Diagnostic performance of coronary computed tomography angiography-derived fractional flow reverse in lesion-specific ischemia patients with different Gensini score levels
Introduction
Coronary heart disease (CHD) caused by atherosclerosis is a leading cause of morbidity and mortality worldwide (1). Coronary angiography (CAG) is still the gold standard for the identification of obstructive CHD (2). However, more than one-third of patients with suspected CHD are reported as no CHD (defined as <20% stenosis in all vessels) using CAG (3). Therefore, a more precise assessment system should be explored in order to determine a more effective risk stratification of patients and enhance the yield of diagnostic CAG.
CAG can not only reveal the angiographic degree of coronary stenosis, but can also demonstrate the relevant ischemia by means of intracoronary pressure wire assessment, typically measuring fractional flow reverse (FFR), which defines the ratio of the mean coronary artery pressure distal to the stenosis and the mean pressure in the aorta (4). At present, coronary pressure-derived FFR is the standard of the functional assessment of lesion severity, especially in patients with intermediate-grade stenosis, those without evidence of ischemia in non-invasive testing, or in those with multi-vessel disease, and has been recommended by guidelines (5). In spite of its strengths in determining ischemia-related coronary stenosis, the invasive operation involved still limits its clinical application.
Recently, increasing evidence has indicated that coronary computed tomography angiography (CCTA) and CCTA-derived FFR or computed tomography-derived FFR (CT-FFR) were effective tools to evaluate lesion-specific ischemia (5). However, the data for both remains limited. Di Jiang et al. have reported that coronary calcification did not affect diagnostic performance of CT-FFR (6). Michail and his collogues also found that CT-FFR was feasible and valid in patients with severe aortic stenosis (7). Another study also affirmed its good diagnostic performance of CT-FFR in patients with or without diabetes mellitus (8). Therefore, the diagnostic performance of CT-FFR in patients with different severities of coronary stenosis has not been reported, which restricted its clinical use to a certain extent. The present study aims to investigate the diagnostic performance of CCTA-derived FFR, and explore whether it is consistent in patients with different severities of coronary stenosis. The current research attempted to provide the foundation for extensive clinical application of CCTA-FFR. We present the following article in accordance with the STARD reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-881/rc).
Methods
Study population
A protocol was prepared before the study with registration (ID: ChiCTR1900026971). The design of the present study was a diagnostic test. From December 2019 to April 2021, a total of 36 vessels from 35 patients diagnosed by selective CAG participated in this study at the Cardiology Department of Shaanxi Provincial People’s Hospital. Furthermore, 61 vessels from 56 patients obtained from West China Hospital of Sichuan University between July 2020 and April 2021 were also included. The inclusion criteria were as follows: (I) patients aged between 18 and 80; (II) patients who were able to understand the purpose of the study and signed the informed consent voluntarily; (III) patients who were suspected of having coronary artery stenosis and planned to have selective CAG; (IV) patients who underwent coronary computed tomography angiography (CTA) using CT scanners with ≥64-row detectors; (V) clear and readable coronary CTA images; (VI) cases in which the degree of coronary artery stenosis was probably between 30% and 90% through coronary CTA; and (VII) the diameter of target vessel was greater than 2 mm through coronary CTA.
The exclusion criteria were as follows: (I) women who were pregnant, breastfeeding, or planning pregnancy; (II) patients with a history of myocardial infraction in the last 30 days prior to coronary CTA; (III) those who had previously undergone coronary artery bypass surgery or stenting, or had installed pacemakers, implantable cardioverter defibrillators, or artificial heart valves; (IV) patients with a history of allergies to contrast media; (V) those with hypertrophic obstructive cardiomyopathy or severe heart failure [New York Heart Association (NYHA) ≥ Ⅲ]; (VI) body mass index >35 kg/m2; (VII) serum creatinine >178 µmol/L; (VIII) cases of non-diagnostic quality of CTA data; (IX) cases of chronic total occlusion; (X) cases of aneurysm or myocardial bridge involvement; (XI) an unqualified pressure curve for FFR analysis; and (XII) other circumstances that were not suitable for participating in the experiment.
