Please sir, may I have some more? The case against underfeeding
In the critically ill patient, current recommendations endorse administering nutritional support according to indirect calorimetry measurements or if not available, according to formulae, such as 25 kcal/kg ideal body weight/day or other predictive equations (1,2). However, it is universally recognized that these equations are largely inaccurate and may result in both under- or over-feeding in 40-70% of patients. Over the past few years, numerous studies have compared outcomes of patient receiving by different routes, various amounts of calories and protein (3-5). One of the most recent, by Arabi et al. (6), namely the PermiT study, compared a standard caloric regimen consisting of 70-100% of estimated caloric requirements as determined by the Penn State equation, to a permissive underfeeding regimen consisting of 40-60% of caloric requirements. The study was an unblinded, randomized, controlled trial conducted in seven centers. In effect, however, both arms were underfed, i.e., the “planned” underfed group received 46% of daily requirements while the standard group received only 71% of daily requirements, what might be called the “unplanned” underfed group. Thus a large negative energy balance was likely incurred by both groups. In this regard, many observational studies have noted the association between negative energy balance and increased complications (7,8). In a recent editorial (9), we pointed out that underfeeding is the common denominator of most of recent studies examining the effects of nutritional support in critically ill patients, with the exception of the SPN study (3), the TICACOS study (10) and the EPaniC study (4). The ESPEN initiated Nutrition Day in ICU audit, as well as other large audits performed by the Canadian group (11), have confirmed the worldwide trend of underfeeding patients despite clear guidelines. This may be explained by the fact that while enteral feeding is encouraged, intestinal failure as well as technical difficulties are frequently encountered, limiting the ability to achieve caloric goals. Adding to the problem is the reluctance, especially in North America, to increase caloric intake by the use of total or supplemental parenteral nutrition in these circumstances. The strength of a large randomized, controlled study published in a prestigious journal should not let us forget that the best way to reach a scientific conclusion is to perform studies with actually achieved end-points. Thus we need to compare a nutritional regimen, prescribed and administered according to guidelines and which achieves both caloric goals, according to indirect calorimetry or the best predictive equation, and protein goals according to 1.5 g/kg/day, to a defined underfeeding regimen. Where this was performed, the truly underfed group had a worse outcome (12).
Recently, Kastrup and Spies (13) pointed out a general lack of adherence to guidelines. There is some confusion regarding the various requirements related to nutritional support. Table 1 shows the administered calories and protein intake in most of the studies comparing underfeeding to “standard therapy” demonstrating again the difficulties in reaching nutritional targets in daily practice.
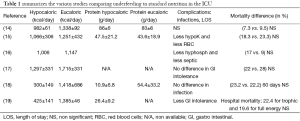
Full table.
To provide the best nutritional support, the practitioner should ask himself the following questions.
Whom to feed?
There is no information regarding the severity of malnutrition of the population of PermiT study. BMI is not accurate enough to evaluate the level of malnutrition and a decrease in weight prior to admission is the best currently available tool to evaluate the degree of malnutrition. Alberda et al. (20) showed in a large-scale nutrition adequacy database that there was an association between 6-month survival and health status in critically ill patients ventilated for more than 8 days. Receiving closer to target calorie prescriptions in the first week of ICU stay was associated with improved 6-month survival and improved health-related quality of life (21). In particular, severely malnourished patients should receive full nutritional support both earlier while avoiding underfeeding (22).
What are the best calorie and protein goals? Guidelines
The main limitation of the Arabi study is the use of predictive equations. In a recent review, 38% of the prescriptions using predictive equations underestimated energy needs when compared to measured energy expenditure obtained by indirect calorimetry (23). The use of the Harris Benedict formula yielded the worst results, underestimating 54% of the prescriptions, while the Penn State University equation used in the Arabi paper underestimated 27% of energy requirements. On the other hand this equation did not overestimate energy needs. The fact that all the studies cited in Table 1 comparing underfeeding to standard therapy used predictive equations and not indirect calorimetry is a limiting factor and their conclusions should be cautiously interpreted. It is important to note that the only studies showing an improvement in clinical outcome targeted the calorie intake using indirect calorimetry (3,5,10).
Protein intake appears to be of significant importance in influencing the outcome of ICU patients. Half of the studies in Table 1 administered a low protein intake which may in fact negatively affect outcome. Berg et al. (24) using stable isotopes methodology, demonstrated that a hypocaloric regimen is typically associated with a more negative protein balance, increasing the importance of ensuring a high protein intake even if underfeeding is planned. These findings were already demonstrated by Shaw and Elwyn (25). This was the case in the Arabi study where the planned underfed group received a higher percentage of protein compared to the standard group-might this account for the good outcome.
Route of feeding
While enteral feeding is the preferred route for providing nutritional support, it is not the only route. Insufficient enteral feeding is frequently observed and may be the result of delays in initiation, stopping the feeding due to mechanical problems or the need to perform diagnostic tests (e.g., CT scans outside the ICU) or failure to increase feeding according to the changing metabolic state of the patient. In addition surgical interventions, such as bowel surgery, are often cited as reasons for not initiating enteral nutrition while the presence of a large gastric residual volume frequently leads to a decision to either stop or decrease nutrient administration (26). In malnourished patients who are either not able to receive enteral feeding at all or in inadequate amounts, total or supplemental parenteral nutrition should be prescribed (1). In severely malnourished patients, there is an important need to feed the patient with PN if needed. This aspect is lacking in the studies cited in Table 1 in the control group, again demonstrating failure to follow the guidelines.
