Percutaneously assisted total hip (PATH) and Supercapsular percutaneously assisted total hip (SuperPATH) arthroplasty: learning curves and early outcomes
Introduction
A number of minimally invasive surgical (MIS) total hip arthroplasty (THA) approaches have been proposed: the mini-anterior, the mini-posterior, the mini-lateral, and the two-incision technique (1-4). However, as underlined by Chow et al. (5), these MIS techniques have their respective shortcomings, such as increased overall complication rates, extended learning curves, periprosthetic fracture, increased peri-operative blood loss, component malposition, and inability to extend the approach (6-13).
In an attempt to overcome these shortcomings, a new family of micro-posterior approaches has been developed, including the percutaneously-assisted total hip (PATH) (MicroPort—Arlington, TN) approach developed by Dr. Penenberg (14), the SuperCapsular (SuperCap) (MicroPort—Arlington, TN) approach developed by Dr. Stephen Murphy (15), and the Supercapsular Percutaneously-Assisted Total Hip (SuperPATH) (MicroPort—Arlington, TN) approach developed by Dr. Chow (5), which combines elements of the PATH and SuperCap approaches. The micro-posterior family of approaches distinguishes itself from the mini-posterior approach by sparing most or all of the external rotators. In theory, these soft tissue-sparing approaches should decrease soft tissue trauma, accelerate recovery, and decrease dislocation rates. Specialized instrumentation is required, but these approaches can be performed on a standard operating room table and are easily extendable to a more conventional posterolateral approach if necessary.
Encouraging results suggest that most of the limitations of MIS THA approaches can be overcome (5,14-16). The primary objective of this study was to assess the early outcomes of two of the micro-posterior approaches (PATH and SuperPATH) when performed by a non-developer surgeon. A secondary objective was to evaluate the learning curve associated with the PATH and SuperPATH approaches in order to assess whether the outcomes reported in the literature are likely to be reproducible by surgeons incorporating these innovative techniques into their own practice.
Methods
Ethics approval was obtained from the Ottawa Hospital Research Ethics Board for a single-centre retrospective chart review. Our study involved a single non-developer surgeon (W.G.) and two patient cohorts, representing a total of 99 primary total hips at a single training institution. The first cohort (PATH) was composed of our first 50 consecutive PATH cases performed between 2009 and 2011 (one patient who presented with a hip fracture was excluded). The second cohort (SuperPATH) was composed of our first 50 consecutive SuperPATH cases performed between 2013 and 2014.
W.G. possesses a fellowship in trauma and lower extremity reconstruction. He had 4 years of experience performing primary THA exclusively through a Hardinge approach and had experience with the posterior approach for trauma and revision THA. He performs approximately 250 joint replacements per year, of which 50% are THA.
All patients included in this study presented with a diagnosis of degenerative hip arthritis, had failed non-operative therapy, and were candidates for total hip replacement. Patients were excluded from the study if they presented with a femoral neck fracture, severe acetabular defect likely to require grafting or augmentation, metastatic disease, or if they had undergone simultaneous bilateral procedures.
Patient characteristics were collected to determine whether the two cohorts were comparable at baseline. Analysis of variance (ANOVA) was used to compare age, body mass index (BMI), and pre-operative hemoglobin. Gender was compared using a Chi-square test. Clinical outcomes, including operative time and length of stay (LOS), were compared using a nonparametric Wilcoxon test. Disposition, use of tranexamic acid, and need for post-operative blood transfusion were compared using a Chi-square test. Acetabular cup abduction and anteversion were evaluated using the first post-operative AP pelvis and a modified protractor developed by Liaw et al. (17).
The learning curves for the PATH and SuperPATH cohorts were assessed using operative time as a surrogate. These cohorts were subdivided into groups of five consecutive cases. Mean operative time for each subgroup was calculated and compared using the correlation coefficient to determine whether operative time decreased as the surgeon gained experience with the technique.