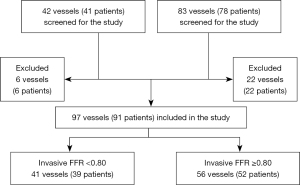
The flowchart of the analysis is presented in Figure 1. This study complied with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Shaanxi Provincial People’s Hospital, Xi’an, Shaanxi, China (No. 2019X005) and West China Hospital, Chengdu, Sichuan, China (No. 20202). Written informed consent was obtained from all study participants.
Data collection
The collected data included patients’ demographics, medical history, vital signs, and results of laboratory testing at admission. Body mass index was calculated by dividing weight in kilograms by the square of height in meters. The CTA and CAG procedures, and the obtainment of CT-FFR and FFR have been published previously (9). Briefly, CT-FFR measurement was computed using a commercial software program (CAscope, EScope Ltd.), which adopted a deep learning method for vessel model creation from CCTA images. The patients’ brachial artery diastolic (mmHg) and systolic (mmHg) blood pressure, as well as heart rate (bpm) measured before CCTA were used as inputs for CT-FFR calculation. The representative analysis of CT-FFR is illustrated in Figure 2. The vessel characteristics were also acquired during CAG. The Gensini score was calculated as described in the literature (10).

Statistical analysis
Continuous variables were presented as the mean ± standard deviation (SD) or median [lower quartile, upper quartile]. The Kolmogorov-Smirnov test was used to assess the normality of continuous variables distribution. Categorical variables were presented as frequencies (percentages). FFR was indicated as the golden diagnosis of lesion-specific ischemia with a cut-off value of 0.80, which was consistent with most contemporary studies. The diagnostic performance of CT-FFR was determined using the receiver-operating characteristic (ROC) curve. It was acceptable that if the area under the curve (AUC) was more than 0.70. Sensitivity and specificity of CT-FFR were also calculated. Simple linear analysis was performed by calculating the correlation between CT-FFR and FFR. The systematic difference between CT-FFR and FFR was represented using a Bland-Altman plot. As for the diagnostic performance on a per patient basis, the lowest values of FFR and CT-FFR were used in patients rather than one vessel (7). The Z test was performed to compare the diagnostic performance of CT-FFR in patients with low and high Gensini scores.
Results
Clinical and vessel characteristics of the study population
A total of 91 patients were included in this analysis. Patient characteristics are presented in Table 1; 64.8% were males and the mean age was 63 years. Physical examinations, past medical history, and laboratory tests are also shown in the Table 1. A total of 97 vessels were analyzed in our study, and the vessel characteristics are listed in the Table 2. As for the target vessel, approximately two-thirds of the vessels were left anterior descending coronary arteries, and a quarter was right coronary arteries. More than half of the plaque was combined plaque. As for severity, nearly half of the vessels had 50–69% stenosis, and 30–49% and 70–90% stenosis also accounted for a certain percentage (29% and 23% separately).
