PubMed]
- Ji R, Zhang Z, Zhang J, et al. Cohort Profile: A population-based cohort for the study of gastric cancer in northwest area of China (Wuwei Cohort). Int J Epidemiol 2021;50:1433-42. [Crossref] [PubMed]
- Fan JG, Jia JD, Li YM, et al. Guidelines for the diagnosis and management of nonalcoholic fatty liver disease: update 2010: (published in Chinese on Chinese Journal of Hepatology 2010; 18:163-166). J Dig Dis 2011;12:38-44. [Crossref] [PubMed]
- Farrell GC, Chitturi S, Lau GK, et al. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol 2007;22:775-7. [Crossref] [PubMed]
- Leung JC, Loong TC, Wei JL, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology 2017;65:54-64. [Crossref] [PubMed]
- Stefan N, Schick F, Häring HU. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab 2017;26:292-300. [Crossref] [PubMed]
- Wei JL, Leung JC, Loong TC, et al. Prevalence and Severity of Nonalcoholic Fatty Liver Disease in Non-Obese Patients: A Population Study Using Proton-Magnetic Resonance Spectroscopy. Am J Gastroenterol 2015;110:1306-14; quiz 1315. [Crossref] [PubMed]
- Phipps M, Wattacheril J. Non-alcoholic fatty liver disease (NAFLD) in non-obese individuals. Frontline Gastroenterol 2020;11:478-83. [Crossref] [PubMed]
- Sedlak TW, Saleh M, Higginson DS, et al. Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proc Natl Acad Sci U S A 2009;106:5171-6. [Crossref] [PubMed]
- Chang Y, Ryu S, Zhang Y, et al. A cohort study of serum bilirubin levels and incident non-alcoholic fatty liver disease in middle aged Korean workers. PLoS One 2012;7:e37241. [Crossref] [PubMed]
- Puri K, Nobili V, Melville K, et al. Serum bilirubin level is inversely associated with nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr 2013;57:114-8. [Crossref] [PubMed]
- Tian J, Zhong R, Liu C, et al. Association between bilirubin and risk of Non-Alcoholic Fatty Liver Disease based on a prospective cohort study. Sci Rep 2016;6:31006. [Crossref] [PubMed]
- Luo L, An P, Jia X, et al. Genetically Regulated Bilirubin and Risk of Non-alcoholic Fatty Liver Disease: A Mendelian Randomization Study. Front Genet 2018;9:662. [Crossref] [PubMed]
- Kunutsor SK, Frysz M, Verweij N, et al. Circulating total bilirubin and risk of non-alcoholic fatty liver disease in the PREVEND study: observational findings and a Mendelian randomization study. Eur J Epidemiol 2020;35:123-37. [Crossref] [PubMed]
(English Language Editor: B. Draper)