Results
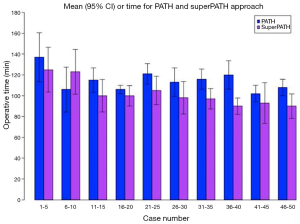
Mean follow-up time in months was recorded for the PATH (24.7) and SuperPATH (7.9) cohorts. No significant difference was identified between the two cohorts in terms of age, gender, BMI or pre-operative hemoglobin (Table 1). Mean operative time in minutes was recorded for the PATH (114.5±17.5) and SuperPATH (101.7±18.3) cohorts (P value =0.0002). The correlation coefficient for the SuperPATH cohort was significant (−0.467; P value <0.001). The coefficient for the PATH cohort was found to be non-significant (−0.0246; P value=0.088).
A greater percentage of patients in the SuperPATH (92.0%) cohort received tranexamic acid when compared to the PATH (40.8%) cohort. However, this difference was not statistically significant. The difference in post-operative blood transfusion was documented for the PATH (6.1%) and SuperPATH (4.0%) cohorts. This difference was also non-significant.
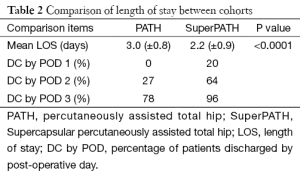
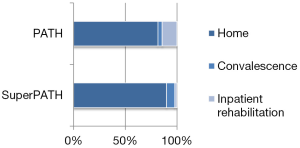
Mean LOS in days was significantly shorter in the SuperPATH (2.2±0.9) cohort compared to the PATH (3.0±0.8) cohort (P value <0.0001). Discharge rates are also presented in Table 2. In the PATH cohort, patients were discharged home (81.6%), to short term rehabilitation (STR) (14.3%), or to plan convalescence (4.1%). In the SuperPATH cohort, post-operative disposition was home (90%), STR (2%), or planned convalescence (8%), as seen in Figure 1. There was no statistically significant difference in disposition between the two cohorts. Mean LOS in STR was calculated for the PATH (10.6±3.1) cohort. Mean LOS in STR following a SuperPATH approach could not be calculated as only one patient attended STR (7 days) in the SuperPATH cohort.
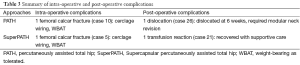
Overall complication rates were reported for the PATH (4.1%) and SuperPATH (4.0%) cohorts (Table 3). In the SuperPATH cohort, one patient (case 5) suffered an intra-operative femoral calcar fracture. This was treated with extension of the skin incision, piriformis release, and cerclage wiring. Post-operatively, weight-bearing was permitted without incident. Another patient (case 21) returned to hospital following discharge complaining of fatigue. The patient was found to be anemic (hemoglobin 74 g/L) and received a blood transfusion. Subsequently, this patient developed an acute hemolytic transfusion reaction, but recovered with supportive measures. In the PATH cohort, one patient (case 10) suffered an intra-operative fracture of the femoral calcar; it was identified at the time of surgery and treated with extension of the skin incision and cerclage wiring. Post-operatively, weight-bearing was permitted without incident. One patient (case 26) suffered a spontaneous dislocation 6 weeks post-operatively due to poor compliance. This was managed with revision of the modular neck component and soft tissue capsular repair; there has been no recurrence.
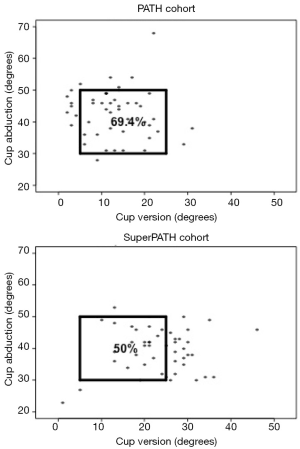
For the PATH cohort, mean acetabular cup anteversion and abduction were 13.1°±7.1° and 42.9°±7.6°, respectively. For the SuperPATH cohort, mean acetabular cup anteversion and abduction were 23.5°±8.2° and 39.0°±8.4°, respectively. Acetabular cups in the SuperPATH cohort were significantly more anteverted (P value <0.0001) and less abducted (P value <0.05) than in the PATH cohort.