Table 1
| Characteristics | Values |
|---|---|
| Male, % | 59 (64.8) |
| Age, years | 62.95±9.35 |
| Body mass index, kg/m2 | 24.75±3.05 |
| Heart rate, bpm | 71 [64, 82] |
| Systolic blood pressure, mmHg | 126 [118, 138] |
| Diastolic blood pressure, mmHg | 78.14±11.05 |
| Past medical history | |
| Diabetes mellitus, % | 22 (24.2) |
| Hypertension, % | 45 (49.5) |
| Hyperlipidemia, % | 22 (24.2) |
| Peripheral vascular disease, % | 8 (8.8) |
| Stroke, % | 8 (8.8) |
| Smoking, % | 19 (20.9) |
| Laboratory test | |
| White blood cell, 109/L | 6.13 [5.43, 7.08] |
| Red blood cell, 1012/L | 4.31 [4.08, 4.85] |
| Platelet, 109/L | 192.85±65.14 |
| Hemoglobin, g/L | 136.05±16.64 |
| Serum creatinine, μmol/L | 73.87±17.99 |
| Blood urea nitrogen, mmol/L | 5.72±1.49 |
| Alanine aminotransferase, U/L | 21 [13, 29] |
| Aspartate aminotransferase, U/L | 22 [18, 27] |
Table 2
| Characteristics | No. (%) |
|---|---|
| Target vessel | |
| Left anterior descending coronary artery | 65 (67.0) |
| Right coronary artery | 23 (23.7) |
| Left coronary circumflexus artery | 7 (7.2) |
| Left main coronary artery | 2 (2.1) |
| Plaque | |
| Combined plaque | 49 (50.5) |
| Non-calcified plaque | 33 (34.0) |
| Calcified plaque | 15 (15.5) |
| Severity | |
| 30–49% | 29 (29.9) |
| 50–69% | 45 (46.4) |
| 70–90% | 23 (23.7) |
Diagnostic accuracy of CT-FFR compared with FFR
Consistent with most contemporary studies, we used an FFR cut-off of 0.80, and the following analysis was performed at the per-vessel level (5). Table 3 shows CT-FFR in relation to FFR and the sensitivity was 94.6% and the specificity was 95.1%. As shown in Figure 3, CT-FFR was well correlated with invasive FFR (R2=0.745, P<0.001) and the AUC was 0.976. Further analysis of the systematic difference was performed, which indicated that the mean difference between FFR and CT-FFR was 0.011, and the 95% confidence interval was −0.173 to 0.196 (Figure 4).
Table 3
| CT-FFR | FFR | Total | |
|---|---|---|---|
| Positive | Negative | ||
| Positive | 53 | 2 | 55 |
| Negative | 3 | 39 | 42 |
| Total | 56 | 41 | 97 |
CT-FFR, computed tomography-derived fractional flow reverse. FFR, fractional flow reverse.


Diagnostic performance of CT-FFR in different degrees of coronary stenosis
We utilized the Gensini score as an evaluation method of the severity of coronary stenosis. According to the median scores, all participants were divided into a low Gensini group (Gensini score: 1.5–21, n=48) and a high Gensini group (Gensini score: 21.5–99.5, n=43). Subsequent analysis was performed at the per-patient level and the results are shown in Figure 5. Firstly, the AUCs were 0.989 and 0.928 in low and high Gensini groups, respectively. However, there was no significant difference in the diagnostic accuracies between these two groups (Z=0.003, P>0.500). Secondly, CT-FFR still exhibited a good correlation with FFR (R2=0.713, P<0.001 in the low Gensini group and R2=0.743, P<0.001 in the high Gensini group). Thirdly, the systematic differences were calculated, and the mean difference between FFR and CT-FFR was −0.005 and 0.025, respectively, in these two groups.

Discussion
Although CT-FFR has been indicated as an effective index to assess lesion-specific ischemia, relevant research remains limited at present. Our current study focused on the diagnostic performance of CT-FFR and found that CT-FFR had a good diagnostic accuracy compared with FFR, which was maintained in the subgroup analysis of different degrees of coronary stenosis. To the best of our knowledge, our study is the first analysis of the diagnostic performance of CT-FFR in patients with different Gensini score levels.
DISCOVER-FLOW is the first multi-center clinical trial to evaluate the diagnostic value of CT-FFR. It included 103 patients suspected with complete CHD, and the results showed that the diagnostic performance of CT-FFR in coronary stenosis was better than CCTA, especially in terms of specificity (CT-FFR: 82.2% vs. CCTA: 39.6%). Furthermore, there was a strong correlation between CT-FFR and invasive FFR (r=0.678, P<0.001), which indicated that CCTA-derived non-invasive FFR was an effective method with high diagnostic performance for the detection and exclusion of ischemia-causing coronary lesions (11). Multiple subsequent studies also confirmed similar conclusions. Several studies have shown that CT-FFR is a useful method to recognize hemodynamically-significant CHD (12-16). Rasoul et al. also suggested that CT-FFR could preliminarily screen patients for CAG (17-19). Other researchers also reported that CT-FFR improved the diagnostic performance of CTA (20-26). In the current study, we also showed (using a ROC curve) that CT-FFR was an excellent tool to evaluate ischemia-causing coronary stenosis compared with invasive FFR. In addition, we observed a good correlation between non-invasive CT-FFR and invasive FFR through simple linear analysis and the Bland-Altman plot. These results were consistent with previous research.
