Nonintubated bilateral single port thoracoscopic sympathectomy in the context of an outpatient program, the least invasive management for hyperhidrosis surgery
Primary hyperhidrosis (PH) is an idiopathic condition characterized by abnormally increased sweating. Surgery remains the mainstay of treatment when there is no response to conservative therapies. Conventionally, thoracoscopic sympathectomy is performed routinely under general anesthesia with endotracheal intubation. However, this management leads inherently to several anesthesia risks and possible postoperative complications. Here we propose a novel and less invasive surgical management of patients with PH, a nonintubated bilateral single port thoracoscopic sympathectomy in the context of an outpatient program.
Technique
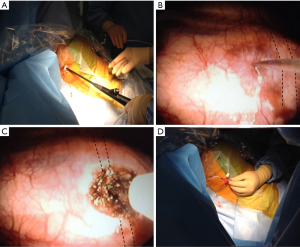
A 42-year-old woman was referred to our Department for evaluation of palmar hyperhidrosis. Once the preoperative evaluation was completed, the patient underwent surgery. Following standard monitorization, including a temperature sensor in both hands in order to check the temperature rise after sympathectomy, the patient was placed in a semi-Fowler’s position with both arms abducted (Figure 1). The goal of ventilation was to establish a relaxed spontaneous breathing with a respiratory rate of 12 to 20 breaths per minute. Oxygenation was facilitated with O2 supplement by Venturi mask 3–4 L/min. Sedation was induced by intravenous administration of midazolam (2 mg) and remifentanil (0.03–0.05 µg/kg/min), as well as Propofol (0.5–1.5 mg/kg/h) using a target-controlled infusion system. We started on the right side. After infiltration of local anesthesia (LA), an 8-mm. skin incision was performed at the level of the third intercostal space in the anterior axillary line. Then, we placed a flexible trocar and an open pneumothorax was created. Air injection help to accelerate the lung collapse. Furthermore, gravity leads to the lung to fall downwards and exposes better the upper posterior chest wall. CO2 insufflation was not used at any time. When the lung was deflated sufficiently, we introduced a semirigid pleuroscopy (LTF-160, Olympus) into the pleural cavity (Figure 2A). Once the T3 level was identified, we inserted an injection needle (MAJ-75, Olympus) through the working channel of the pleuroscopy and we infiltrated 3 mL of LA into both sides of the sympathetic chain (Figure 2B). Then, we incised the parietal pleura and cut the chain with electrocautery (KD-31C-1.B, Olympus) (Figure 2C). The depth of the ablation must reach the rib periosteum. The nerve bundle of Kuntz must also be divided to avoid recurrence. After a proper hemostasis, we placed a chest tube connected to a Pleur-evac system with mild suction (Figure 2D) and we ask the patient to deep breathe. We must ensure that the lung is fully re-expanded before approaching the opposite side. The anesthesiologist could ventilate the patient manually if it was necessary. Thereby, the presence of postoperative pneumothorax is prevented. Finally the same procedure was then repeated on the left side. The total surgical time was 88 min, including anesthesia time. The patient reported feeling calm and relaxed during the surgery.
Once in the recovery room, a chest X-ray was done prior to tubes removal. Postoperative course was uneventful and the patient was discharged 6 h later. An outpatient follow-up confirmed that her hands remained dry.
Discussion
The interruption of the thoracic sympathetic chain has proven to be a safe, accurate and useful technique. Commonly, thoracoscopic sympathectomy is performed under general anesthesia with double or single lumen intubation. According to our philosophy, sympathectomy is a minor procedure that should be less and less invasive. Nonintubated thoracoscopic sympathectomy offers several advantages over the traditional technique such as:
- Minimally invasive anesthesia. Nonintubated surgery avoids possible adverse complications following intubated general anesthesia such as intubation-related airway trauma, ventilation-induced lung injury, residual neuromuscular blockade… (1).
- Outpatient program: only a few studies have analyzed the feasibility of outpatient programs in hyperhidrosis surgery (2). Maybe this technique may encourage surgeons to implement these programs.
- Economic benefits: cheaper anesthetic management, lower requirements of antiemetics and analgesic drugs, less over-all complication rates and shorter hospitalization stay.
Over time, nonintubated video-assisted thoracoscopic surgery has become a globally accepted surgical approach for a variety of thoracic diseases. However, thoracoscopic sympathectomy under sedation without intubation has not yet been widely used. On August 2005, Elia et al. (3) reported the first cases of two-ports awake bilateral thoracoscopic sympathectomy performed as an outpatient procedure. Five years later, Jeong et al. (4) completed three cases of two-port thoracoscopic sympathectomy under LA without intubation and CO2 insufflation. By contrast, we place the patient in semi-upright position, instead of semi-prone or prone position, and we prefer a uniportal approach. These changes lead to decrease the surgical time and a minor surgical invasion. Recently, Tang et al. (5) demonstrated that thoracic sympathectomy under deep sedation without intubation is a safe and effective method. In this case, our surgical technique is very similar to that used by the Chinese team, although they did not implement an outpatient surgery program. So after reading carefully these three publications, we took the best of each and we developed this novel management. Surgical time is expected to decrease notably as we gain experience.
We have to take into account several risks of operating on non-intubated patients, such as losing the airway, aspiration, the need for emergent intubation if the surgery is not going well, etc. Despite the novelty of this technique, further studies are needed to promote this kind of perioperative management.
Conclusions
Nonintubated bilateral single port thoracoscopic sympathectomy is a safe, effective, cost-efficient and minimally invasive technique that could reduce certain anesthesia risks.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Molins L, Fibla JJ, Pérez J, et al. Outpatient thoracic surgical programme in 300 patients: clinical results and economic impact. Eur J Cardiothorac Surg 2006;29:271-5. [PubMed]
- Elia S, Guggino G, Mineo D, et al. Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 2005;28:312-7; discussion 317. [PubMed]
- Jeong JY, Park HJ. Sympathicotomy under local anesthesia: a simple way to treat primary hyperhidrosis. Ann Thorac Surg 2010;90:1730-1. [PubMed]
- Tang H, Wu B, Xu Z, et al. A new surgical procedure for palmar hyperhidrosis: is it possible to perform endoscopic sympathectomy under deep sedation without intubation? Eur J Cardiothorac Surg 2014;46:286-90; discussion 290. [PubMed]