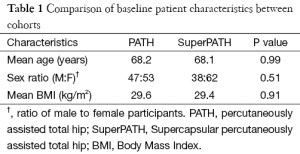
Full table.
Full table.
Full table.
Discussion
Recent publications suggest that the micro-posterior family of tissue-sparing THA approaches is associated with a low dislocation rate, low overall complication rate, decreased peri-operative blood loss, and decreased LOS (5,14-16). While these results are promising, we have yet to see an independent confirmation of surgical outcomes or an assessment of the surgical learning curve associated with the micro-posterior family of approaches. In this study, we sought to provide a report of an independent surgeon’s early experience with the PATH and SuperPATH techniques. Our results suggest that a surgeon adopting these techniques may expect a significant reduction in LOS without an increase in complications. Anecdotally, we also noted a reduction in post-operative pain and earlier mobilization. Our data supports the results presented by the surgical innovators and suggests that the SuperPATH and PATH techniques can be safely incorporated into a surgeon’s practice.
Mean LOS was only 3 days in the PATH cohort with the large majority of patients being discharged directly home (81.6%). Mean LOS in the SuperPATH cohort was even shorter (2.2 days), with only one patient requiring post-operative inpatient rehabilitation (STR). In the SuperPATH cohort, 20% of patients were discharged by POD 1, 64% by POD 2, and 96% by POD 3. Moreover, our current LOS is less than 2 days, which suggests that LOS for the PATH and SuperPATH approaches may be even less than presently reported. Both micro-posterior approaches appear to significantly reduce LOS when compared to traditional approaches, and could therefore reduce hospital stay and expenses.
The post-operative transfusion rate for both the PATH (6%) and SuperPATH (4%) cohorts were found to be equal or lower than the provincial average (6-7.4%) in Ontario at that time (personal communication from TOH blood conservation program collected through ONTraC, December 22, 2014). The lower transfusion rates for the PATH and SuperPATH techniques suggest that soft-tissue sparing approaches may also minimize blood loss and post-operative transfusions. Further studies are required to confirm this finding.
It is generally accepted that a surgeon adopting a new technique will experience an increase in operative time, which then decreases as the surgeon gains experience (18,19). In this study, operative time was used as a surrogate to estimate the learning curve for the PATH (learned first) and SuperPATH (learned second) approaches (Figure 2) (20). W Gofton’s learning curves for the PATH and SuperPATH approaches were found to be significantly different (P value <0.001). By the 40th case, operative time for the PATH cohort had reached a plateau. In contrast, operative time in the SuperPATH cohort was still significantly decreasing by the 50th case (P value <0.001), suggesting that proficiency continues to improve beyond the first 50 cases. This finding was unanticipated, as we had predicted that the SuperPATH technique would be associated with a shorter learning curve given that it was learned after the PATH technique, which utilizes many of the same instruments for acetabular preparation. This suggests that the SuperPATH approach may be associated with subtle learning cues that require extensive experience with the procedure. In an attempt to modify the learning curve to their advantage, a surgeon adopting one of these micro-posterior approaches may benefit from a site visit with an expert or expert mentorship at various points during the learning curve. Following a site visit, our results indicate that a temporary increase in operative time can be expected while the surgeon refines and incorporates newly acquired skills. As seen in Figure 2, operative time temporarily increased shortly after W.G. completed site visits, which occurred after the 12th PATH case and the 15th SuperPATH case.
It is important to note that a longer learning curve does not necessarily correlate with increased operative time. In fact, despite the longer learning curve, mean operative time for the SuperPATH approach (101.7 min) only exceeded the mean operative time for a traditional Hardinge approach by 8.5 min, and this was despite the addition of intra-operative imaging to confirm implant position. With further experience and the elimination of intra-operative imaging, the percutaneous nature of the approach may allow for a further reduction in operative time. This is especially true in large patients where time dedicated to exposure and closure may be significantly reduced.