Recent studies have increasingly been paying attention to the diagnostic value of CT-FFR in different kinds of coronary stenosis (7,27). The aim of the DeFACTO study was to focus on the diagnostic performance of CT-FFR for lesions of intermediate stenosis severity and draw a consistent conclusion. Nevertheless, the researchers suggested that CT-FFR might serve as an excluded index for ischemia due to its high sensitivity and negative predictive value (27). However, the severity of CHD is amazingly varied, regardless of whether it is measured at the per-vessel or per-patient levels, and whether the diagnostic performance of CT-FFR is still high in different degrees of coronary stenosis has not been reported. In our present study, we calculated the Gensini score for each patient according to CAG and divided them into two groups on the basis of the median Gensini score. Statistical analyses were performed in the low and high Gensini groups, respectively, and the results revealed that CT-FFR showed eminent diagnostic performance in both the low and high Gensini score groups, and there was no statistical difference between them.
The current study has several limitations that should be noted. Firstly, the sample size was relatively small, and thus, the results still need to be confirmed in a larger sample size study. Secondly, the Gensini score was the only metric used to evaluate the severity of coronary stenosis. Subsequent studies could determine the diagnostic performance of CT-FFR in varied severity of CHD according to other scoring systems, such as the Syntax score. Thirdly, we only investigated the diagnostic performance of CT-FFR in different levels of CHD. Long-term follow-up could determine the prognostic value of CT-FFR in CHD and guide clinical decision-making.
In conclusion, CT-FFR showed good prognostic performance in patients with different Gensini score levels. CT-FFR is an excellent non-invasive index to evaluate coronary ischemia, regardless of the severity of stenosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-881/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-881/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-881/coif). QZ and YL report that they are from Beijing Escope Tech Co., Ltd. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study complied with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Shaanxi Provincial People’s Hospital, Xi’an, Shaanxi, China (No. 2019X005) and West China Hospital, Chengdu, Sichuan, China (No. 20202). Written informed consent was obtained from all study participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020;141:e139-596. [Crossref] [PubMed]
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Thorac Cardiovasc Surg 2015;149:e5-23. [Crossref] [PubMed]
- Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med 2010;362:886-95. [Crossref] [PubMed]
- Gaede L, Möllmann H, Rudolph T, et al. Coronary Angiography With Pressure Wire and Fractional Flow Reserve. Dtsch Arztebl Int 2019;116:205-11. [Crossref] [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165. [Crossref] [PubMed]
- Di Jiang M, Zhang XL, Liu H, et al. The effect of coronary calcification on diagnostic performance of machine learning-based CT-FFR: a Chinese multicenter study. Eur Radiol 2021;31:1482-93. [Crossref] [PubMed]
- Michail M, Ihdayhid AR, Comella A, et al. Feasibility and Validity of Computed Tomography-Derived Fractional Flow Reserve in Patients With Severe Aortic Stenosis: The CAST-FFR Study. Circ Cardiovasc Interv 2021;14:e009586. [Crossref] [PubMed]
- Nous FMA, Coenen A, Boersma E, et al. Comparison of the Diagnostic Performance of Coronary Computed Tomography Angiography-Derived Fractional Flow Reserve in Patients With Versus Without Diabetes Mellitus (from the MACHINE Consortium). Am J Cardiol 2019;123:537-43. [Crossref] [PubMed]