The results of the PermiT study should be cautiously interpreted. The conclusion states that “a strategy of enteral feeding to provide a moderate amount of calories to critically ill adults in the presence of full protein intake was not associated with lower mortality than a strategy aimed at providing a full amount of calories. ” The significant gap may develop between the intention to feed (e.g., strategy) and actually administered calories and studies should not assess strategies but in particular compliance with accepted protocols. Finally, authors planning studies focused on nutrition in the ICU should not aim for a reduction in ICU mortality as a primary outcome since nutrition may not be able to influence ICU mortality. Instead, long term outcome should be the primary parameter to be evaluated.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Singer P, Berger MM, Van den Berghe G, et al. ESPEN Guidelines on Parenteral Nutrition: intensive care. Clin Nutr 2009;28:387-400. [PubMed]
- McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2009;33:277-316. [PubMed]
- Heidegger CP, Berger MM, Graf S, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet 2013;381:385-93. [PubMed]
- Casaer MP, Mesotten D, Hermans G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med 2011;365:506-17. [PubMed]
- Weijs P J, Stapel SN, de Groot SD, et al. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: a prospective observational cohort study. JPEN J Parenter Enteral Nutr 2012;36:60-8. [PubMed]
- Arabi YM, Aldawood AS, Haddad SH, et al. Permissive Underfeeding or Standard Enteral Feeding in Critically Ill Adults. N Engl J Med 2015;372:2398-408. [PubMed]
- Villet S, Chiolero RL, Bollmann MD, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502-9. [PubMed]
- Dvir D, Cohen J, Singer P. Computerized energy balance and complications in critically ill patients: an observational study. Clin Nutr 2006;25:37-44. [PubMed]
- Singer P, Cohen J. Nutrition in the ICU: proof of the pudding is in the testing. Intensive care Med 2015;41:154-6. [PubMed]
- Singer P, Anbar R, Cohen J, et al. The Tight calorie control study (TICACOS); a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 2011;37:601-9. [PubMed]
- Cahill NE, Dhalial R, Day AG, et al. Nutrition therapy in the critical care setting; what is the best achievable’ practice? An international multicenter observational study. Crit Care Med 2010;38:395-401. [PubMed]
- Allingstrup MJ, Esmailzadeh N, Wilkens KA, et al. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin Nutr 2012;31:462-8. [PubMed]
- Kastrup M, Spies C. Less is more? Is permissive underfeeding in critically ill patients necessary? Am J Clin Nutr 2011;94:957-8. [PubMed]
- Charles EJ, Petroze RT, Metzger R, et al. Hypocaloric compared with eucaloric nutritional support and its effect on infection rates in a surgical intensive care unit: a randomized controlled trial. Am J Clin Nutr 2014;100:1337-43. [PubMed]
- Arabi YM, Tamim HM, Dhar GS, et al. Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr 2011;93:569-77. [PubMed]
- Owais AE, Kabir SI, Mcnaught C, et al. A single-blinded randomised clinical trial of permissive underfeeding in patients requiring parenteral nutrition. Clin Nutr 2014;33:997-1001. [PubMed]
- Desachy A, Clavel M, Vuagnat A, et al. Initial efficacy and tolerability of early enteral nutrition with immediate or gradual introduction in intubated patients. Intensive Care Med 2008;34:1054-9. [PubMed]
- Rice TW, Wheeler AP, Thompson BT, et al. Initial trophic vs full enteral feeding in patients with acute lung injury. JAMA 2012;307:795-803. [PubMed]
- Rice TW, Mogan S, Hays MA, et al. Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med 2011;39:967-74. [PubMed]
- Alberda C, Gramlich L, Jones N, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 2009;35:1728-37. [PubMed]
- Rubinson L, Diette GB, Song X, et al. Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit Care Med 2004;32:350-7. [PubMed]
- Weimann A, Singer P. Avoiding underfeeding in severely ill patients. Lancet 2013;381:1811. [PubMed]
- Tatucu-Babet OA, Ridley EJ, Tierney AC. The Prevalence of Underprescription or Overprescription of Energy Needs in Critically Ill Mechanically Ventilated Adults as Determined by Indirect Calorimetry: A Systematic Literature Review. JPEN J Parenter Enteral Nutr 2015. [Epub ahead of print]. [PubMed]
- Berg A, Rooyackers O, Bellander BM, et al. Whole body protein kinetics during hypocaloric and normalcaloric feeding in cirtically ill patients. Crit Care 2013;17:R158. [PubMed]
- Shaw SN, Elwyn DH, Askanazi J, et al. effectsof increasing nitrogen intake on nitrogen balance and energy expenditure in nutritionally depleted adult patients reiving parenteral nutrition. Am J Clin Nutr 1983;37:930-40. [PubMed]
- Kuslapuu M, Jõgela K, Starkopf J, et al. The reasons for insufficient enteral feeding in an intensive care unit: A prospective observational study. Intensive Crit Care Nurs 2015. [Epub ahead of print]. [PubMed]