This study demonstrates that incorporation of the PATH and SuperPATH approaches into a surgeon’s practice does not negatively impact early clinical outcomes, even during the learning curve. Both the PATH (4.1%) and SuperPATH (4.0%) techniques were associated with low complication rates. The two intra-operative complications in the SuperPATH and PATH cohorts occurred relatively early in the learning curve, and none occurred after a site visit with an expert in the procedure. The significance of this finding is undetermined, but we recommend an early site visit with an expert to decrease the risk of intra-operative complications. A post-operative dislocation at 6 weeks in the PATH group was the only other surgical complication. The dislocation was not attributed to acetabular cup alignment (anteversion 8°; abduction 45°). The patient had a diagnosis of rheumatoid arthritis, treated with prednisone, and was non-compliant with post-operative restrictions. Of note, no superficial or deep infections were identified in the SuperPATH or PATH cohorts. This finding is echoed by a recent multicenter study by Gofton et al. (16), suggesting that percutaneous approaches may decrease infection rates.
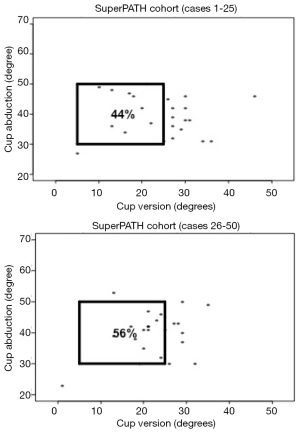
Radiographic outcomes, such as acetabular cup anteversion and abduction, may also be subject to a learning curve. Prior to the adoption of the PATH and SuperPATH approaches, the surgeon aimed for 45° of abduction and 10° to 15° of anteversion. With conversion to the PATH and SuperPATH approaches, Surgeon X aimed for an abduction angle less than 45° and anteversion of 15° to 20°. We identified the proportion of cups implanted within the safe zone described by Lewinnek et al. for the PATH (69.4%) and SuperPATH (50.0%) cohorts (Figure 3). This safe zone, which has been shown to be associated with a lower post-operative dislocation rate, is defined by cup anteversion of 5° to 25° and abduction of 30° to 50° (21). Although these results appear to suggest that cup position was rather homogeneous between these cohorts, cups in the SuperPATH cohort were significantly more anteverted (23.5°) and significantly less abducted (39.0°) than cups in the PATH cohort (13.1° and 42.9°, respectively). This unexpected finding was identified following a preliminary review of the first 25 SuperPATH cases. The main concern was that excessive anteversion may lead to an increased risk of post-operative dislocation. Therefore, from cases 26-50, the surgeon relied more on the transverse acetabular ligament to determine version (22), which is easily visualized during the approach. As seen in Figure 4, the effect of this modification was assessed by comparing the proportion of cups that were implanted within the safe zone in SuperPATH cases 1-25 (44.0%) and cases 26-50 (56.0%). Although encouraging, this trend towards improved cup alignment was not statistically significant. Nevertheless, our early results (7.9 months) do not demonstrate any association between increased anteversion and dislocation. Similarly, Penenberg et al. reported a mean anteversion of 31° (range, 22° to 40°) in their series of 250 PATH cases with no early post-operative dislocations (14). We speculate that reduced soft-tissue damage reduces the likelihood of dislocation secondary to increased anteversion, but further studies are required. Currently, we recommend that a surgeon adopting the SuperPATH approach utilize the transverse acetabular ligament as a guide to determine version and review radiographic parameters during the learning curve to ensure optimal cup alignment.
Limitations of this study include the lack of randomization. However, randomization may have inappropriately lengthened the learning curve by increasing the time interval between sequential PATH and SuperPATH cases. The absence of a control group is also a weakness of this study, and further studies are required to compare the outcomes of the PATH and SuperPATH approaches to those of more traditional approaches used in THA. Other limitations of this study include small sample size, lack of long-term follow-up, and lack of functional results.
In conclusion, the SuperPATH and PATH approaches can be successfully incorporated into a surgeon’s practice. Our early results reveal that these soft-tissue sparing THA approaches are associated with decreased overall complication rates, decreased LOS, and decreased inpatient rehabilitation. This surgeon’s learning curve demonstrated that operative time stabilized by case 40 for the PATH technique. In comparison, the SuperPATH technique was associated with shorter operative time that continued to decrease, suggesting that proficiency continues to improve beyond the first 50 cases. Despite the learning curve, the LOS and complication rates for the PATH and SuperPATH cohorts were both relatively low. The results published by innovators of the SuperPATH and PATH procedures are consistent with the results of the present study, which suggests that they are generalizable to surgeons adopting these techniques. However, further research with long-term outcomes is necessary.