- Li Q, Zhang Y, Wang C, et al. Diagnostic performance of CT-derived resting distal to aortic pressure ratio (resting Pd/Pa) vs. CT-derived fractional flow reserve (CT-FFR) in coronary lesion severity assessment. Ann Transl Med 2021;9:1390. [Crossref] [PubMed]
- Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 1983;51:606. [Crossref] [PubMed]
- Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:1989-97. [Crossref] [PubMed]
- Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145-55. [Crossref] [PubMed]
- Kurata A, Fukuyama N, Hirai K, et al. On-Site Computed Tomography-Derived Fractional Flow Reserve Using a Machine-Learning Algorithm - Clinical Effectiveness in a Retrospective Multicenter Cohort. Circ J 2019;83:1563-71. [Crossref] [PubMed]
- Tang CX, Wang YN, Zhou F, et al. Diagnostic performance of fractional flow reserve derived from coronary CT angiography for detection of lesion-specific ischemia: A multi-center study and meta-analysis. Eur J Radiol 2019;116:90-7. [Crossref] [PubMed]
- Chung JH, Lee KE, Nam CW, et al. Diagnostic Performance of a Novel Method for Fractional Flow Reserve Computed from Noninvasive Computed Tomography Angiography (NOVEL-FLOW Study). Am J Cardiol 2017;120:362-8. [Crossref] [PubMed]
- Ihdayhid AR, Sakaguchi T, Linde JJ, et al. Performance of computed tomography-derived fractional flow reserve using reduced-order modelling and static computed tomography stress myocardial perfusion imaging for detection of haemodynamically significant coronary stenosis. Eur Heart J Cardiovasc Imaging 2018;19:1234-43. [Crossref] [PubMed]
- Rasoul H, Fyyaz S, Noakes D, et al. NHS England-funded CT fractional flow reserve in the era of the ISCHEMIA trial. Clin Med (Lond) 2021;21:90-5. [Crossref] [PubMed]
- Khattak MF, Horne S. Retraction: The Use of CT Coronary Angiography and CT Fractional Flow Reserve in the Investigation of Patients With Suspected Coronary Artery Disease. Cureus 2020;12:r19. [PubMed]
- Tesche C, Vliegenthart R, Duguay TM, et al. Coronary Computed Tomographic Angiography-Derived Fractional Flow Reserve for Therapeutic Decision Making. Am J Cardiol 2017;120:2121-7. [Crossref] [PubMed]
- Kapoor A, Mahajan G, Kapoor A. Onsite Computed Tomography Fractional Flow Reserve in Patients with Suspected Stable Coronary Artery Disease Initial Experience. Indian J Radiol Imaging 2021;31:291-6. [Crossref] [PubMed]
- Miyajima K, Motoyama S, Sarai M, et al. On-site assessment of computed tomography-derived fractional flow reserve in comparison with myocardial perfusion imaging and invasive fractional flow reserve. Heart Vessels 2020;35:1331-40. [Crossref] [PubMed]
- Nous FMA, Budde RPJ, Lubbers MM, et al. Impact of machine-learning CT-derived fractional flow reserve for the diagnosis and management of coronary artery disease in the randomized CRESCENT trials. Eur Radiol 2020;30:3692-701. [Crossref] [PubMed]
- Kawasaki T, Kidoh M, Kido T, et al. Evaluation of Significant Coronary Artery Disease Based on CT Fractional Flow Reserve and Plaque Characteristics Using Random Forest Analysis in Machine Learning. Acad Radiol 2020;27:1700-8. [Crossref] [PubMed]
- Guo W, Lin Y, Taniguchi A, et al. Prospective comparison of integrated on-site CT-fractional flow reserve and static CT perfusion with coronary CT angiography for detection of flow-limiting coronary stenosis. Eur Radiol 2021;31:5096-105. [Crossref] [PubMed]
- Li Y, Qiu H, Hou Z, et al. Additional value of deep learning computed tomographic angiography-based fractional flow reserve in detecting coronary stenosis and predicting outcomes. Acta Radiol 2022;63:133-40. [Crossref] [PubMed]
- Wang R, Renker M, Schoepf UJ, et al. Diagnostic value of quantitative stenosis predictors with coronary CT angiography compared to invasive fractional flow reserve. Eur J Radiol 2015;84:1509-15. [Crossref] [PubMed]
- Nakazato R, Park HB, Berman DS, et al. Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity: results from the DeFACTO study. Circ Cardiovasc Imaging 2013;6:881-9. [Crossref] [PubMed]
(English Language Editor: A. Kassem)