Acknowledgements
Ranjeeta Mallick participated in analysis and interpretation of data. Richard Lee and Jonathan Peck contributed to the collection of data.
Footnote
Conflicts of Interest: W Gofton is an active consultant for Microport, receiving fees for technique training. The another author has no conflicts of interest to declare.
References
- Dorr LD, Maheshwari AV, Long WT, et al. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am 2007;89:1153-60. [PubMed]
- Bal BS, Haltom D, Aleto T, et al. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique. J Bone Joint Surg Am 2005;87:2432-8. [PubMed]
- Speranza A, Iorio R, Ferretti M, et al. A lateral minimal-incision technique in total hip replacement: a prospective, randomizes, controlled trial. Hip Int 2007;17:4-8. [PubMed]
- Paillard P. Hip replacement by a minimal anterior approach. Int Orthop 2007;31:S13-5. [PubMed]
- Chow J, Penenberg B, Murphy S. Modified micro-superior percutaneously-assisted total hip: early experiences & case reports. Curr Rev Musculoskelet Med 2011;4:146-50. [PubMed]
- Pagnano MW, Trousdale RT, Meneghini RM, et al. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty. A randomized clinical trial. J Bone Joint Surg Am 2008;90:1000-6. [PubMed]
- Mouilhade F, Matsoukis J, Oger P, et al. Component positioning in primary total hip replacement: a prospective comparative study of two anterolateral approaches, minimally invasive versus gluteus medius hemimyotomy. Orthop Traumatol Surg Res 2011;97:14-21. [PubMed]
- Foucher KC, Wimmer MA, Moisio KC, et al. Time course and extent of functional recovery during the first postoperative year after minimally invasive total hip arthroplasty with two different surgical approaches--a randomized controlled trial. J Biomech 2011;44:372-8. [PubMed]
- Fink B, Mittelstaedt A, Schulz MS, et al. Comparison of a minimally invasive posterior approach and the standard posterior approach for total hip arthroplasty A prospective and comparative study. J Orthop Surg Res 2010;5:46. [PubMed]
- Mayr E, Nogler M, Benedetti MG, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon) 2009;24:812-8. [PubMed]
- Procyk S. Initial results with a mini-posterior approach for total hip arthroplasty. Int Orthop 2007;31:S17-20. [PubMed]
- O'Brien DA, Rorabeck CH. The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Relat Res 2005.99-103. [PubMed]
- Ogonda L, Wilson R, Archbold P, et al. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am 2005;87:701-10. [PubMed]
- Penenberg BL, Bolling WS, Riley M. Percutaneously assisted total hip arthroplasty (PATH): a preliminary report. J Bone Joint Surg Am 2008;90:209-20. [PubMed]
- Murphy SB, Tannast M. Conventional vs minimally invasive total hip arthroplasty. A prospective study of rehabilitation and complications. Orthopade 2006;35:761-4, 766-8. [PubMed]
- Gofton W, Chow J, Olsen KD, et al. Thirty-day readmission rate and discharge status following total hip arthroplasty using the supercapsular percutaneously-assisted total hip surgical technique. Int Orthop 2015;39:847-51. [PubMed]
- Liaw CK, Hou SM, Yang RS, et al. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res 2006.134-9. [PubMed]
- Arora KS, Khan N, Abboudi H, et al. Learning curves for cardiothoracic and vascular surgical procedures - a systematic review. Postgrad Med 2015;127:202-14. [PubMed]
- Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J 2007;83:777-9. [PubMed]
- Tekkis PP, Senagore AJ, Delaney CP, et al. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 2005;242:83-91. [PubMed]
- Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60:217-20. [PubMed]
- Archbold HA, Mockford B, Molloy D, et al. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br 2006;88:883-6. [PubMed]


